The article was published on p. 49-52
Isolated pulmonary artery stenosis (ISPA) is a congenital anomaly characterized by obstruction of the right ventricular outflow tract and disruption of the blood outflow pathways from it into the pulmonary circulation. According to ICD-10, Q 25.6 “Pulmonary artery stenosis” is distinguished. The first descriptions of the vice belong to JB De Senac (1749) and GB Morgagni (1761).
The frequency of ISHA, according to sectional and clinical data, among all congenital heart defects (CHD) ranges from 2.4 to 12%.
Pathogenesis
In a healthy person, the pressure in the right ventricle and the artery that carries blood to the lungs is the same. The pulmonary artery valve has a tricuspid structure, and when contraction of the right ventricle occurs, all its valves open completely under the influence of blood flow and facilitate its free flow into the space of the pulmonary artery. Then the walls of the right ventricle relax and fill it with venous blood coming from the organs and tissues of the body, which causes the valve flaps to close and ensures complete closure for the reverse flow of blood and the impossibility of penetration of biological fluids in the opposite direction - from the pulmonary artery to the right ventricle.
Pathogenesis causing pulmonary valve stenosis
In the case of valve stenosis, due to partial fusion of the leaflets, their complete opening becomes impossible, valve stenosis and a difference in pressure occur - in the ventricle it is too high, and in the pulmonary artery it is low enough to form a pressure gradient. In some cases, valvular stenosis causes the deformed leaflets to bulge during systole into the lumen of the trunk into the pulmonary artery and accelerate the systolic flow.
Stenotic valve
As a result of pulmonary stenosis, to compensate for hemodynamic disturbances, the right ventricle is forced to work extra hard to push blood through the narrowed lumen. This can lead to stretching, rigidity and hypertrophy (thickening) of the walls, as a result of which its cavity increases, rhythm is disturbed and heart failure . The narrowing site reduces the volume of blood flow, and insufficient blood supply to the lungs causes frequent bronchopulmonary diseases.
Forecast
Children with successful balloon valve repair have a favorable prognosis for life. Patients with a dysplastic pulmonary valve, often found in Noonan syndrome, have less favorable outcomes. Patients with successful balloon repair rarely require reoperation, unlike patients with right ventricular hypoplasia. The survival rate for such children is 60%. Mild to moderate pulmonary stenosis usually does not progress, and children have a favorable prognosis. In patients with severe stenosis, the defect progresses with age. The average life expectancy in the natural course of the defect is 25 years. After surgery, restenosis and valvular insufficiency of the pulmonary artery are possible. Long-term good results after surgical treatment were recorded in 84.3% of patients.
Classification
Depending on the location of the narrowing, there are:
- valvular stenosis is the most common case when the pulmonary valve itself is subject to pathological changes; its valves can be underdeveloped, fused together by commissures, and even have the appearance of a membrane with a hole in the center, ranging in size from 1-1.5 mm to normal;
- supravalvular - in which the trunk of the pulmonary artery is narrowed above the location of the valve;
- subvalvular (infundibular) – in this case, excessive growth of muscle tissue or fibrous structures in the area of the outflow tract of the right ventricle has occurred, preventing the blood flow from entering the pulmonary artery;
- peripheral - caused by a narrowing of the branches of the pulmonary artery that bring blood to the right or left lung.
According to the nature of the severity, the disease can be mild (asymptomatic), moderate-severe and critical.
Treatment
Treatment of secondary pulmonary hypertension is aimed at getting rid of the underlying disease. Patients with severe pulmonary arterial hypertension due to chronic thromboembolism are treated with pulmonary thromboendarterectomy. This operation is considered more complex than emergency surgical embolectomy. Under conditions of extrapulmonary circulation, an organized vascularized thrombus is excised along the pulmonary trunk. In specialized centers, the mortality rate during and after surgery is less than 10%.
Treatment of primary pulmonary hypertension should begin with oral calcium channel blockers. In a minority of patients, these drugs reduce pulmonary artery pressure or pulmonary vascular resistance. Most doctors do not recommend verapamil because it has a negative inotropic effect. If treatment with calcium channel blockers is effective, the prognosis is favorable, you need to continue the course. If there is no response to treatment, the doctor prescribes other drugs.
Intravenous epoprostenol (a prostacyclin analogue) is often used to treat pulmonary hypertension. It increases survival in patients, even those who do not respond to vasodilator medications during catheterization. This treatment has disadvantages, such as the need for an indwelling central catheter. Side effects also occur, such as bacteremia and diarrhea. Oral (beraprost), inhaled (iloprost), subcutaneous (treprostinil) analogs of prostacyclin are considered alternative drugs. But their effects on the human body are still being studied, so they are not widely introduced into medical practice.
The oral endothelin receptor antagonist bosentan is effective in some cases. It is mainly prescribed for milder forms of pulmonary hypertension and insensitivity to vasodilators. L-arginine and oral sildenafil are also currently under investigation.
Lung transplantation is a dangerous procedure that can cause complications, because it is possible that an infection may occur and the body may reject the new lung. The procedure is used for heart failure of the fourth degree (according to the classification of the New York Heart Association), when a person develops shortness of breath even with minimal activity, due to which he cannot actively live, but constantly lies or sits; and only if in such cases there is no effectiveness of prostacyclin analogues.
Many patients are prescribed additional medications to treat deficiency, including diuretics. They should also receive warfarin to prevent thromboembolism.
Symptoms
The clinical picture can vary significantly depending on the severity of the stenosis and can even be asymptomatic, for example, if the pressure gradient between the heart and artery does not exceed 25 mm Hg. I don’t even prescribe treatment for such people.
The symptom complex usually manifests itself in the form of an increasing and decreasing ejection noise, cyanosis of the skin, the development of a “heart hump” and various signs of heart failure, including:
- causeless fainting;
- swelling;
- liver enlargement;
- frequent chest pain and discomfort (“angina pectoris”);
- dyspnea.
Heart defects in children
Heart defects are a common pathology in children. The frequency of defects in children has been increasing in recent years. Consultation and examination by a pediatric cardiologist - Markushka Children's Clinic.
Congenital heart defects in children, child
The incidence of congenital heart defects (CHD) in newborns is 0.8%, they vary widely in anatomical features and severity. The clinical manifestations of congenital heart disease in children are varied and are determined by three main factors: the anatomical features of the defect, the degree of compensation and the complications that arise.
CHD in a child can be suspected if he has: cyanosis or severe pallor, malnutrition, frequent colds, insufficient tolerance to age-appropriate physical activity (fatigue during breastfeeding, during outdoor play, shortness of breath when climbing even one flight of stairs and etc.), an increase in heart size, a change in heart sounds, the appearance of a heart murmur, a change in the pulse in the arms, a weak or absent pulse in the femoral artery, a change in arterial blood pressure, chest deformation, heart rhythm disturbances, any pathological ECG changes, unusual changes detected on a chest x-ray, etc.
Congenital heart defects with enrichment of the pulmonary circulation
Atrial septal defect (ASD) is one of the most common congenital heart diseases. In 10-20% of cases, ASD is combined with mitral valve prolapse.
Hemodynamics in ASD are determined by the discharge of arterial blood from left to right, which leads to an increase in the minute volume of the pulmonary circulation. In the formation of a shunt, the difference in pressure between the right and left atria, the higher position of the latter, the greater distensibility of the right ventricle and the area of the right atrioventricular orifice, resistance, and the volume of the vascular bed of the lung are important. The development of pulmonary hypertension and damage to the vascular bed of the lungs lead to reverse shunting of the blood and the appearance of cyanosis. With primary defects, mitral insufficiency is often observed.
Unlike ventricular septal defects, in which significant shunt leads to volume overload in both ventricles, with ASD the shunt is smaller and affects only the right side of the heart.
With severe weight loss, patients experience weight loss and a tendency to recurrent respiratory diseases and pneumonia in the first years of life. As a rule, in these cases there are complaints of shortness of breath, fatigue, and heart pain.
Ventricular septal defect (VSD) is one of the most common congenital heart defects. It accounts for 17 to 30% of cases of cardiac anomalies.
There are three types of VSD development depending on the hemodynamic characteristics of the defect (the size of the left-right shunt), which determine the clinical manifestations and prognosis of the disease.
The first type - there is a small defect in the septum (less than 0.5 cm2/m2), a small discharge of blood (<25% of stroke volume) does not cause changes in pressure in the right ventricle and pulmonary circulation, pulmonary hypertension does not develop. There are no clinical manifestations. Children with this defect do not require systematic treatment.
The second type is a medium-sized defect (0.5-1 cm2/m2) that leads to a greater discharge of blood into the right ventricle (<50% of stroke volume) and an average increase in pressure in the pulmonary circulation. With this type of VSD, the clinical signs of the defect are mild and there are no problems with treatment. Retarded physical development, congestive heart failure, and recurrent lower lobe pneumonia may occur. Such children are operated on in preschool age.
The third type is a large defect (more than 1 cm2/m2), when the discharge of blood into the right ventricle exceeds 50% of the stroke volume. It is characterized by frequent bronchopulmonary diseases, growth disturbances and signs of heart failure, which, if severe, require radical or palliative surgery. With high pulmonary resistance, shortness of breath at rest and during exercise, chest pain, cyanosis, and hemoptysis may be observed. Most patients die in childhood and adolescence.
Most ventricular septal defects are small and pose a risk for infective endocarditis.
Patent aortic duct in children, child
The ductus arteriosus (ductus arteriosus) connects the pulmonary artery and the aorta immediately behind the left subclavian artery. Functional closure of the patent aortic duct in full-term infants occurs 10-15 hours after birth, obliteration of the duct occurs after several weeks of life. In premature babies, the PDA can function from several weeks to a month. In full-term infants, it remains open in case of structural abnormalities; in premature infants, the more immature the child, although spontaneous closure is common.
In PDA, there is a discharge of blood from the aorta into the pulmonary artery due to higher pressure in the aorta, which leads to overflow of the pulmonary circulation and overload of the left chambers of the heart. With the development of pulmonary hypertension, overload of the right ventricle also occurs. The diameter and length of the duct determine the severity of the accompanying hemodynamic disturbances, which are similar to those with VSD of various sizes.
Typically, clinical manifestations of the defect occur at the end of the 1st or 2-3rd year of life. Before the appearance of clinical symptoms of the defect, children develop physically and neuropsychically normally, and the first phase of the course of the defect is easy for some of them. Early clinical signs of the defect occur with wide ducts.
Complete transposition of the great vessels in children, child
Complete transposition of the great vessels (TMS) - the aorta departs from the right ventricle, the pulmonary artery from the left, and two separate and independent circulations are formed. The life of a child after birth is possible only if there are compensatory communications . This heart defect represents the leading cause of death in the first two months of life among other congenital heart defects.
Congenital heart defects with depletion of the pulmonary circulation
Pulmonary artery stenosis (PAS) is most often caused by stenosis of the pulmonary valves, less often by sub- and supravalvular stenosis, stenosis of the branches of the pulmonary artery. Subvalvular stenosis is often part of a complex congenital heart disease.
Obstruction of the outflow of blood from the right ventricle into the pulmonary artery causes an increase in systolic pressure and hypertrophy of the right ventricle. The magnitude of the pressure gradient depends on the size of the valve ring opening.
In most children under one year of age and older, the disease is asymptomatic, although in some cases slight fatigue is noted.
Mild or moderate SLA may have no symptoms. With severe stenosis, shortness of breath, heart pain, and pallor are observed.
Tetralogy of Fallot
Tetralogy of Fallot is characterized by a large ventricular septal defect, the location of the aorta over the defect, right ventricular hypertrophy, and pulmonary stenosis.
Due to the large size of the VSD, systolic pressure is equal in both ventricles and the aorta. The degree of obstruction of the right ventricle determines the direction and volume of blood discharge. In most cases it is large enough to overcome systemic resistance and cause right-to-left shunting and development of cyanosis. The size of the VSD is of secondary importance, since its diameter is basically equal to the diameter of the aortic orifice.
There are two main forms of TF. In the extreme case of tetralogy of Fallot, a type of common false truncus arteriosus, the pulmonary trunk does not work, the child’s condition is severe, and a pronounced hemodynamic disturbance is observed. In 80% of cases, children die in the first month of life without surgical intervention.
In the classic version of tetralogy of Fallot, there is pulmonary artery stenosis (usually valvular and the outlet of the right ventricle), ventricular septal defect (membranous part), dextraposition of the aorta (aorta above the ventricular septal defect), secondary hypertrophy of the right ventricle.
Children are lagging behind in physical development and are characterized by shortness of breath (when feeding or moving the child), cyanosis, and deformation of the fingers and toes (“drumsticks”). Attacks of increasing cyanosis with deepening of breathing—dyspnea-cyanotic—develop in children under one year of age and in young children. The prognosis is poor due to the development of complications of cyanosis and polycythemia, such as stroke and brain abscess. Infectious endocarditis often develops.
Congenital heart defects with impoverishment of the systemic circulation
Coarctation of the aorta (CA). Narrowing is observed below the origin of the left subclavian artery from the aorta. Although narrowings can be localized in any area, from the arch to the bifurcation of the aorta, in 98% of cases they are located in the region of the branch of the ductus arteriosus. With preductive stenosis (infantile form), narrowing is observed before the PDA; this form is combined with other defects: VSD, bicuspid aortic valve, transposition of the great vessels, etc.
Clinical manifestations of the defect occur already during the newborn period. Symptoms in children in the first year of life are characteristic of heart failure. Feeding difficulties and low weight gain are common. In older children, the disease is usually asymptomatic, although there may be some fatigue or weakness in the legs when running.
Classic signs of coronary artery disease are different pulses and blood pressure in the arms and legs: arterial hypertension in the upper extremities and absence or weakening of the pulse in the arteries of the legs and significantly lower blood pressure in the legs than in the arms (normal blood pressure in the legs is 10-20 mm Hg . century higher than on the hands). The pulsation of the vessels of the upper half of the body is pronounced, and an elevating left ventricular impulse is detected. The borders of the heart are expanded to the left.
Aortic stenosis in children, child
Aortic stenosis (AS) accounts for about 5% of all congenital heart disease in children. Valvular stenosis is more common (about 80%), less common (20%) are subvalvular and supravalvular variants of aortic stenosis. An anomaly in the structure of the aortic valve (bicuspidity) is one of the main congenital heart defects in adults. The course and prognosis of the defect are determined by its localization and severity, combination with other heart defects and fibroelastosis, concomitant myocardial damage.
With severe stenosis, signs of severe left ventricular failure appear already in infancy, but in most cases the defect is detected at school age. Patients complain of fatigue, shortness of breath, pain in the heart, dizziness, and fainting.
Acquired heart defects in children, child
Acquired heart defects are acquired morphological changes in the valve apparatus, leading to disruption of its function and hemodynamics. Most often they arise as a result of rheumatism, infective endocarditis, systemic connective tissue diseases, trauma, and mitral valve prolapse (MVP).
Mitral valve insufficiency in a child, children
Mitral (bicuspid) valve insufficiency develops when its leaflets, as well as the subvalvular apparatus, are damaged. It occurs as a complication of rheumatism, infective endocarditis, systemic connective tissue diseases, as a result of trauma, MVP, pathology of the valve apparatus: rupture of chords, rupture or dysfunction of papillary muscles, dilatation of the mitral ring or left ventricular cavity, etc.
Children may not make any complaints. With long-term valve insufficiency, a bulging of the left half of the chest - a cardiac hump - can form.
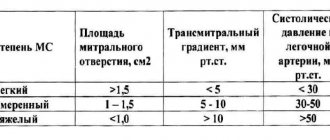
Mitral stenosis can be primary (with latent or subacute rheumatism) or secondary, occurring against the background of mitral valve insufficiency. Congenital mitral stenosis manifests itself as heart failure in infancy and early childhood.
The pressure in the left atrium increases, its hypertrophy develops, and blood flow into the left ventricle accelerates due to the narrowing of the mitral orifice to 1-1.5 cm2 (normally, the area of the mitral orifice is 4-6 cm2). There is a high risk of infective endocarditis with any valve damage. In severe mitral stenosis (mitral orifice area <1 cm2, pressure in the left atrium exceeds 25 mm Hg, which leads to pulmonary hypertension at rest. With a full-blown clinical picture, children complain of shortness of breath and fatigue (dyspnea on exertion occurs when The area of the valve opening is halved (< 2 cm2).Atrial fibrillation, infections and infective endocarditis can cause pulmonary edema in severe mitral stenosis.
Aortic valve insufficiency in children, child
Most often, aortic valve insufficiency occurs as a result of deformation of the aortic valves during rheumatism (almost always combined with damage to the mitral valve), due to infective endocarditis, myxomatous valve degeneration, trauma, hereditary connective tissue diseases, congenital bicuspid valve, etc.
In case of aortic valve insufficiency, part of the blood returns during diastole from the aorta to the left ventricle, as a result of which the muscle fibers of the left ventricle stretch and hypertrophy.
Patients complain of shortness of breath and palpitations that occur during physical activity, and often of pain in the heart area. The skin is pale, and there is often increased pulsation of the carotid arteries (carotid dancing). The pulse is fast and high, less often the appearance of a capillary pulse can be noted.
Aortic stenosis in children, child
Most often, stenosis of the aortic mouth occurs as a result of deformation and development of fibrosis and calcification of the bicuspid aortic valve, due to rheumatism (almost always combined with damage to the mitral valve), isolated calcification of the aortic valves, infective endocarditis with massive vegetations, and trauma.
With aortic stenosis, hemodynamics are determined by a narrowing of the left ventricular outflow tract and an increase in the load on the left ventricle (systolic overload). With a mild degree of stenosis, the area of the aortic valve opening is 1.2-2 cm2, with moderate stenosis - 0.75-1.2 cm2, with severe stenosis <0.75 cm2. 15-20% of patients with symptoms of aortic stenosis die suddenly.
Mitral valve prolapse in children, child
Mitral valve prolapse (MVP) is the bowing of the mitral valves into the cavity of the left atrium during left ventricular systole. This syndrome is more often associated with an anomaly in the structure of the valve, in which one of its leaflets (usually the posterior one) or both sag at the end of systole into the cavity of the left atrium. MVP can be primary (idiopathic) or secondary (as a result of congenital or acquired diseases).
Among congenital diseases, MVP is more often combined with hereditary connective tissue diseases (Marfan, Ehlers-Danlos, Holt-Oram syndromes, etc.). Patients often experience asthenic physique, scoliosis, flat feet, valgus deformity of the feet, and relaxation of ligaments. In the occurrence of MVP, a certain role is played by the condition of the subvalvular apparatus - elongation or anomalies in the attachment of chords, the shape of the valve leaflets. MVP occurs with pathological changes in its leaflets and valve chords, dysfunction of the papillary muscles, impaired contractility of the left ventricle in rheumatism, non-rheumatic carditis, bacterial endocarditis, cardiomyopathies, congenital heart disease. MVP often accompanies neurocirculatory dystonia and functional cardiopathy, in which there is a predominance of the sympathetic or parasympathetic part of the autonomic nervous system. Hereditary predisposition plays a major role in its genesis.
Children with MVP do not show any special complaints, so the disease is usually detected by chance. Sometimes there is pain in the heart, dizziness, fainting (eg for a child - Markushka clinic), which is caused by vegetative changes, often a decrease in blood pressure.
Tests and diagnostics
In case of narrowing of the blood-expelling structures of the heart or pulmonary artery, you should consult a doctor - a cardiologist who can assess the scale and nature of the pathological changes. During examination, patients may be diagnosed with:
- hypertrophy on palpation;
- signs of systolic overload of the right ventricle on the electrocardiogram - deviation of the electrical axis of the heart to the right, displacement of the ST segment by 2-5 mm below the isoline and a negative deep T wave, although more often the data obtained are within normal limits;
- bifurcation of the second heart sound;
- a hard ejection noise, a click and a decreasing ejection noise are heard in the second intercostal space with valvular stenosis or the fourth intercostal space with subvalvular stenosis of the pulmonary trunk in patients in a forward leaning position when using a stethoscope;
- the noise becomes louder during the Valsalva maneuver and during inspiration, and can lengthen and intensify as the stenosis progresses;
- ECG usually reveals hypertrophy of the walls of the right ventricle;
- using Doppler echocardiography, it is possible to detect pronounced turbulent blood flow at the level of the pulmonary valve and obtain an image of the narrowing, establish the severity of the patient’s condition and the pressure gradient - if it does not exceed 35 mm Hg, then the damage is considered mild, if within 35-65 mm Hg - moderate, over 65 mmHg - severe.
Patients may need periodic cardiac ultrasounds to monitor possible progression of stenosis (narrowing).
Interview and examination of the patient
It is necessary to find out whether the patient has had episodes of deep vein thrombosis, sudden swelling of the legs, or thrombophlebitis. Many patients have a family history of sudden death, cardiovascular disease, and an increased tendency to thrombus formation.
Objective evidence of a history of pulmonary embolism (PE) is the coincidence in time of the clinical presentation of thrombosis of the veins of the lower extremities and the appearance of shortness of breath. In the coming months after PE, a period can be identified in patients when the condition remains stable and asymptomatic. This is due to the fact that the right ventricle copes with the load and allows maintaining good exercise tolerance until progressive pulmonary vascular remodeling develops. Almost the only reliable evidence of previous PE can be data from perfusion scintigraphy or computed tomography of the lungs performed during an acute episode of PE.
During a general examination of patients with CTEPH, blueness (cyanosis) may be detected. With the development of right ventricular heart failure, swollen neck veins, enlarged liver, peripheral edema, and abdominal dropsy are noted.
Pulmonary stenosis in newborns
In newborns, a severe (critical) form of stenosis causes heart failure and a bluish tint to the skin, and a pronounced heart murmur raises suspicion.
The pressure gradient can disappear over time and be compensated by the internal forces of the body, however, the condition of the resulting post-stenotic aneurysmal dilatations of small vessels can be complicated by thrombosis and arteritis , causing pulmonary hemorrhages. Severe stenoses can lead to death, both in infancy and in subsequent periods of life.
Diet for pulmonary stenosis
Diet 10th table
- Efficacy: therapeutic effect after 1 month
- Timing: constantly
- Cost of products: 1700-1850 rubles. in Week
Pulmonary artery stenosis requires a special diet, most often prescribed number 10 with a significant reduction in salt content, which ensures normal functioning of the cardiovascular system. In addition, it spares the gastric and urinary systems. Typically the following products are preferred:
- unhealthy and whole grain bread;
- various types of dietary soups;
- obligatory vegetable side dishes;
- eggs;
- fruit sauces and salads;
- low-fat dairy products.
Spicy, salty, spicy and smoked foods, as well as animal fats, are prohibited. Drinks that contain caffeine and alcohol. It is recommended to limit fats, even of vegetable origin.