Chronic myeloid leukemia
(CML) is one of the types of leukemia with slow progression.
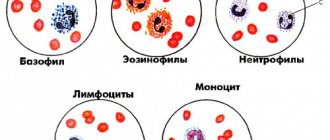
The cells formed during leukemia are immature and have a longer lifespan than mature (normal) leukocytes. As the disease progresses, immature cells accumulate in the bone marrow and enter the peripheral blood, displacing normal hematopoietic cells.
Men suffer from CML somewhat more often than women. The average age of patients is 30-70 years.
Causes of myeloid leukemia
The reasons for the development of CML is the exchange of sections of chromosomes 9 and 22. The new chromosome that forms in this case is called the Philadelphia or Ph+ chromosome. The Philadelphia chromosome was discovered in 1960 by Peter Nowell and David Hungerford in Philadelphia. It got its name from the place where the discoverers worked. The Philadelphia chromosome (Ph+) contains an abnormal gene called BCR-ABL. This gene is responsible for the formation of the abnormal protein BCR-ABL, which causes excessive production of abnormal white blood cells.
Who is at risk?
- Men.
- People over 60 years of age.
- People who smoke.
- People who have had radiation therapy or chemotherapy (this happens with other forms of cancer).
- People who have been exposed to radioactive radiation.
- People suffering from Down syndrome and other genetic disorders.
- People who suffer from myelodysplastic diseases (this is the name of a group of chronic diseases in which the bone marrow stops producing a sufficient number of full-fledged blood cells).
Symptoms of myeloid leukemia
Symptoms for this disease are not specific: weakness, loss of appetite, weight loss, sweating, fever, itchy skin, bone pain, fatigue, pale skin, tachycardia, bleeding with minimal abrasions and bruises.
When contacting a therapist with this complaint, the first thing you might think of is a viral disease (acute respiratory infection, ARVI, influenza, etc.). Only based on the results of a complete blood count (CBC), a blood disease can be suspected. The blood test must be deciphered by a specialist, because With viral diseases, there are also deviations in the results. If the therapist sees from the blood results that the changes are not characteristic of a viral disease, you will be referred for a consultation with a hematologist.
Treatment of chronic myeloid leukemia
At the initial stage, before obtaining cytogenetic confirmation of the diagnosis (as we already know, chronic myeloid leukemia is diagnosed in the presence of the Philadelphia chromosome), symptomatic therapy with hydroxyurea is prescribed. Its goal is to reduce the overall level of white blood cells and platelets. If there is intolerance to the drug or insufficient reduction in platelet levels, anagrelide can be used. If there are signs of leukostasis (encephalopathy, visual disturbances, renal dysfunction), leukapheresis is performed.
After cytogenetic confirmation of the diagnosis, specific antitumor therapy is prescribed. The main drugs are tyrosine kinase inhibitors (TKIs). The dosage is selected depending on the level of leukocytes. At the initial stage, to prevent tumor lysis syndrome, enhanced hydration is necessary (additional fluid administration in a volume of 2-2.5 l/m2, if there are no contraindications from the cardiovascular system) and the administration of allopurinol.
The goal of specific treatment for chronic myeloid leukemia is to suppress the tumor cell clone, reduce the risk of pathology progression and prolong the patient’s life to values comparable to general population indicators. With the introduction of TKIs into practice, these tasks became quite feasible and not only made it possible to increase the overall survival of such patients several times, but also to eliminate lifelong medication use and transfer to dynamic observation in patients with a good molecular tumor response.
Currently, according to accepted treatment protocols, TKIs should be prescribed to all patients with newly diagnosed chronic myeloid leukemia. Their mechanism of action is based on the blockade of the ATP-binding pocket of the pathological molecule BCR-ABL, which deprives this protein of tyrosine kinase activity, which stimulates excessive division of tumor cells. With constant use of TKIs, the tumor clone undergoes reduction, which makes it possible to restore normal hematopoiesis.
In Russia, the following drugs from the TKI group are registered for first-line therapy:
- imatinib,
- nilotinib,
- dasatinib.
Imatinib
Imatinib has selective activity against BCR-ABL tyrosine kinase and several other tyrosine kinases. It is prescribed in long courses and must be taken daily. The initial dosage is 400 mg per day for the chronic phase of myeloid leukemia, and 600 mg/day for the accelerated phase or blast crisis. The dosage does not depend on the patient’s height, gender and body weight. The drug is available in tablet form or capsules. Can be used on an outpatient basis. If the result of therapy is unsatisfactory, the dosage can be increased, and if toxic complications develop, it can be reduced.
Nilotinib
Nilotinib is a highly selective BCR-ABL tyrosine kinase inhibitor. It was developed based on the imatinib molecule and modified to increase affinity for BCR-ABL tyrosine kinase. Available in capsules. The dosage for chronic phase therapy is 600 mg/day, for acceleration phase therapy - 800 mg/day. The drug is taken 2 times a day with an interval of 12 hours strictly on an empty stomach, since food increases the bioavailability of the drug, which increases its concentration in plasma and can provoke the development of toxic complications. If the therapeutic effect in the treatment of the chronic phase is insufficient, the dosage may be increased to 800 mg/day. If complications develop, the dose is reduced.
Dasatinib
Dasatinib has activity against many tyrosine kinases, including mutant BCR-ABL. Penetrates the blood-brain barrier. Available in forms for oral use. The recommended dosage is 100 mg/day for the chronic phase and 140 mg/day for the accelerated phase and blast crisis. If chronic phase therapy is insufficiently effective, the dosage may be increased to 140 mg/day. If toxic complications develop, it is reduced to 80 mg/day.
Bosutinib
Bosutinib is a relatively new drug, registered in Russia in 2014 and is used for second and subsequent line therapy in cases of intolerance or ineffectiveness of the above drugs. The standard daily dose is 500 mg, which can be increased to 600 mg if necessary.
The choice of first-line drug is carried out individually for each patient. This takes into account the phase of leukemia, the sensitivity of the tumor clone with individual mutations, the toxicity profile of each drug and the presence of concomitant diseases in the patient.
Determination of the spectrum of mutations is carried out when the pathology manifests itself in the acceleration phase or blast crisis, or when therapy with the selected drug is ineffective and there is a need to change the drug, since there is a possibility of the emergence of resistant clones. For example, mutations F317L/V, T315A, V299L cause low sensitivity to dasatinib, so it is changed to nilotinib. Mutations Y253H, E255K/V, F359V/C, on the contrary, make tumor cells resistant to nilotinib, so dasatinib is indicated for such patients.
Mutations E255K/V, G250E, V299L cause resistance to bosutinib. The presence of the T3151 mutation determines resistance to all types of TKIs, so allogeneic hematopoietic stem cell transplantation is recommended for such patients. Ponatinib therapy is also a possible option, but it has not yet been registered in Russia.
The effect of first-line therapy can be classified into one of three groups:
- Optimal answer. This is a good result, which allows us to hope for a long period of disease-free survival (7-8 years or more). The criteria for achieving optimal response are complete hematologic response within 3 months, complete cytogenetic response within 6 months, and major molecular response within 12-18 months.
- Warning. In the presence of warning factors, careful monitoring of the patient's condition and readiness to change the treatment regimen are required. Prevention factors include a high-risk group for chronic myeloid leukemia, a more than 10-fold increase in the transcription level of the mutant gene, and the presence of additional chromosomal abnormalities in cells with the Philadelphia chromosome.
- Therapy failure. This includes the progression of the disease, the emergence of new mutations, and the appearance of additional chromosomal abnormalities in cells with the Philadelphia chromosome. A change in therapy is required.
Other treatments for chronic myeloid leukemia
Donor stem cell transplantation is indicated for patients who have failed second-line therapy and for patients with the T315I mutation. Patients intolerant of TKIs and unable to undergo transplantation can be treated with hydroxyurea, interferons and cytostatics.
Diet
Diet for leukemia (blood cancer)
- Efficacy: no data
- Duration: until recovery/lifelong
- Cost of products: 3000-4600 rubles. in Week
During the treatment period, it is important to adhere to recommendations regarding proper nutrition. A proper diet with sufficient content of substances important for the body will contribute to the effectiveness of treatment of the disease. During the treatment of myeloid leukemia, it is very important to prevent deficiency of iron, cobalt, copper, manganese, nickel, and vitamin C. All these components are important for the restoration of blood cells, as well as for maintaining the optimal general condition of the patient. The following products should be included in the diet:
- protein foods - sea fish and seafood, rabbit and poultry meat, egg yolks, offal, dairy products;
- vegetables - greens, peppers, cabbage, legumes, carrots, pumpkin, corn, zucchini;
- fruits - citrus fruits, pears, berries, apples, plums, peaches, apricots, sea buckthorn;
- cereals;
- bran bread;
- honey.
It is recommended to exclude from the diet:
- lamb and beef, which contain refractory fat;
- coffee, tea and other products containing caffeine;
- products with vinegar - canned food, etc.;
- alcohol;
- hot spices.
It is recommended to reduce the amount of fat consumed.
Diagnostic methods for CML
To ensure a qualified and effective treatment process at the Hadassah MC, the most modern diagnostic techniques are used to examine patients, the basis of which is molecular biology and immunofluorescence. Data from such studies make it possible to establish pathological changes and accurately confirm the diagnosis.
Diagnostics consists of:
1)
From a detailed analysis of venous blood, which allows you to determine or refute the presence of blast cells (signs of a malignant disease).
2)
The use of a puncture biopsy of the hematopoietic organ makes it possible to diagnose the type and stage of myeloid leukemia.
3)
To obtain a complete picture of the disease and to plan an appropriate treatment program, a genetic analysis is prescribed to identify chromosomal aberrations that confirm the probable cause of the myeloid leukemic nature of the disease.
General diagnostics includes consultations with various specialists, on whose recommendation additional diagnostics may be prescribed, including:
x-ray examination;
bone scan – scintigraphy
multi-inlet arteriography, to determine changes in the functions of the cardiac ventricles.
List of sources
- Abdulkadyrov K.M., Bessmeltsev S.S., Rukavitsyn O.A. Chronic myeloid leukemia. – St. Petersburg: “Special Literature”, 1998.- 464 p.
- Quality of life of patients with chronic myeloid leukemia / M. I. Savelyeva, I. N. Samarina, O. S. Samoilova, etc. // Kremlin. medicine. Wedge. Vestn. – 2012. – No. 1. – P. 60-64.
- Savva N.N. Innovative approaches to the treatment of chronic myeloid leukemia in children / N.N. Savva // Republican Scientific and Practical Center of Pediatric Oncology and Hematology of the Ministry of Health of the Republic of Belarus. Medical news. - 2010. - No. 5-6. — P.12-17.
- Smirnova, O. V. Chronic myeloid leukemia - clinical and immunological features in adult patients / O. V. Smirnova // Acta Biomedica Scientifica. – 2012. – No. 3-2. – pp. 185-189.