Blood pressure is the force that hematologic fluid exerts on the blood vessels.
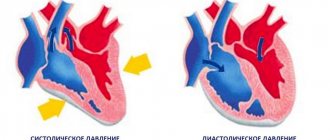
Two indicators play a major role in diagnosing and determining the quality of health: systolic pressure or the upper indicator.
The initial value, determined at the moment of greatest tension in the heart, the lower or diastolic pressure is the blood pressure level at the moment the muscle structures of the organ relax and blood returns.
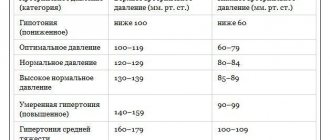
The generally accepted norm today is not the notorious 120 to 80, but a range from 100 to 140 to 60-90. If the tonometer reading is at the upper limit, this is normal, but not always.
How, in such a situation, to assess the level of diastolic blood pressure of 90 mmHg? It turns out that the World Health Organization recognizes such figures as acceptable? Big question.
It's all about the existence of the so-called individual norm. It can vary by 10-15 mmHg, deviating from the reference values.
However, you need to take into account what kind of working, constant pressure a particular person has. If the patient feels normal with a diastolic level of 60-70, then 90 will obviously be too much for him.
In which cases are we talking about the norm, and in which cases are we talking about pathology?
In addition to the individual or working norm for the arterial indicator, you need to keep in mind that there is a physiological increase in pressure. This phenomenon occurs frequently and is not considered a pathology.
In what cases can we talk about a variant of the norm:
- The course of puberty. Teenagers are most susceptible to changes in blood pressure due to hormonal changes in the body.
Puberty or puberty is associated with adolescent or juvenile hypertension; hypotension is possible, but less common.
In such patients, a slight increase in blood pressure is considered quite acceptable, although it requires dynamic observation and control. In which case, correction of the condition with special medications is indicated.
- Pregnant women find themselves in the same situation. The nature of general hemodynamics changes, the entire body is rebuilt to please the fetus. The interests of the mother's body fade into the background. Best case scenario.
Changes in blood pressure, persistent hypertension or hypotension are clinically possible variations in the tonometer reading during gestation. In this case, the condition resolves on its own after childbirth, within 3-4 weeks.
Otherwise, we are talking about a coincidence and we need to look for the reasons for the development of the problem. Pregnant women, even with physiological hypertension of the diastolic type, should be monitored on an ongoing basis. Possible harm to the fetus.
- If the lower pressure is 90-95, the reason may be hidden in age. Thus, patients in the older group are more susceptible to the development of an isolated hypertensive process. Somatic diseases do not always play a role here. A variant of the physiological norm is possible.
- Body type. Patients with a special constitution, strongly built, are more susceptible to developing a physiological increase in blood pressure. This is not considered a pathology.
- Belonging to the female gender. Studies show that the female body is more susceptible to developing elevated blood pressure levels.
There are also other reasons, not of a physiological, but of a subjective nature: long-term smoking, abuse of alcoholic beverages, especially psychoactive substances such as cocaine, which completely destroys the cardiovascular system.
What to do if saturation drops?
Don't panic about low saturation - normal vital signs can be quickly restored, and even a reading of 70% within a few days is compatible with life, and the chances may be even higher if the patient has, for example, chronic obstructive pulmonary disease, and to a low level oxygen, his body has already adapted. Saturation may drop for several days.
However, if during coronavirus the saturation drops to 95%, 93, 90...%, and all measurements are made correctly (it is important to check that the pulse oximeter has an adequate battery level, and that the device itself is registered as a medical device and not purchased from dubious manufacturer) - you need to call an ambulance.
Causes of pathological increase in blood pressure
Often a lower pressure of 90 means that some pathological process is taking place. The type of disease can only be determined through differential diagnosis.
It is impossible to establish the fundamental factor “by eye”; symptoms alone are not enough. When does isolated diastolic hypertension or the classic hemodynamic variant of the disease develop?
Pathologies of the spinal column
With compression of the blood vessels supplying the brain and its individual areas.
Among the record holders are vertebrobasilar syndrome, fibrosis of muscle tissue, and osteochondrosis of the cervical spine. It is not known in advance which scenario the pathology will follow.
The development of isolated hypertension or classical hypertension with an increase in systolic and diastolic values is possible.
It all depends on the intensity of dysfunction of special centers of the brain that regulate vascular tone.
Endocrine diseases
Like hypercortisolism, when too much of the hormone cortisol and corticosteroids are produced.
A similar condition develops as a result of the presence of corticotropinoma (a special hormone-secreting tumor of the pituitary gland), neoplastic (tumor) processes in the adrenal glands themselves.
Possible options include thyrotoxicosis (excess of active substances of the thyroid gland), diabetes mellitus.
Attention:
All hormonal diseases affect the cardiovascular system, increasing the risk of premature death or severe disability.
Pathologies of the cardiovascular system itself
Congestive heart failure, ischemic organ disease. They are accompanied by impaired cardiac output and, as a result, impaired general hemodynamics (blood circulation). The vessels are toned, the speed of blood flow and its efficiency decrease.
History of heart attack
In the early rehabilitation period, an asymmetric increase in blood pressure, including lower blood pressure, is possible.
This is not normal, but it does happen. The phenomenon is observed for 1-3 months. The patient must be monitored all this time.
The patient himself is recommended to take prescribed medications to prevent relapse.
Stroke
Acute cerebrovascular accident such as ischemia (lack of nutrients and oxygen) or hemorrhage (rupture of a blood vessel).
Both processes are dangerous; the outpouring of blood is more life-threatening, since brain death or deep coma is possible.
In the first few months, pressure can “jump” within a wide range. But the diastolic indicator should not rise above 90-95.
This is a threatening sign that requires re-hospitalization and preventive measures. A second stroke is often fatal.
Renal pathologies
Associated with a violation of the filtering function of the paired organ or the process of synthesis of renin (prehormone, the metabolites of which have a hypertensive effect on the body).
They require a serious attitude. In advanced cases, they provoke the development of malignant hypertension, which is difficult to correct even in a fully equipped hospital.
Atherosclerosis
Especially in the form of occlusion (blockage) of the lumen of a vessel with a cholesterol plaque.
Strictly speaking, a plaque is not a single formation, but an entire lipid layer that radially covers the inner lining of the artery.
Over time, the formation calcifies and hardens. Such a “stone” cannot be eliminated with medications. Requires surgery.
Pressure in atherosclerosis often increases disproportionately: the lower is high, the upper is normal.
Pulse pressure (the difference between systolic and diastolic) in this case can be determined by significant numbers: more than 60 mmHg, which is life-threatening.
The causes (etiological factors) allow us to develop a clear therapeutic model.
For a more accurate diagnosis, it is necessary to objectify all symptoms, and then pay attention to those that may be related to the hypertensive process.
How to increase saturation after viral pneumonia?
If even after suffering from coronavirus the saturation is slightly reduced, then this is normal - the lung tissue needs time to restore the previous vital capacity of the respiratory organ. Breathing exercises (see Strelnikova’s set of breathing exercises) and walks in the fresh air with moderate physical activity are extremely useful.
To prevent aggressive adhesions in the lungs in patients with fibrous changes evident on CT; usually with CT-4, CT-3, less often with CT-2 and very rarely with CT-1, antioxidant therapy for pulmonary fibrosis is prescribed, which includes a diet enriched with antioxidants, acetylcysteine, and vitamins E (if there are no allergies).
To clarify the diagnosis and causes of reduced saturation after coronavirus, CT control is important.
Is this condition dangerous?
It all depends on the patient’s individual norm, as well as pulse pressure.
According to statistics, complications are more often observed in patients with an isolated hemodynamic variant of hypertension (when one indicator is high and the other is low or normal).
The development of pathology is associated with a number of dangers:
- Total blindness due to hemorrhage into the vitreous body of the eye and subsequent secondary detachment of the retina. It occurs frequently, especially with sudden changes in blood pressure.
Requires vitrectomy (pumping out blood, filling the eye structures with mineral oil or gas to compress the retina and restore the function of the organ of vision), which, unfortunately, few people can do urgently in small towns.
- Heart failure. Often asymmetric hypertension is accompanied by sinus tachycardia. There is no direct connection between these phenomena, but the etiology (root cause) of the pathological processes is identical.
A prolonged increase in heart rate (even if the rhythm is correct) is fraught with cardiac arrest and death of the patient.
- Heart attack. Necrosis of myocardial structures (middle muscular layer of the heart). Ends in death or severe disability without the possibility of restoration of ability to work. Symptoms of a pre-infarction state are described here, and first aid methods are here.
- Stroke. It carries even greater danger. In 70% of cases, patients with the diagnosis are left with a gross neurological defect. In 100% of cases, pathology reminds itself of itself with fewer problems in the future. The hemorrhagic variety leaves the patient less chance of a full life (and life in general).
- Cardiac ischemia.
- Congestive heart failure.
- Hypertensive crisis. An emergency condition with a sharp increase in blood pressure. It is observed in 70% of patients diagnosed with hypertension.
Some may live with the disease for years and never know what a crisis is, while others are not so lucky. May result in the death of the patient. The mechanisms of development, symptoms and first aid for GC are described in this article.
- Impaired cognitive function and early dementia are also likely. The risk of Alzheimer's disease increases.
Why measure saturation during coronavirus?
Coronavirus saturation is measured to quickly detect life-threatening hypoxemia. In this way, the severity of the disease is determined and a decision is made on further actions: hospitalization, oxygen support, computed tomography.
In foreign literature there is the term “silent hypoxemia”, which appeared only recently, during the COVID-19 pandemic, when it became clear that a fairly large percentage of patients were admitted to the hospital with an acute lack of oxygen, disproportionate to the symptoms. It turns out that patients can breathe, do not choke, there is no strong cough and no fever, while the lungs are severely damaged, saturation is critically low, and additional oxygen is needed.
Can a patient with symptoms of coronavirus somehow suspect that he has a lack of oxygen due to pneumonia? Yes.
Is it worth reducing these numbers?
It is better to address this question to the attending physician, who has been caring for the patient for a long time and already knows the characteristics of the patient’s body.
If you are prone to hypotension and have normal readings below 140/90, yes, it’s worth it. How? At home, it is recommended to use only medications prescribed by your doctor.
Dosages should not be exceeded; a sharp drop in blood pressure is just as dangerous as an increase. The same functional disorders are possible, including strokes and heart attacks.
In addition to basic means, the use of herbal preparations with a sedative effect, phenobarbital (Corvalol, Valocordin) in alcohol solutions is indicated. There is no point in taking maintenance pills.
If the blood pressure level increases significantly, above 90 mmHg (diastolic indicator), you need to call an ambulance for urgent help. Initiative in improving health is punishable. No amateur performances.
Is it possible to quickly increase the saturation on your own?
Before the ambulance and oxygen therapy arrive, the patient can take the following measures:
1. Do breathing exercises
Sit up straight, lower your shoulders, straighten up and try to relax.
Exercise 1
- Raise one hand up and grab the floor lamp/beam/door handle to secure the position of your hand.
- Place your other hand on the diaphragm. Breathe deeply, lifting your diaphragm as you inhale.
Exercise 2
- Continue to hold one arm up while keeping the other extended forward.
- As you inhale, turn your body towards your outstretched arm (if your left hand is raised, turn your body to the left and vice versa).
Exercise 3
- Breathe deeply with one arm raised up. The hand is fixed on any object (floor lamp) or wall.
Open the windows and ventilate the room.
Lie on your stomach for up to 30 minutes.
Important! Due to individual anatomical characteristics, elderly patients should not lie on their stomach - compression of the respiratory organ is possible.
There is no evidence that any medications can effectively increase saturation in a coronavirus patient. However, in the absence of individual intolerance and the presence of aspirin in the home medicine cabinet, the use of this drug is acceptable.
The anticoagulant aspirin is associated with a reduction in the need for mechanical ventilation and admission to the intensive care unit, as well as a reduction in mortality in patients hospitalized with COVID-19.
In general, doctors who worked with seriously ill patients have repeatedly noted that oxygen therapy, or rather the constant stay of the patient “on oxygen,” is less effective than breathing exercises. The patient must breathe independently, under the supervision of medical personnel, “kneading” and stimulating the lungs.
Important! Performing the popular exercise with “inflating” balloons is not permissible in cases of lung damage KT-2, KT-3, KT-4 and especially in elderly patients, since the damaged and overstretched pulmonary matrix may simply not withstand the load.
Symptoms that require you to see a doctor
Any manifestation that worries the patient is grounds for a visit to a cardiology specialist. You need to listen carefully to your own body.
If at least one pathological manifestation presented in the list below is observed, you need to go for a consultation with a cardiologist, or even better, call an ambulance for an emergency assessment of the situation:
- Dizziness of a regular nature, up to complete disorientation in space.
- Tinnitus, hearing loss.
- Speech dysfunction that developed suddenly or gradually.
- Visual impairment up to transient (transient) blindness or flickering of floaters, photopsia.
- Decreased cognitive function.
- Low heartbeat, bradycardia-type arrhythmia.
- Headache of unbearable, stabbing nature. Usually localized in the occipital region.
- Nausea and vomiting without signs of relief.
- Increase or decrease in temperature.
- Sudden shortness of breath, even at rest. Moreover, suffocation.
- Facial distortion.
- Muscle weakness, paresis, paralysis, paresthesia.
Perhaps the reason is completely different, but it’s better to be safe.
What is saturation?
Saturation is an indicator of the saturation of blood with oxygen, which comes from the pulmonary alveoli. Together with blood, oxygen is transported to organs and tissues. A decrease in saturation during COVID-19 indicates hypoxemia, the likely cause of which is viral infection of the lungs. The hypothesis can be confirmed or refuted by computed tomography - during a visual assessment of the lungs.
Diagnostic measures
Diagnosis and differentiation of conditions from each other does not present great difficulties. Consultation with a cardiologist is necessary.
At the discretion of the doctor, it is possible to connect an endocrinologist, neurologist and nephrologist. Such “consilium” occurs often.
The list of diagnostic measures is as follows:
- Oral assessment of complaints. Done to identify symptoms. It's important to tell everything. Even if it seems like it's not relevant. It is up to the doctor to judge. Minor facts can turn out to be important.
- Collecting anamnesis (individual and family, since isolated hypertension is often hereditary).
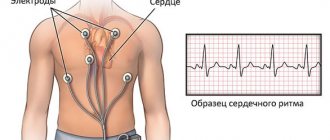
- Heart rate study.
- Measuring pressure on the hands. With short breaks. The degree of asymmetry of indicators on the left and right hands is also assessed, this can lead the specialist to thoughts that are correct from a diagnostic point of view.
- Monitored for 24 hours using a Holter tonometer.
- Electrocardiographic study.
- ECHO-KG.
- Urinalysis, general blood analysis, biochemical analysis.
- Angiography.
- Ultrasound of the kidneys.
- Dopplerography of the vessels of the head and neck.
- Study of hormonal status, neurological profile.
The list can be adjusted taking into account the goals and objectives of the diagnosis.
When else does a person have low saturation?
- For heart defects;
- With hypoventilation of the lungs (with a slowdown in the frequency of exhalations and inhalations);
- For anemia;
- For chronic diseases of the lungs and bronchi (COPD, emphysema);
- If the oxygen concentration in the air is reduced;
- For diffuse disorders;
- Under excessive loads;
- When smoking;
- If you are overweight;
- When there are changes in atmospheric pressure;
- At night (from 3 to 7 o’clock) and in the deep sleep phase;
- When he is under general anesthesia.
Treatment and prognosis
{banner_banstat9}
You can reduce the lower pressure, if it is 90, in different ways. But this is symptomatic therapy. A combination of combating the manifestations and the etiological factor that caused these signs to come to life is required.
Antihypertensive drugs, diuretics, and angioprotectors are used to prevent complications. The main etiological treatment varies from case to case: surgical intervention, correction of hormonal status, etc. are possible.
The prognosis is favorable in most cases. A diastolic pressure level of 90 mm Hg is not so high, if you do not take into account “inveterate” hypotensive patients with excessively low blood pressure levels.
You can live quite a quality life with it. However, it is better to correct conditions before reaching operating levels. This will reduce all risks to nothing.
A lower pressure level of 90 mmHg formally means normal. In reality, this is not always the case. There are a lot of factors to consider. Treatment is etiological and symptomatic, as necessary. Self-therapy is unacceptable.