Chronic heart failure (CHF) is a disease characterized by the inability of the heart to pump a certain volume of blood sufficient to provide the body with oxygen. CHF can be caused by many diseases of the cardiovascular system, the most common of which include coronary heart disease, hypertension, endocarditis and rheumatoid heart defects. Weakening of the heart muscle leads to the impossibility of normal pumping of blood, as a result of which the amount of blood released into the vessels gradually decreases.
The development of heart failure occurs gradually; in the early stages, the disease can manifest itself only during physical exertion, then it begins to be felt at rest.
The appearance of characteristic symptoms at rest indicates that the disease has entered a severe stage. The progression of chronic heart failure threatens a significant deterioration of the patient’s condition, a decrease in his working capacity and even disability. The development of chronic liver and kidney failure, blood clots, and strokes may occur.
Conducting timely comprehensive diagnostics and competent treatment ensures a slowdown in the development of CHF and the prevention of dangerous complications of this serious disease.
In order to stabilize the condition, a patient diagnosed with “acute and chronic heart failure” must adhere to the correct lifestyle: normalize his weight, follow a low-salt diet, limit physical and emotional stress.
Chronic heart failure: classification
Chronic heart failure develops gradually, passing through certain stages.
Chronic heart failure - stages with characteristic symptoms:
- the first stage – the patient has no restrictions on physical activity: during normal exercise, weakness (lightheadedness), palpitations, shortness of breath or anginal pain does not occur;
- second stage - physical activity is moderately limited: the patient is in a comfortable state at rest, ordinary physical activity can provoke the appearance of weakness (lightheadedness), palpitations, shortness of breath or anginal pain;
- third stage – physical activity is expressed and limited: the patient’s comfortable state is observed exclusively at rest. When performing physical activity, weakness (lightheadedness), palpitations, shortness of breath or anginal pain appears;
- in the fourth degree of chronic heart failure, performing any exercise is invariably accompanied by discomfort. Chronic heart failure syndrome also appears at rest. Even with minimal loads, discomfort increases.
CHF classification includes various types of disease, subdivided depending on the form (acute and chronic heart failure), localization (left ventricular, right ventricular and mixed heart failure), origin (myocardial, overload or combined chronic heart failure). The tables used by the attending physician provide all the information about the disease, its stages and characteristic symptoms.
Diagnosis and treatment
The main purpose of the examination is to identify the disease that caused pulmonary heart failure. As part of the diagnosis, the following is prescribed:
- consultations with a pulmonologist and cardiologist;
- chest x-ray;
- study of external respiration function (RPF) - spirometry, pneumotachometry, gas analytical study of external respiration;
- electrocardiography, echocardiography;
- right heart catheterization;
- Ultrasound of the heart;
- if pulmonary embolism is suspected, pulmonary angiography and ventilation-perfusion scintigraphy of the lungs are performed.
Pulmonary heart failure is eliminated with the help of oxygen therapy and medications. It is possible to perform operations - balloon atrial septostomy, sympathectomy, lung tissue reduction, lung transplantation. In acute pulmonary heart failure caused by pulmonary embolism, thromboembolectomy is indicated.
The reception is being conducted
General practitioner, family doctor, cardiologist, doctor of the highest category
Malashkina Irina Borisovna
Make an appointment
Your message has been sent
Thank you for contacting Multidisciplinary Medical!
Your message will be processed shortly and we will contact you to clarify the details.
Be healthy!
Join us on social networks!
Current news, promotions, useful information.
How to find us
OUR ADDRESS
Moscow, st. Shchukinskaya, 2
Shchukinskaya, Streshnevo, Sokol
TELEPHONE
+7
Chronic heart failure: pathogenesis
The main causes of chronic heart failure: damage to the heart muscle or impairment of its ability to pump the required amount of blood through the vessels, which can occur in patients suffering from the following pathologies:
- arterial hypertension – high blood pressure;
- IHD (coronary heart disease);
- heart defects.
The development of CHF in women is most often caused by arterial hypertension. In men, chronic heart failure usually occurs as a consequence of coronary heart disease.
In addition, chronic heart failure can develop due to the presence of the following diseases and dependencies:
- diabetes mellitus;
- arrhythmias (heart rhythm disturbances);
- cardiomyopathies;
- myocarditis;
- alcoholism and smoking.
Causes
Factors stimulating the development of pulmonary heart failure are persistent pulmonary hypertension and hypertrophy. As a result of increased pressure in the pulmonary artery, the hypertrophied right ventricle can no longer cope with pumping the venous blood entering it. The disease can develop as:
- complication of obstructive bronchitis, bronchiectasis, bronchial asthma, pneumonia;
- a consequence of damage to the pulmonary vascular bed that occurred due to thromboembolism, compression of the pulmonary veins and arteries by tumor formations;
- the result of conditions accompanied by limited mobility of the chest and diaphragm: chest deformation, spinal diseases, rib fractures, myasthenia gravis, polio, botulism, paresis and paralysis of the diaphragm.
CHF: symptoms
The clinical picture of CHF is quite diverse and depends on the severity and duration of its course. The disease develops slowly over several years. Lack of treatment threatens serious deterioration of the patient's condition.
Most often, chronic heart failure is manifested by the following symptoms:
- shortness of breath during physical exertion, when the patient moves to a supine position, and later at rest;
- dizziness, fatigue and weakness;
- nausea and lack of appetite;
- swelling of the lower extremities;
- development of ascites (accumulation of fluid in the abdominal cavity);
- weight gain due to swelling;
- fast or irregular heartbeat;
- dry cough with pinkish sputum;
- decreased intelligence and attention.
Chronic heart failure: risk group
The following risk factors, or at least one of them, can provoke the development of CHF. When several factors are combined, the likelihood of chronic heart failure increases significantly.
The risk group for the development of CHF includes patients suffering from the following diseases:
- cardiac ischemia;
- history of myocardial infarction;
- high blood pressure;
- heart rhythm disturbance;
- diabetes;
- Congenital heart defect;
- frequent viral diseases;
- chronic renal failure;
- alcohol addiction.
Detection methods
Since symptoms of cardiopulmonary failure may indicate a number of other diseases, cardiologists, to determine an accurate diagnosis, carry out a number of necessary measures, which include:
- Study of patient complaints.
- X-ray examination of the lungs, which allows you to determine changes in the pulmonary system and the size of the heart.
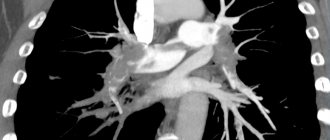
- If the previous study did not lead to an accurate diagnosis, an additional CT scan of the chest is performed.
- An ultrasound is required to determine the extent of heart damage.
- To determine the pressure in the lungs and heart, invasive manometry and catheterization are performed.
- In advanced cases, it is necessary to conduct an ECG, which will show the degree of changes in the organs.
Pregnancy with chronic heart failure: disease progression
The body of a pregnant woman has to overcome quite serious loads, including on the heart. Due to intrauterine growth and fetal development, the heart muscle must cope with the circulation of increased blood volume.
In women suffering from certain cardiovascular diseases, this heart function is often impaired, which leads to the development of CHF. The degrees of heart failure manifest themselves in different ways, but if even the slightest discomfort occurs, pregnant women should immediately inform their doctor.
Symptoms and signs
The main symptoms that determine exertional angina are attacks of heaviness in the chest, as well as burning or squeezing pain. These sensations can occur when a person is running, working out in the gym, or even just walking up the stairs.
The pain goes away if the load stops or the person takes Nitroglycerin in the form of a tablet/spray. This point is very important, it distinguishes more dangerous conditions - heart attack and unstable form of angina from this disease, since in them the pain is not relieved by Nitroglycerin.
Angina pain is characterized by specific irradiation - return to other parts of the body. This is mainly the lower jaw, neck, left arm and shoulder blade, and upper abdomen. Moreover, the place where the pain is applied is often felt much more strongly, and discomfort in the heart may go unnoticed. I often met patients who for a long time mistook attacks of angina for toothache and unsuccessfully underwent treatment for “pulpitis” or “periodontitis” at the dentist.
In addition to physical work, pain can “overtake” a person under other circumstances. Depending on the factor provoking a painful attack, the following clinical forms of angina pectoris are distinguished:
- Early morning - exacerbation appears at approximately 5-6 o'clock in the morning. Associated with increased blood viscosity and an increase in the amount of cortisol and adrenaline. They cause increased heart rate and hypertension.
- Angina after eating - a large meal redistributes blood flow in favor of the digestive organs. As a result, the oxygen supply to the heart deteriorates.
- Supine angina - when a person lies down, the volume load on his heart increases, which provokes increased work of the organ and, as a result, an increase in its need for oxygenation.
- Cold - at low ambient temperatures, the superficial blood vessels of the skin narrow, which forces the heart to work harder.
- Tobacco – components of cigarette smoke, including nicotine, increase heart rate, constrict blood vessels and thicken the blood.
- Angina after stress – stress stimulates the release of adrenaline and cortisol into the blood.
- Static – when a person bends over to, for example, put on shoes, pressure increases inside the chest. This, in turn, increases the volume load on the heart in the same way as supine angina occurs.
In some groups of patients, the clinical course of angina has its own characteristics. These include:
- elderly people - approximately 50% of people over 65 years of age experience not pain, but sudden difficulty breathing (shortness of breath);
- women - in females, due to the predominance of the emotional component during an attack, in addition to the pain associated with angina pectoris, neurotic pain develops as a result of vasospasm. I often have to accept female patients in whom it is difficult to determine the severity of angina pectoris only by symptoms and to distinguish it from other forms of ischemia;
- diabetics – due to the long course of diabetes mellitus, nerve endings are damaged, including those that conduct pain impulses. Therefore, I often meet such patients with hidden or asymptomatic angina.
Diagnosis of chronic heart failure
When diagnosing CHF, doctors at the Yusupov Hospital take into account medical history, characteristic symptoms and the results of a physical examination, instrumental and laboratory tests.
Laboratory tests include the following tests:
- General blood test - as a rule, there are no changes. Sometimes the presence of moderate anemia is determined;
- ESR (erythrocyte sedimentation rate) - an increase in ESR is observed with rheumatic heart disease or infective endocarditis, which resulted in the development of heart failure;
- general urinalysis - performed to diagnose kidney complications and exclude the renal origin of edema. The most common possible manifestation of CHF is an increase in protein levels in the urine;
- study of total protein and protein fractions - in CHF their indicators decrease, which is associated with redistribution into the edematous fluid;
- blood glucose level – important in order to exclude such a risk factor for CHF as diabetes mellitus;
- indicators of cholesterol, low and high density lipoproteins - a clear relationship has been proven between high cholesterol levels and atherosclerosis, hypertension, coronary heart disease; Elevated levels of lipoproteins and cholesterol in CHF may indicate a more severe course of the disease;
- the level of sodium and potassium in the blood - edema that occurs in patients with CHF is the cause of a significant decrease in the level of these microelements. Monitoring blood composition is especially important when taking diuretic drugs, as well as in cases where the patient has chronic heart and kidney failure;
- study of the level of brain natriuretic propeptide, a protein whose formation in the heart muscle is associated with its excessive stretching and overload. Its circulation in the blood is quite long, so laboratory testing can easily determine its level. With increasing cardiac overload, the secretion of propeptide is activated. Therefore, its indicators are important for determining the severity of CHF.
Additionally, instrumental studies are prescribed, the scope of which is determined by the attending physician:
- plain chest x-ray - to assess the position and size of the heart, exclude or confirm concomitant changes in the lungs (if the patient is suspected of chronic pulmonary heart failure);
- electrocardiography (ECG) - to determine heart rhythm disturbances and the consequences of a previous myocardial infarction;
- echocardiography - to differentiate systolic and diastolic heart failure, assess the activity of all parts of the heart, its size, the thickness of the heart muscle and its valves;
- stress tests – allow you to study the reaction of the heart muscle to increased physical activity;
- coronary angiocardiography - the essence of this x-ray study is the introduction of a special contrast agent through a catheter directly into the vessels of the heart, thanks to which it is possible to diagnose coronary heart disease;
- transesophageal echocardiography - ultrasound examination of the heart with placement of a sensor in the esophagus. Can be used if conventional cardiography does not provide a sufficiently clear image, and also helps to identify blood clots in the right atrium in patients with atrial fibrillation;
- stress echocardiography - ultrasound examination of the heart at rest and after exercise or after the use of medications with an effect similar to exercise. The study allows you to assess the reserve capabilities of the heart and identify areas of viable heart muscle;
- spiral computed tomography - during the procedure, X-rays are taken at different depths, which, in combination with MRI, provides an accurate image of the heart;
- endomyocardial biopsy - during the diagnostic procedure, tissues of the muscle and inner lining of the heart are taken for histological examination, which makes it possible to clarify the cause of the disease in complex cases.
In addition, patients at the Yusupov Hospital are given consultations with therapists and cardiac surgeons.
Doctor's advice
In addition to the generally accepted lifestyle interventions described above, I strongly encourage my patients to monitor their blood pressure and take appropriate medications regularly.
If a person suffers from diabetes, he should regularly check his blood glucose levels and periodically take a glycated hemoglobin test. This is important, since diabetes can worsen the course of angina several times and lead to complications.
Also, if you cannot eat fish often, you can take fish oil in the form of dietary supplements. They are available in any pharmacy. To argue for the benefits of fish oil, I would like to give the example of Japan, a country where heart disease rates are extremely low, and fish as a food product occupies the top positions.
Clinical case
I would like to provide an example from personal experience.
A 52-year-old man visited his local physician for an outpatient appointment with complaints of pressing pain in the heart area, which occurs when climbing the stairs to the 3rd floor and goes away a few minutes after resting. I began to notice the appearance of these pains about a month ago. Suffering from type 2 diabetes mellitus and hypertension. She takes Metformin 1000 mg 2 times a day and Lisinopril 10 mg 1 time a day. The therapist referred him to a cardiologist, who prescribed an ECG and VEM (veloergometry). At rest, when deciphering the ECG, there were no changes. When performing a VEM, an ECG revealed ST segment depression of 2 mm. The patient was sent to the cardiology hospital for further examination with a diagnosis of coronary artery disease, angina pectoris FC 2. Coronary angiography was performed, which revealed 70% stenosis of the right coronary artery. The damage to the remaining vessels was not critical, so the decision was made to install a stent. Drug therapy was also prescribed (Acetylsalicylic acid, Rosuvastatin, Bisoprolol). The patient noted a significant improvement in his condition in the form of cessation of pain attacks. Upon discharge, recommendations for lifestyle modifications were given.
In conclusion, I would like to note that angina pectoris is a serious disease that requires due attention from both the doctor and the patient. Ignoring attacks of pain can lead to an unfavorable prognosis in the form of myocardial infarction, disability and death. However, timely diagnosis and proper treatment can improve the quality and increase the life expectancy of a person.
Chronic heart failure: treatment, drugs
CHF is a disease in which patients need to constantly take medications. For chronic heart failure, drugs are used that help slow the progression of the process and improve the patient's condition. In some patients with CHF, treatment requires surgical intervention.
Medicines for chronic deficiency are primary, auxiliary and additional.
The main drugs include ACE inhibitors (angiotensin-converting enzyme), angiotensin receptor antagonists, beta-blockers, aldosterone receptor antagonists, diuretics, ethyl esters of polyunsaturated fatty acids, cardiac glycosides. Cardiac glycoside for the treatment of chronic heart failure is used most often in patients with atrial fibrillation.
Auxiliary drugs for chronic heart failure are used in special clinical situations with complications of CHF. These include nitrates, calcium antagonists, antiarrhythmic drugs, antiplatelet agents, and non-glycoside inotropic stimulants.
Additional medications for chronic insufficiency: statins, indirect anticoagulants.
For patients diagnosed with chronic heart failure, clinical recommendations from doctors relate not only to taking medications, but also to revising their lifestyle in general:
- it is necessary to stop smoking and drinking alcohol;
- bring your weight back to normal;
- follow a salt-free diet. Nutrition for CHF should be balanced, contain a sufficient amount of proteins and vitamins;
- walk more in the fresh air.
Treatment
Before starting treatment, I need to assess the risk, i.e. the likelihood of the patient developing complications in the future (myocardial infarction and death). This is necessary to choose treatment tactics.
To do this, I pay attention to the following parameters:
- Results of tests with physical activity (the time of performing the exercise, after which the patient has an attack);
- echocardiography indicators, namely the adequacy of the pumping function of the heart;
- glow intensity on myocardial scintigraphy;
- the prevalence of atherosclerosis of the coronary arteries and the degree of narrowing of their lumen.
If the patient is at low or medium risk, then I limit myself to drug therapy. And if he is at high risk, then he needs more aggressive treatment of angina pectoris in the form of surgery.
The Braunwald Guide for the treatment of cardiac diseases, the most authoritative publication, recommends the use of the following medications for angina pectoris:
- Beta-blockers (Bisoprolol, Metoprolol) - reduce the pulse rate and slow down the conduction of nerve impulses, thereby reducing the myocardial need for oxygen. In addition, due to an increase in the period of relaxation (diastole) of the heart muscle, its blood circulation improves.
- Slow calcium channel antagonists (Diltiazem, Verapamil) have a similar mechanism of action. I use them in case of intolerance to beta-blockers or if there are contraindications to them.
- Antiplatelet drugs are necessary to prevent the formation of blood clots in the arteries, which lead to a heart attack. First, I prescribe Acetylsalicylic acid, and if the patient has a stomach or duodenal ulcer, then Clopidogrel.
- Statins (Atorvastatin, Rosuvastatin) - reduce the concentration of cholesterol in the blood, thereby slowing down the process of formation of atherosclerotic plaque.
- ACE inhibitors (Perindopril, Lisinopril) - these medications are needed by patients who, in addition to angina, suffer from chronic heart failure or diabetes.
- Blockers of If-channels of sinus node cells (Ivabradine) are so-called pulse-lowering drugs. I use them when the patient has a very fast pulse (more than 100).
This scheme allows me to achieve clinical improvement in the form of cessation of pain in some patients. If attacks persist with the selected therapy, then I add nitrates (Nitroglycerin). These drugs relax the smooth muscle walls of the coronary arteries, which leads to their expansion and increased blood flow to the myocardium.
However, these drugs must be handled very carefully, since if they are not taken correctly, tolerance (addiction) quickly develops, and their therapeutic effect is reduced several times. Therefore, I always recommend that my patients take nitrates only when an attack begins, or no more than 2 times a day, and so that the interval between doses is at least 12 hours.
If drug treatment is unsuccessful, or if the patient has a high cardiovascular risk, surgery is performed.
There are 2 main types of operations:
- Stenting, or percutaneous coronary intervention (PCI);
- coronary artery bypass grafting (CABG)
The essence of PCI is the introduction of a special metal stent into the vessel, which improves its patency. The operation is performed under local anesthesia. Access is through the femoral artery. PCI is performed when stenosis in one vessel is more severe than 50%.
When performing CABG, a connection is created between the aorta and the coronary artery to bypass the narrowed vessels. CABG is an open abdominal operation with general anesthesia (anesthesia) and opening of the chest. This method is justified if several arteries are affected or stenting is not possible.
Lifestyle requirements
In order for drug and surgical treatment to have maximum effect, I recommend that my patients adhere to a certain lifestyle, which includes several aspects:
- bad habits – it is advisable to limit alcoholic drinks (to about 300 ml of wine per week). Smoking is strictly prohibited;
- diet - reducing the consumption of foods rich in saturated fats (meat, milk, butter) and increasing foods with a predominant content of omega-3.6 fatty acids (vegetables, fish, vegetable oil). The diet must include fruits, nuts, and cereals;
- regular moderate physical activity or exercise therapy - aerobic exercises are preferable, such as swimming, running, cycling;
- body weight control is achieved by strict adherence to the previous 2 points.
Chronic heart failure: recommendations for prevention
Prevention of chronic heart failure is based on the basic principles that every person should adhere to, especially after 40-45 years:
- engage in physical activity regularly;
- control blood pressure;
- lead a lifestyle that prevents the development of coronary artery disease;
- normalize metabolism (reduce excess weight, control cholesterol levels, limit salt intake);
- give up frequent consumption of coffee, alcoholic beverages, quit smoking.
Thanks to the clear and consistent implementation of the above recommendations, it is possible to significantly slow down the pathological process and improve the patient’s quality of life.
Diagnosis and treatment of CHF in Moscow is offered by the Yusupov Hospital Therapy Clinic, a leading multidisciplinary center equipped with the latest equipment. The use of innovative techniques and the vast experience of the clinic’s team of specialists - therapists, cardiologists, diagnosticians - allows us to achieve impressive results in the treatment of chronic heart failure. Each patient at the Yusupov Hospital is provided with professional nursing care. In case of chronic heart failure, not only drug treatment is necessary, but also a review of the diet, which our qualified nutritionists help to cope with, who develop a special nutrition plan for each patient with CHF.
Providing first aid for acute illness
The acute form of decompensated heart failure requires urgent assistance to the patient anywhere. To do this you need:
- call an ambulance, while informing the dispatcher in detail about the symptoms of the patient’s pathological condition;
- give the victim a comfortable sitting or semi-sitting position with the back raised as much as possible and arms and legs down. The head and back should be supported by some object and, if possible, lowered into a container of hot water. This positioning of the body will help reduce shortness of breath and will help reduce the load on the heart;
- to provide the patient with fresh air, it is necessary to remove clothes from the chest, free the neck, open doors and windows;
- Pulmonary edema can be prevented by using a piece of cotton wool soaked in alcohol or strong alcoholic drink (vodka) and placed directly next to the patient’s nose;
- set blood pressure readings. When it decreases to a level of less than 90 mm Hg. Art. It is advisable for the patient to take Nitrosorbitol or Nitroglycerin, as well as a diuretic (Lasix or another) in the amount of 1 tablet. Nitrate preparations are used until symptoms disappear every 5–10 minutes. 1 tablet, but not more than 4 pieces;
- after 15 minutes. After the onset of symptoms, it is advisable to apply a moderately compressive tourniquet to the shoulder or thigh for about half an hour. After this time, the position of the tourniquet must be changed to avoid prolonged compression of the limbs;
- absence of pulse, breathing, pressure and heart contractions require urgent resuscitation measures (artificial respiration, chest compressions).
It is advisable for every person to master the technique of performing cardiopulmonary resuscitation; this knowledge can save the life of another person



![Rice. 1. Functioning of the glymphatic system of the brain (according to [11]) 1. Glymphatic system functioning (according to [11])](https://expert35.ru/wp-content/uploads/ris-1-funkcionirovanie-glimfaticheskoj-sistemy-mozga-po-11-fig-1-330x140.jpg)