The heart works, the heart does not sleep
Heart... An organ surrounded by a romantic halo, awarded the attention of writers, musicians, poets... The heart is a unique symbol of love; we associate our feelings and emotions with it. If you descend from heaven to the “sinful” earth and briefly and prosaically define what a heart is, you will get something like this: “the heart is a strong muscular pump capable of pumping blood throughout the body to provide tissues with oxygen.” It would seem like just a pump, but what a pump! Able to work without sleep or rest for years, decades; capable, if necessary, of instantly changing the operating mode. And all this thanks to its amazing structure - muscle, valves, its own circulatory system, innervation and many ingenious mechanisms of regulation and compensation both inside and outside the heart.
Implantation of resynchronization devices
Before implantation:
- Before scheduling your procedure, tell your doctor if you are taking anticoagulants such as warfarin (Coumarin, Pradaxa, Xarelto, Eliquis). Find out when you can continue taking these medications.
- Do not eat or drink the night before implantation. On the morning of the procedure, take only the medications your doctor recommends.
Implantation procedure:
Resynchronizing pacemakers, or cardioverter defibrillators, are surgically implanted into the body. Before surgery, your breasts should be washed clean with antibacterial soap. An intravenous catheter will be placed in your arm to administer any necessary medications during surgery. Your relatives may be in the room during the operation. Most of these operations are performed under local anesthesia. If necessary, you will be given a sedative medication to help you relax before the operation. The operation is performed in an operating room equipped with an X-ray machine. An incision is usually made in the upper chest, and then electrodes are inserted through the veins. An X-ray machine helps the doctor guide electrodes through the veins and place them in the heart. (Sometimes these devices are implanted during open-heart surgery. In these cases, the leads are placed epicardially, on the outer surface of the heart.) The electrodes are checked before connecting to the stimulator. The doctor then makes a bed for the device under the skin (usually in the upper part of the chest). (If implantation is carried out during heart surgery, the stimulator is installed in the abdomen). If you have been implanted with a defibrillator, an electrical shock will be sent to your heart to induce tachycardia to test its functionality. During this test you will be under general anesthesia and will not feel anything.
After implantation
Typically, after the device is implanted, you will spend the night in the clinic. If you experience pain in the incision area, you may require pain medication. Do not raise your arm on the side where the device is implanted, as this may cause the electrodes to become dislodged. Your doctor will tell you when you can get out of bed. While you are in the clinic, continuous monitoring will be carried out to monitor the operation of the stimulator and the correct position of the electrodes. When you are cleared to get out of bed, you will have a chest x-ray. During the x-ray, the doctor may ask you to raise your hands. Do not raise your hands during the actual photo. Tell the radiologist that you have a pacemaker or defibrillator and that you should not raise your arms. In the future, it will be possible to configure or reprogram the device according to your needs. If there is a need to change the settings of your device, this can be done at any time after the operation. Reprogramming will not harm you or your device. After discharge from the clinic, you will receive an identification card confirming that you have an pacemaker or ICD. Carry this card with you at all times. You and your family will need to remember the manufacturer of your device. If you have an identification bracelet, add information about your device to it.
Medical care after implantation
This chapter contains information that will help you make the recovery period after surgery more comfortable and faster.
The impact of general anesthesia on your activities
During the operation, you may be given intravenous sedatives or general anesthesia. In the first 24 hours, slow reactions and impaired consciousness may occur. That's why:
- if you are sent home on the same day, then make sure that someone looks after you on the first day;
- do not drive a car; if you are allowed to go home after the procedure, make sure that someone takes you;
- try to rest more during the first day;
- you should not return to work or school on the first day;
- do not ride a bicycle or rollerblade;
- do not take responsibility for small children or anyone who will depend on your help;
- Avoid rough play and participation in sports;
- do not drink alcoholic beverages;
- limit yourself in making serious decisions and working with important documents.
Water will not harm your device, but you may not shower or bathe until 48 hours after implantation. If you have an adhesive plaster stuck to your wound, then if it gets wet it will become unusable. You can remove the adhesive plaster 2 weeks after surgery or as directed by your doctor. You may experience discomfort and pain in the incision area. Bruising may also occur in this area. These extraneous sensations will pass after some time (they are not pathological and can occur after any surgical intervention). To relieve pain and discomfort, you can take painkillers that do not contain aspirin in doses recommended by your doctor. Until you are instructed by your healthcare provider, do not take pain relievers containing aspirin, ibuprofen, or naproxen on your own. These drugs reduce blood clotting, thereby increasing the risk of bleeding. Talk to your doctor before taking or buying a new drug. You may experience redness and swelling in the incision area for several weeks. In people taking anticoagulants, these phenomena are usually more pronounced. Once the swelling subsides, you will be able to see the outline of your device.
Monitoring the resynchronization device
Before you are discharged from the hospital, a plan will be made for your future doctor visits (usually about 3 months after surgery). During each inspection, your device will be checked and reprogrammed if necessary. Your device should be checked regularly. If you have had a pacemaker implanted, this can be done over the phone. You will be given special instructions to follow after discharge. The remote monitoring system will allow your doctor to monitor the performance of the device and battery charge. As a rule, for the first 4 weeks you will perform transmissions to transfer data to the doctor, then once every 3 months or more often (if the battery begins to discharge). If you have had a pacemaker/defibrillator implanted, you will need to see your doctor regularly. Guaranteeing the functionality of the device requires your regular monitoring. Examinations will be carried out during the first month after surgery and then every 3 or 6 months, or more often (for example, before reimplantation). During each inspection, the functionality of the device will be checked. Your doctor will check to see if there are any changes in the way your stimulator works since your previous visit and relate them to your symptoms. The battery life will also be checked. Depending on the situation, the examination can be carried out in a hospital or on an outpatient basis. It can last up to 4 hours and necessarily includes testing the shock discharge function of the device. If you will have general anesthesia, follow the recommendations listed in the “Activities after anesthesia” section.
Reimplantation of a resynchronization device
Your device will not stop working suddenly. The battery charge will decrease gradually. To determine when the device will need to be reimplanted, the battery charge will be checked at each inspection. During reimplantation, the old device will be removed and a new one will be installed in its place. Reimplantation is usually performed as an outpatient procedure. From the moment you receive intravenous and/or general anesthesia, follow the recommendations listed in the section “Activities after anesthesia.” During surgery, the electrodes and the new device will be tested. If necessary, the electrodes will be repositioned or replaced (in this case, you will need to stay in the clinic overnight). You will need to follow the same physical activity restrictions as you did with your initial implantation. After reimplantation, you may feel pain in the incision area, which will subside over time.
How will the device operate?
If your device only works to synchronize the contractions of the ventricles, you will not feel the electrical impulses. If you were implanted with a cardioverter-defibrillator to correct attacks of tachycardia, then during operation of the device you will feel an electrical discharge, which may cause you discomfort. You may feel chest pain, slight palpitations, or nothing at all. However, these sensations will be short-lived and harmless and will not be similar to external defibrillation that you may have previously had. If your tachycardia attack was stopped on your own, then you will not feel an electrical discharge, but you may feel dizziness and a temporary deterioration in your general condition. In some people, this electrical discharge appears as a single muscle contraction.
If you feel an electric shock
If you feel weak or dizzy, you need to sit or lie down immediately. You may have an abnormal heart rhythm. It may take from 5 to 10 seconds. before your device sends an electrical impulse to the heart. These symptoms usually go away once the device starts operating.
In this case, follow these recommendations:
- If you feel a single electrical shock and then improve, you can call your doctor, but this is not necessary;
- If you feel two or more electrical shocks, the device is damaged, or you receive an electrical shock from a device or electrical outlet, be sure to contact your doctor;
- If you feel more than two electrical shocks and/or do not feel any improvement, ask someone near you to help you call emergency services. When emergency personnel arrive, they will need to be alerted to the device.
Qualified medical personnel use external defibrillation if necessary. When you arrive at the medical facility, you will undergo a full examination. If your heart rate is normal, you can return home. If a heart rhythm disorder or other illness is detected, you will have to stay in the clinic for further examination and observation.
The heart is a “fiery motor”!
Normally, the heart is a strong muscular pump capable of pumping blood throughout the body to provide oxygen and nutrients to all organs and tissues of the body, as well as remove their waste products. Depending on whether we are resting or actively working, the body requires different amounts of nutrients. To meet the needs of the body, the frequency and strength of heart contractions, as well as the size of the lumen of blood vessels, can vary significantly. What happens when the heart stops sufficiently supplying tissues and organs with oxygen and nutrients? In this case, doctors diagnose heart failure (HF). The disease is usually chronic and the patient may live with it for many years before being diagnosed.
Treating Heart Failure Symptoms
Treatment of chronic heart failure takes a lot of time, and many drugs (diuretics, glycosides, inhibitors, beta blockers) are prescribed to the patient for life. Basically, the action of the drugs is aimed at relieving the symptoms of the disease and making life easier for the patient. In particular, shortness of breath in heart failure is treated, swelling of the extremities is relieved, and blood pressure is normalized.
In acute cases of the disease, in addition to medications, surgical methods are used. The goal of treatment is to eliminate the causes that led to the disease: narrowing of the coronary artery, consequences of myocardial infarction. In case of severe pathological changes in cardiac tissue, a defibrillator is implanted in the patient.
“Glitches”, “coughs”, “sneezes”... Who is to blame?
There are many reasons for the development of heart failure. Among them, the most important place is occupied by coronary heart disease or insufficient blood supply to the heart muscle. Ischemia, in turn, is caused by blockage of the heart vessels with fat-like substances. A heart attack can also cause heart failure because some of the heart tissue dies and becomes scarred. Arterial hypertension is another common cause of insufficiency. The heart requires much more effort to move blood through the spasmodic vessels, which results in an increase in its size, in particular the left ventricle. Later, weakness of the heart muscle or heart failure develops. Causes that influence the development of heart failure include cardiac arrhythmias (irregular contractions). A number of beats of more than 140 per minute is considered dangerous for the development of the disease, because At the same time, the processes of filling and ejection of blood by the heart are disrupted. Changes in the heart valves lead to disturbances in the filling of the heart with blood and can also cause the development of heart failure. The problem is usually caused by an internal infection (endocarditis) or a rheumatic disease. Risk factors for the development of diseases of the cardiovascular system, and, ultimately, heart failure, can also include excess weight, a sedentary lifestyle, alcohol and drug addiction, and hormonal disorders.
Qualified care for heart failure at the CBCP clinic
At the slightest suspicion of this disease, undergo diagnostics of the functioning of the heart and blood vessels. Modern diagnostic methods make it possible to determine the true cause of the disease in order to promptly block its further development.
The CBCP clinic has the latest expert-class equipment for diagnosing all types of this disease. Experienced, qualified cardiologists will advise you and give recommendations on how to treat heart failure.
Make an appointment right now on the website or during business hours by phone.
Listen to your heart
Thus, heart failure is not an independent disease, but a stage of heart disease. Its severity and speed of development can vary and depend on the severity of the primary heart disease, the patient’s lifestyle, his age, concomitant diseases and, finally, on the quality of treatment. Heart failure is manifested by such symptoms as increased fatigue, swelling of the legs, shortness of breath, asthma attacks, causeless weight loss, etc. Any of these symptoms, especially taken individually, can occur in a variety of diseases. Therefore, the correct diagnosis is made, unfortunately, rarely and most often in the later stages of the disease. Thus, significant weight loss, which is typical for severe degrees of heart failure, is often mistaken for a sign of cancer. Or, for example, harmless swelling of the legs caused by stagnation of lymph gives rise to a diagnosis of “heart failure.” In my practice, there was a case when a patient with a severe form of heart failure was treated for several months for... constipation.
Degrees of chronic pathology
There are several degrees of chronic heart failure. The earlier a problem is identified, the easier it is to treat. In the later stages of the disease, mortality is 50%.
The first stage of chronic insufficiency is characterized by shortness of breath and rapid fatigue after active physical work or sports. Treatment at this time is most effective. Early detection of symptoms of chronic deficiency will not only help to cope with it, but also to determine the true cause.
In the second stage of heart failure, symptoms become more pronounced:
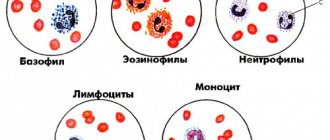
- cyanosis, or blue discoloration of the fingertips, nose and nasolabial folds, lips. The reason is a change in blood composition, insufficient oxygen content.
- With low-intensity loads, typical symptoms appear: shortness of breath, rapid heartbeat, weakness.
- Dry cough not associated with a cold.
The second stage is characterized by damage to the pulmonary circulation, the lungs suffer, so a cough occurs, and the blood is poorly saturated with oxygen.
Another variant of the manifestation of the second stage is damage to the systemic circulation. First of all, swelling appears. They can be hidden: fluid accumulates in body cavities, for example, filling the abdominal cavity. Swelling of the legs is more noticeable. This condition is called dropsy.
In addition, stagnation begins in all organs: liver, kidneys, digestive system, brain. Associated pathologies develop and the functioning of these organs is disrupted.
At the third stage, irreversible changes occur. Usually the functioning of the entire circulatory system is disrupted. Lesion of the small circle is characterized by a strong cough with sputum production, the appearance of pink foam not only when coughing, but also at rest. This is explained by a violation of the permeability of numerous vessels, lymphatic fluid fills the lungs, and edema occurs. The condition is fatal and requires urgent hospitalization. Shortness of breath accompanies a person at rest. Worsens when lying down. Periodically there are attacks of suffocation, accompanied by fear of death. They force the patient into a sitting position with his legs down.
At the same time, all vital organs suffer. Signs of congestive liver damage:
- increase in organ volume;
- formation of sclerotic and connective tissue;
- cirrhosis of the liver.
Congestive kidney damage leads to chronic renal failure. At the same time, the amount of urine excreted decreases, swelling increases and no longer goes away under the influence of medications. Intestinal dysfunction occurs, constipation or diarrhea is possible.
The third stage is irreversible. A person completely loses the ability to be active. Even household chores become beyond his power. Usually the patient is assigned a certain form of disability. The survival rate in this case is 50%. Medicine in this case can only offer supportive therapy.
Important! The third stage of the formation of congestive heart failure occurs as a result of the lack of treatment for the disease. If you consult a doctor in a timely manner in the early stages, you can not only stop the progression of the disease, but also be completely cured.
If you notice the following signs of heart failure, you should immediately contact a cardiologist:
- Shortness of breath with minor physical exertion;
- Blueness of fingers, lips, nose;
- Unreasonable dry cough, sometimes accompanied by sputum production;
- Pain in the chest, under the shoulder blade;
- Swelling of the legs, enlargement of the abdomen, which may be hidden edema.
Mild heart failure responds well to treatment, so a preventive examination by a therapist and cardiologist and the necessary diagnostic methods will help avoid serious consequences.
Sad facts
Meanwhile, the prognosis for heart failure is unfavorable, if not fatal. When some primary symptoms of the disease (for example, pulmonary edema) appear, there is immediately a threat of death. These statistics are disappointing - within 3-5 years, 50% of patients die from heart failure, and after 9 years only 0.2% remain alive, of course, provided that the disease was not treated appropriately. Conventional drug treatment can only keep such patients alive in a state of severe disability with frequent hospitalizations. Of course, there is a radical way to help them - transplant a new heart. However, significant limitations for this intervention (age limit, high cost of surgery, lack of a sufficient number of donor hearts) make it unrealistic for the majority of heart failure sufferers. Now they have begun to talk about a new, promising method of restoring decrepit heart muscle, based on planting so-called “stem” cells. But, unfortunately, for practical use this is a matter of a rather distant future.
Functional classes of heart failure
- First . The patient is physically active and does not feel obvious signs of the disease.
- Second . The patient experiences well at rest, but physical activity causes symptoms of the disease to appear.
- Third . The patient is comfortable at rest, but much less physical activity is required for signs of the disease to appear.
- Fourth . Already at rest the patient feels discomfort, and with minimal exertion the symptoms increase sharply.
... and the other side of the coin
At the same time, in recent years, the development of medical science and pharmacology, in a successful combination with medical experience, has made it possible to achieve amazing success in the treatment of even the most severe forms of heart failure. Patients manage not only to save life, but also to regain its quality, an active lifestyle, and regain weight (and this after losing 20-30 kg!). Moreover, all treatment takes place on an outpatient basis, without hospital stay. Having worked for decades in a cardiac surgery center where there was a heart transplant department, I, along with other doctors, was a powerless witness to the death of patients after many months of fruitless waiting for donor hearts. How many of them could be saved thanks to today's knowledge, capabilities and experience!
According to the feat and the reward...
Angioplasty and stenting of arteries
- Cost: 100,000 - 250,000 rubles.
- Duration: 40 minutes
- Hospitalization: 1-2 days in hospital
More details
I will not hide that the treatment of such patients, in addition to experience, requires considerable effort and time from the doctor and great pedantry in carrying out the patient’s prescriptions. However, it would be too arrogant to attribute all the successes in the treatment of heart failure only to yourself, as the attending physician. The ability to quickly and accurately diagnose the underlying disease that caused heart failure has a huge role. In 50% of cases, this is coronary heart disease, the identification and treatment of which with coronary angiography and angioplasty greatly facilitates the subsequent correction of myocardial weakness. Equally important for successful treatment is the identification of the earliest, so-called “preclinical” (i.e., before the onset of complaints) forms of heart failure, which is only possible with the use of instrumental research methods: echocardiography, Holter monitoring, stress tests. The Center for Endosurgery and Lithotripsy has not only the most modern equipment, but also highly qualified specialists, which is necessary for the detection and timely treatment of heart failure. All these conditions help to successfully achieve the task of long-term preservation of active life in one of the most severe categories of patients with heart disease - patients with heart failure. But the reward is high: over the past 5 years, there has not been a single death among my 187 patients with heart failure!
4.Diagnosis of the disease
A special test called ejection fraction (EF) . It helps determine how well the heart pumps blood with each beat and can be used to diagnose both systolic and diastolic dysfunction. Ejection fraction as a percentage measures the amount of blood pumped with each beat.
In patients with systolic heart failure, the ejection fraction is less than 40%. Other diagnostic tests such as an echocardiogram or cardiac ultrasound can show how the heart is dilating and not pumping out enough blood with each beat.
Patients with diastylic heart failure have a normal ejection fraction test and their heart is pumping well, but an echocardiogram will show that the heart is not filling sufficiently during the relaxation phase that occurs between beats.
For timely diagnosis of heart failure, it is recommended to consult a cardiologist and periodically undergo a comprehensive cardiac examination.