Saturation (English saturation - “saturation”) is an indicator of the level of oxygen saturation in the blood. If it is at a low level, this indicates hypoxemia - a condition requiring emergency medical attention.
It is necessary to normalize the level of oxygen in the lungs and blood, otherwise complications, including death, are possible.
Doctors use a special medical device to measure oxygen saturation - a pulse oximeter. Using this device, an analysis is made that gives an idea of the current state of the patient’s lungs and circulatory system. Thanks to the quick results, doctors decide on the need for additional oxygen support. Since it is not possible to urgently organize a computed tomography (CT) scan in all cases, reduced saturation helps specialists determine the presence of a viral infection of the respiratory system - pneumonia.
Measuring oxygen in the lungs and in the circulatory system with a pulse oximeter makes it possible to assess the patient’s condition and hospitalize him. This is especially true when affected by COVID-19. If a person who suspects he has this disease has such a device, he can analyze the condition at home. However, it is worth knowing that measurement cannot be an alternative to other methods.
Both the patient and the staff of the medical institution should not draw conclusions based on saturation - oxygen levels in the blood can vary depending on various factors:
- device sensitivity;
- the color of the patient's skin;
- type of lighting.
If we consider saturation as the main diagnostic method, the risks of incorrectly assessing the patient’s condition are quite high.
Even with a severe form of coronavirus, oxygen may be at an acceptable level in the first days, and then drop sharply. The decrease occurs at night even in those who are completely healthy.
More about saturation
Saturation is a parameter showing the oxygen level as a percentage. It enters the bloodstream from the lungs and is transported to all systems of the body. If the indicator is lowered during coronavirus, this indicates a lack of oxygen - hypoxemia is highly likely provoked by a viral infection of the respiratory system. The assumption can be confirmed or refuted by conducting other studies, such as CT, where the doctor evaluates the visual condition of the organ.
determination of oxygen norm with a pulse oximeter
Treatment of coronavirus with oxygen
Oxygen therapy is the main method of treating inpatients in serious condition, as it alleviates the patient’s general condition, reduces shortness of breath and normalizes blood gas composition.
If the blood oxygen deficiency is 80-94%, an oxygen mask or gas supply through nasal cannulas is sufficient, and if the decrease is less than 80%, mechanical ventilation is used.
Oxygen and helium - relief for lungs during COVID-19
With the use of oxygen, everything is clear - air mixtures with a high content of this gas (O2 in air is only 21%) make it easier for severe patients to breathe and increase blood saturation with oxygen. Even with severely damaged lungs, concentrated oxygen mixtures provide improvement.
Pulmonologist, Academician of the Russian Academy of Sciences Alexander Chuchalin spoke about the benefits of helium during Covid. He explains that helium is a small molecule that easily penetrates the airways and facilitates the delivery of O2 from the alveoli to the blood. Helium improves the condition of patients with respiratory failure, increases saturation and speeds up recovery.
WHO experts recommend starting oxygen support for COVID-19 if saturation is 90% or less . Russian protocols for the treatment of coronavirus (version 9 of October 26) indicate that a value of less than 94% is a reason for hospitalization and oxygen therapy.
Transfusion of oxygenated blood
Transfusions of blood products with good oxygen saturation help quickly eliminate the shock state of the organs and compensate for the resulting disorders. This treatment is indicated if oxygen support does not produce the expected results due to too large an area of damage to the lung tissue. In addition to blood, modified hemoglobin preparations that increase saturation are rarely used to treat patients.
Transfusion of blood enriched with atomic oxygen is indicated when saturation is less than 50%.
Why are measurements taken?
The oxygen level is measured to determine the state of health and promptly identify hypoxemia, which can cause death. Through this simple analysis, the degree of the disease is determined and measures are taken to stabilize the condition.
With the advent of COVID-19, the term Silent Hypoxemia has been used, which translates as “silent hypoxemia.” Its appearance is due to the fact that about 50% of patients admitted to hospital have a low level of saturation, while the symptoms indicate the opposite. Patients do not experience shortness of breath, they are not tormented by a cough, and their body temperature is at a normal level. However, a CT scan shows significant lung damage, so the patient is placed on oxygen support.
Methodological manual on pulse oximetry. Part 1
This article presents information from a manual on pulse oximetry: “Diagnostic capabilities of non-invasive monitoring of arterial blood hemoglobin oxygen saturation in the clinic of internal diseases: method.recommendation. / D.V. Lapitsky [and others]. – Minsk: BSMU, 2015. – 71 p.”
Intended for doctors of therapeutic specialties, 5th-6th year students of the Faculty of Medicine, clinical residents, interns.
1. Basics of the pulse oximetry method.
In the physiology of respiration, it is customary to distinguish two key processes: cellular (tissue) respiration and external respiration (gas exchange) [1,2]. Cellular respiration is the process by which the cell releases energy from carbohydrates, fats and proteins [3]. External respiration ensures the supply of oxygen to the body for use in the biological oxidation of organic substances (i.e., in the process of cellular respiration), and the removal of the product of this oxidation, carbon dioxide, from the body. Thus, arterial blood can be represented as a link between external and internal respiration. The gas composition of arterial blood reflects the efficiency of external respiration and allows us to indirectly predict the risk of developing tissue hypoxia. Based on these positions, the diagnostic value of assessing the gas composition of arterial blood becomes clear.
The study of the gas composition of alveolar gas and arterial blood was initiated by the English physiologist John Scott Haldane at the beginning of the 20th century. Advances in science and technology over the past century have made it possible to formulate a coherent theory of gas exchange and to design instruments (for example, Radiometer Medical ApS, Denmark) for determining gases in samples of exhaled air, arterial and venous blood [4,5]. However, this examination requires stationary equipment and is invasive.
For the needs of practical and applied medicine, a method for quickly and non-invasively assessing the oxygen status of arterial blood is required. The search for such a method has been carried out since the 30s of the 20th century. In 1940, the first hemoximeter was designed to detect hypoxemia in pilots during flight. The developed equipment was bulky and required complex maintenance. These circumstances were the reason for the limited use of hemoximeters in clinical practice. The development of technology made it possible already in 1975 to launch the first mobile non-invasive pulse oximeter on the market, allowing long-term monitoring of arterial blood hemoglobin oxygen saturation.
The pulse oximetry method is based on two key physiological phenomena:
- The ability of hemoglobin, depending on its oxygenation, to absorb light of a certain wavelength to varying degrees when this light passes through a section of tissue (oximetry).
- Ripple of arteries and arterioles in accordance with the stroke volume of the heart (pulse wave).
The principle of oximetry is as follows. Deoxyhemoglobin (non-oxygen hemoglobin - RHb) absorbs red light intensely and weakly blocks infrared light. Oxyhemoglobin (fully oxygenated hemoglobin, each molecule of which contains four molecules of oxygen - HbO2) absorbs infrared radiation well, weakly retaining red radiation. Based on the ratio of red (R) and infrared (IR) fluxes that reached the photodetector from the radiation source through a section of tissue (for example, earlobe, finger), the degree of saturation of blood hemoglobin with oxygen is determined - saturation, SO2 (Fig. 1).
Rice. 1 The principle of oximetry (explanations in the text).
A pulse wave is formed as a result of pulsation of arteries and arterioles caused by the release of a certain volume of blood (stroke volume) into the aorta by the left ventricle. Each pulse wave leads to a rhythmic, in time with the heartbeat, change in blood supply to the tissue area under study. The result of recording such fluctuations in blood supply is a photoplethysmogram (PPG). PPG analysis allows you to determine the heart rate and assess the quality of peripheral blood flow (Fig. 2). In various clinical situations, the PPG amplitude can change tens of times. PPG allows you to get a fairly accurate impression of local blood flow. A decrease in PPG amplitude is a sign of peripheral vasoconstriction and/or a decrease in stroke volume, while an increase in amplitude indicates the opposite. Vascular tone is the main factor determining the height of PPG waves.
Rice. 2 Photoplethysmogram.
Another important advantage of recording a photoplethysmogram is the ability to isolate the portion of the intensity of the light flux that is absorbed directly by hemoglobin in arterial blood. When light passes through a section of tissue, it encounters various obstacles, which can be divided into several layers (Fig. 3). Layer 1 is tissue (skin, subcutaneous tissue, nail, bone), layer 2 is capillary and venous blood, layer 3 is blood remaining in the arterioles at the end of each pulsation, a kind of “end-systolic volume” of the arterial bed, layer 4 - additional volume of arterial blood flowing into the arterioles during cardiac systole.
Rice. 3 Absorption of light fluxes from LEDs by various tissues (explanation in the text).
At the moment preceding cardiac contraction, the weakening of light fluxes is due to the first three layers: radiation falls on the photodiode, which is regarded as background. When the next pulse wave reaches the arteries, the volume of blood in them increases and the absorption of light changes. At the peak of the pulse wave, the difference between the background and current radiation becomes maximum. The photodetector measures this difference and believes that it is caused by the additional amount of arterial blood that appears in the path of the radiation. This information is sufficient to use a special algorithm to calculate the degree of oxygen saturation of hemoglobin in arterial blood - SaO2, which is designated as SpO2 when measured with a pulse oximeter.
Thus, the use of one measurement principle (tissue transillumination) allows one to determine three diagnostic parameters at once: the degree of oxygen saturation of hemoglobin in arterial blood (SpO2), heart rate, and the volumetric amplitude of blood filling of a tissue area. Since the measurement is carried out by transilluminating tissue, this method is called “transmission pulse oximetry”. The vast majority of pulse oximeters used in medical practice operate based on this method.
Medical personnel who use pulse oximeters in daily activities need to be aware of the disadvantages and limitations of the pulse oximetry method. Pulse oximetry is an indirect method of assessing ventilation and does not provide information on the pH level, oxygen tension (PaO2) and carbon dioxide (PaCO2) in arterial blood. For practical work, it is useful to know that SpO2 indicators correlate with the partial pressure of oxygen in the blood: a decrease in PaO2 entails a decrease in SpO2. This dependence is nonlinear, which is explained by the S-shaped shape of the oxyhemoglobin dissociation curve (Fig. 4):
- 80-100 mm Hg. Art. PaO2 corresponds to 95–100% SpO2;
- 60 mmHg Art. PaO2 corresponds to 90% SpO2;
- 40 mmHg Art. PaO2 corresponds to 75% SpO2.
In addition, a number of factors can have a negative impact on the accuracy of measurements:
- bright external light and movements may interfere with the operation of the device;
- incorrect placement of the sensor: for transmission oximeters it is necessary that both parts of the sensor are symmetrical relative to the area of tissue being illuminated, otherwise the path between the photodetector and the LEDs will be unequal, and one of the wavelengths will be “overloaded”;
- a significant decrease in peripheral tissue perfusion leads to a decrease or disappearance of the pulse wave. In this situation, the SpO2 measurement error increases;
- at SaO2 values below 70%, the error in saturation measurements using pulse oximetry – SpO2 – also increases. In this regard, it should be noted that in the practical work of a physician in a therapeutic specialty, the probability of encountering SaO2 values below 70% in a patient is extremely low;
- anemia requires higher levels of oxygen to support oxygen transport. With hemoglobin values below 50 g/l, 100% blood saturation can be observed even with a lack of oxygen;
- carbon monoxide poisoning (high concentrations of carboxyhemoglobin can give a saturation value of about 100%);
- dyes, including nail polish, can cause an underestimated saturation value;
- cardiac arrhythmias may interfere with the pulse oximeter's perception of the pulse signal;
- age, gender, jaundice and dark skin color do not affect the operation of the pulse oximeter.
It is the simplicity and non-invasiveness of assessing the quality of peripheral blood flow and oxygen saturation of hemoglobin in arterial blood, as well as the ability of monitor systems to conduct arbitrary long-term monitoring of these parameters, that have contributed to the spread of the pulse kimetry method in departments of anesthesiology and intensive care/resuscitation for monitoring patients in severe conditions. At the same time, specially developed algorithms suppress excessive tissue pulsation, tissue scattering of the light flux and reduce the influence of external lighting and other artifacts on the device readings, making the readings reliable and suitable for systematic analysis.
2. Parameters of arterial blood oxygenation.
The quality of arterial blood oxygenation is assessed by the following indicators [6,7]:
1. PaO 2
– oxygen tension in arterial blood, mm Hg.
Art. PaO2 is the pressure required to keep oxygen in the arterial blood dissolved. The higher this indicator, the more oxygen is contained in the blood and the higher the pressure gradient, which determines the rate of movement of oxygen from capillary blood into tissues. Normally, PaO2 is 92-98 mm Hg. Art. and is measured in laboratory conditions in a microsample of arterial blood;
2. SaO 2
– degree of oxygen saturation of hemoglobin in arterial blood, %.
SaO2 depends on PaO2. The relationship between PaO2 and SaO2 is regulated by several physiological factors (carbon dioxide tension in arterial blood - PaCO2, blood acidity - pH, body temperature, etc.) and is expressed by an S-shaped oxyhemoglobin dissociation curve (Fig. 4). Normal values for this indicator are 95–99% and can be obtained in a microsample of arterial blood. This parameter is measured by a pulse oximeter. It is designated SpO2.
3. P 50
– blood oxygen tension at its half-saturation with oxygen (SO 2 = 50%), mm Hg.
Art. This indicator is determined in a microsample of arterial blood and reflects the affinity of hemoglobin for oxygen. Normal values for this indicator are 26 – 27 mmHg. Art. A decrease in the P50 value corresponds to a shift of the oxyhemoglobin dissociation curve to the left and, accordingly, an increase in the affinity of hemoglobin for oxygen; an increase in P50 indicates a shift of the oxyhemoglobin dissociation curve to the right with a decrease in the affinity of hemoglobin for oxygen (Fig. 4).
4. CaO 2
– oxygen capacity of the blood, reflecting the amount of oxygen in arterial blood, ml/l.
As a rule, this indicator is obtained by calculation. Oxygen is contained in the blood in a dissolved state and in a reversible connection with hemoglobin. The solubility constant of oxygen in arterial blood is 0.031 ml for every 1 mmHg. Thus, the product - 0.031 × PaO2 - represents the amount of oxygen dissolved in arterial blood. One gram of fully oxygenated hemoglobin contains 1.39 ml of oxygen. However, taking into account the correction for pathological hemoglobins (carboxyhemoglobin, methemoglobin), this figure is taken as 1.34 ml/g. The amount of oxygen attached to hemoglobin (Hb) is calculated as 1.34×Hb×SaO2/100 (ml/l). Thus, the oxygen capacity of arterial blood is equal to:
(*) CaO 2
(ml/l) = 1.34 × Hb × SaO 2 /100 + 0.031 × PaO 2 .
Normal values for this indicator are 180 – 204 ml/l.
CaO2 can be estimated using SpO2 values. Due to the fact that the pulse oximetry method does not allow estimating PaO2, the second component of the right side of the equation (*) - 0.031×PaO2 - is ignored. At the same time, CaO2 will decrease insignificantly – from 1.5 to 3.0 ml/l. Thus, equation (*) for a pulse oximeter is written:
CaO 2
(ml/l) = 1.34 × Hb × SaO 2 /100.
Rice. 4. Oxyhemoglobin dissociation curve.
Go to part two
How to determine oxygen deficiency
Patients with symptoms of Covid-19 can independently determine their oxygen levels. Medical assistance is required in the following cases:
- Hold your breath and compare whether you can not breathe as much as before. If it is impossible to hold your breath for a couple of seconds, it makes sense to seek help.
- You take more breaths than before and your heart rate increases.
- The skin has become pale with a slight bluish tint, which appears in the area of the mouth and fingers.
- You feel tired even without much physical activity, and feel drowsy.
- Headaches and dizziness.
- You don't remember simple information.
- Concentration is impaired.
- There are signs that are characteristic of an acute respiratory disease, for example, cough, runny nose, sore throat.
- Tingling in the chest, shortness of breath when talking or moving.
Reviews of coronavirus patients with lack of oxygen
I have asthma, so I bought a pulse oximeter 2 years ago.
When I fell ill with coronavirus, on the second day I began to experience shortness of breath and chest pain. The device showed only 89%, so we immediately called an ambulance and they took me to the hospital. I felt bad for about 2 weeks, I was constantly out of breath, only with an oxygen mask it became easier. After discharge, I suffered from shortness of breath for another month, and my asthma worsened due to Covid. Only 2 months after the onset of the disease, the condition returned to normal. Elena, 59 years old
I was sick with coronavirus without pneumonia, but periodically there was a feeling that there was not enough air.
I was very scared, bought a pulse oximeter and measured my oxygen every 3-4 hours, but the readings were normal. As the doctor told me, this happens against the background of fever and weakness. Fortunately, everything went without complications, I was cured in 2 weeks. Yuri, 47 years old
At first, Covid was mild for me.
I had a slight cough and a sore throat. After 5 days, I suddenly woke up at night because there was not enough air. Immediately called an ambulance. When the doctors arrived, my oxygen was only 88%. It turned out that bilateral pneumonia had begun, although there were no special symptoms. I was treated for a long time, almost 3 weeks in the hospital, and another 2 weeks at home. I still feel short of breath when I walk fast and exercise, although I do breathing exercises and go to physiotherapy. Maxim, 36 years old
I was sick with coronavirus pneumonia, but I had no risk factors, so I was treated at home at first.
The doctor advised me to buy a pulse oximeter and measure oxygen 2-3 times every day. For the first 3 days everything was fine, and then shortness of breath began, the indicators began to drop to 91-92%. I had to go to the hospital, they put me on an oxygen mask for several days, and it was normal to breathe with it. Natalya, 53 years old
Share your opinion or experience - write comments. Did you like the article? – Share it with your friends on social networks.
Lack of oxygen in the blood is a common problem with coronavirus infection, which occurs due to damage to the lungs. The pathology is manifested by shortness of breath, bluish skin, tachycardia, dizziness and fainting. Portable pulse oximeters and fitness trackers are used to monitor saturation levels at home. If the indicators decrease to less than 94%, different types of oxygen support are indicated, and if oxygenation drops to 80%, the patient is transferred to mechanical ventilation.
How to measure saturation with a pulse oximeter
Every person will be able to buy a device for measuring saturation on a finger - a pulse oximeter, for the purpose of monitoring it at home. It is visually similar to a clothespin.
As mentioned above, it is fixed on the finger. Within 60 seconds, the sensor built into the device reads and analyzes the data. The pulse oximeter is equipped with a display that displays two numbers. One shows the percentage of oxygen, the second shows the pulse.
PRbpm (pulse rate beats per minute) on a pulse oximeter shows the strength of the pulse, measured in the number of beats per minute.
In medical institutions, invasive equipment is used to obtain the gas composition of biological material.
Pulse oximeter errors
The device may provide inaccurate data in the following cases:
- low quality device;
- the battery is not charged or the batteries are exhausted;
- measurements are performed immediately after physical activity;
- nails are decorated with a decorative coating;
- fingers are cold;
- There is a mask on the face, the material of which does not allow air to pass through.
To obtain correct results, it is important that the device is of high quality - it is better to buy a pulse oximeter from time-tested manufacturers. Measurements should be taken at rest. If a person walked or did homework before the test, the body should be given time to rest.
Oxygen saturation rate
The norm for the normal functioning of the lungs and other organs is a saturation rate of 100% .
However, this parameter depends on the organism. So, with anemia, chronic pathologies of the respiratory and cardiovascular systems, it may be lower. Age and the presence of bad habits, such as smoking, also matter.
At night, the indicator decreases, and the difference with the norm can be impressive. Thus, in patients with chronic lung diseases, the body has managed to adapt to the lack of air, and saturation during night rest can drop by 10%.
According to statistics compiled from the observations of medical specialists who work with patients with coronavirus, the peak of the decrease occurs between three nights and seven in the morning. This is the most dangerous time for people who become ill – during this period the highest number of deaths is recorded.
What is the norm of saturation in adults table
It should be borne in mind that the oxygen norm is a relative concept. It happens that people who have signs of coronavirus measure it, and the results obtained, for example 95%, cause panic - the person calls an ambulance.
Normal saturation in adults (table)
The normal oxygen level is arbitrary. Often, patients who exhibit symptoms of the disease panic and call emergency help when the saturation rate is 95%. According to medical data, the conditional norm depends on various parameters:
- In healthy people, the norm is from 95 to 98%.
- For smokers - from 92 to 95%, while the parameter decreases when consuming alcoholic beverages, coffee, and energy drinks.
- For chronic pathologies of the respiratory system - from 92 to 96%.
- In children in the first months of life – 93-97%.
With coronavirus, oxygen support is needed in the following cases:
- If the rate is less than 93%, the person feels short of breath, has a cough and a runny nose.
- Computed tomography shows lung damage - 50%.
- An elderly patient has symptoms of the disease.
- Low saturation – less than 90%.
- During pregnancy.
- Hospitalization is required for patients with immunodeficiency.
- Patients who are overweight and have diabetes also need medical attention.
If a hospitalized patient has a low reading that cannot be normalized with oxygen, he or she is transferred to the intensive care unit for tracheal intubation.
Why can pulse oximetry data be misleading?
It is important to understand that the result of pulse oximetry can be influenced by: the sensitivity of the device (including battery charge), lighting, and the color of the patient’s skin (the darker, the higher the indicator, which does not reflect the real state of affairs).
The concept of “saturation rate” is very arbitrary. It happens that patients with signs of coronavirus infection and a mobile non-invasive device for measuring saturation begin to panic and call an ambulance if the oxygen in the blood drops, for example, to 93%. To do this, let’s look at the data from the conditional norm table:
Saturation with coronavirus
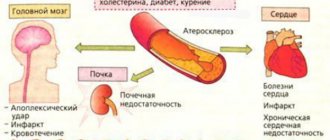
Coronavirus disease is characterized by powerful and comprehensive damage to the main respiratory organ – the lungs. The alveoli are primarily affected - single cells that perform gas exchange between the air entering the lungs and the blood that carries oxygen to the cells of the body.
The alveoli and their septa are blocked by the virus and become inflamed, as a result of which their useful work is reduced to zero in a short period of time. Inflammation spreads to neighboring alveoli, and the affected area increases. As a result, the volume of oxygen entering the body per unit of time continuously decreases.
The condition gradually or quite sharply (over 3-5 days) worsens, the state of health is subjectively assessed with the epithets “tired” or “exhausted”, and cold symptoms appear.
The important thing is that the victim does not know about the fact of infection until a state is discovered in which the body is already exhausted, and the volume of lesions in the lungs can lead to disaster.
Oxygen saturation during coronavirus is a criterion for the degree of damage to the body. If the value is too low, immediate medical attention is required, including connection to a ventilator.
What it is?
Saturation in medicine is the oxygen saturation of the blood, measured as a percentage and denoted as SpO2. Its values are very important because they indicate problems with respiratory and cardiac activity even before the first signs of oxygen deficiency appear. In the body there is a continuous exchange of gases between blood cells and tissues. The blood is saturated with oxygen in the lungs and carries it to the tissues. The latter, in the process of exchange, give up waste generated as a result of respiration and “exchange” carbon dioxide for oxygen.
Carbon dioxide, in turn, is transported by the blood back to the lungs, from which it is released when exhaled. At the same time, space in the red blood cells is freed up and immediately occupied by oxygen. This is the cycle of gases, which is the respiratory cycle. Gas exchange occurs due to the penetration of gases into hemoglobin molecules, binding to it through an iron molecule in its composition.
Hemoglobin forms red blood cells, which give blood its characteristic red color.
Saturation is measured with a special device - a pulse oximeter, including its varieties for home use, and fitness bracelets. However, the latter may show less accurate figures. At low blood oxygen saturation values, an artificial lung ventilation device is connected. Initially, ventilation is performed by inhalation through a mask or nasal catheter; if this is not enough, tracheal intubation is performed with the installation of an endotracheal tube or an ECMO procedure - extracorporeal membrane oxygenation.
What to do if saturation is low
If the saturation has dropped, this is not a reason to panic. The indicator can be quickly returned to normal, and even an indicator in the region of 70-80% is not a threat to life. At the same time, those who suffer from chronic lung diseases also have a chance to recover, since the body is adapted to the lack of oxygen.
If coronavirus is diagnosed and the parameter has decreased by 5, 6, 10, 15%, and the measurements were performed correctly (it is important to make sure that the device is charged), you should call an ambulance.
Measures taken by the doctor
How to normalize saturation yourself
Before the ambulance arrives, a person can raise their oxygen level through simple gymnastics:
- Having previously relaxed, you should raise your hand and touch an object, for example, a door handle. In this case, the second hand rests on the chest. The person takes deep breaths, raising the chest.
- Sit down, raise your hand, and extend the other one forward. Taking a deep breath, turn in the direction opposite to your raised arm.
You should also ensure a flow of fresh air by ventilating the room. In general, doctors who have worked with patients with severe forms of the disease note that oxygen support is less effective than breathing exercises. It is advisable that the patient do them under the supervision of medical personnel.
In which organs is the blood saturated with oxygen?
To answer this question, you should first recall the school topic on anatomy “Circle of Blood Circulation.” After all, it is during this process that the body’s tissues are saturated with all the necessary substances and oxygen. And this happens in the following way: from the left ventricle, the heart muscle gradually flows through the arteries to all organs of the body. As a result of the large circle, a kind of gas exchange occurs in the capillaries. In other words, oxygen goes from the blood to the tissues, and carbon dioxide comes from the tissues to the blood. In this case, the red cells become venous and enter the right atrium through the vena cava, and then into the right ventricle.
Oxygen saturation of the blood occurs in the lungs.
Almost every schoolchild knows about this. By the way, this element is transferred to all internal organs and tissues not only with the help of our natural pump - the heart, but thanks to special carrier proteins contained in red cells or so-called erythrocytes. In medicine they are usually called hemoglobin. It shows the degree and level of oxygen saturation in the blood.
However, the next question immediately arises about what its norm is. It is worth noting that in the normal state, almost all hemoglobin is associated with oxygen. Moreover, the saturation rate itself varies from 96% to 99%. If this level decreases and becomes less than 95%, then the person experiences severe forms of diseases of the blood vessels, respiratory system and heart muscle. In addition, with severe anemia (that is, with a significant decrease in hemoglobin levels), the patient may notice other changes in the body (for example, weakness, deterioration in the condition of nails, skin, etc.).
Saturation after pneumonia and coronavirus
It is not uncommon for the coronavirus to recede, but saturation remains low. Within the framework of pneumonia, this is considered normal, since the lungs need to be restored. Patients are advised to take a leisurely walk in the fresh air every day, as well as perform breathing exercises.
To prevent the formation of adhesions in the lung tissue, recovered patients whose CT scan showed serious fibrotic changes are prescribed antioxidant treatment, which involves following a diet, consuming acetylcysteine, vitamin E. Monitoring through computed tomography is also necessary.