On the issue of ECG diagnosis of right ventricular myocardial infarction
The article draws attention to the importance of diagnosing right ventricular myocardial infarction. ECG diagnosis of right ventricular myocardial infarction is carried out by removing the so-called additional right chest leads V3R-V6R, which reveals pathological Q, ST segment elevation, negative T. The motivation for removing additional right chest leads are both the features of the clinical picture of the disease and mainly, the presence of ECG signs of inferior diaphragmatic or posterobasal myocardial infarction.
To question about ECG diagnosis of myocardial infarction of right ventricle.
The article pay attention to the importance of diagnostics of myocardial infarction of the right ventricle. ECG diagnosis of myocardial infarction of the right ventricle is carried out when removing the so-called additional right precordial leads V3R-V6R, in this case show pathological Q, rise segment ST, negative T. The motivation for the withdrawal of additional right precordial leads are both features of clinical disease and, mainly, the presence of ECG-signs inferior phrenic or posterobasal myocardial infarction.
Recognition of right ventricular myocardial infarction in widespread practice is casuistic. At the same time, its frequency is about 3%. A large number of patients have simultaneously myocardial infarction of the left and right ventricles, while right ventricular myocardial infarction is especially common in patients with damage to the lower wall of the left ventricle (up to 30% of patients). 13% of patients have a combination of myocardial infarction of the right ventricle and the anterior wall of the left ventricle. At autopsy, combined lesions of both ventricles are detected in 14-84% of the deceased (N.A. Mazur, 2009). Unfortunately (in terms of diagnosis), in patients with right ventricular myocardial infarction there are no clear specific differences in the clinical manifestations of the disease. ON THE. Mazur (2009) notes that some patients experience rapid development of right ventricular failure without stagnation of blood in the pulmonary circulation. At the same time, A.V. Shpector and E.Yu. Vasilyeva (2008) draw attention to the fact that in the acute stage of right ventricular infarction, right ventricular failure is usually manifested not by stagnation of blood in the systemic circulation, which develops later as fluid accumulates, but by hypotension. This is due to the fact that a feature of the mechanics of the right ventricle is its high dependence on preload. And therefore, if a patient with signs of right ventricular myocardial infarction has reduced blood pressure, he needs massive infusion therapy. At the same time, vasopressors are dangerous because, by increasing systemic pressure, they increase the pressure in the vessels of the pulmonary circulation, which sharply increases the load on the affected right ventricle. The volume of required infusion for hypotension associated with right ventricular myocardial infarction often reaches several liters. This is quite safe if there is an isolated lesion of the right ventricle, because with a healthy left ventricle, pulmonary edema does not develop. However, if there is combined damage to both ventricles, then the infusion must be carried out under the control of wedge pressure in the pulmonary artery to avoid overload of the pulmonary circulation. Due to the increased sensitivity of the right ventricle to preload, another feature of the treatment of right ventricular myocardial infarction is extreme caution in the use of nitrates and diuretics (as they reduce preload). Caution is also necessary in the use of morphine in such patients, because morphine has a moderate vasodilating effect.
Is it necessary to use thrombolytics for right ventricular myocardial infarction? No special studies have been conducted on this issue, but there is expert agreement on the advisability of their use, especially in the case of hypotension; Angioplasty is also indicated for patients with right ventricular myocardial infarction. It should be noted that the occurrence of atrial fibrillation in patients with right ventricular myocardial infarction leads to rapid deterioration of the condition; in such cases, urgent electrical cardioversion is necessary.
How is right ventricular myocardial infarction diagnosed in routine clinical practice using an ECG?
It is known that the right coronary artery is the common source of blood supply to both the posterior parts of the left ventricle and the right ventricle. Therefore, up to 1/3 of posterior left ventricular myocardial infarction is combined with right ventricular myocardial infarction. With the extreme right type of coronary circulation, the branches of the right coronary artery can extend to the lateral wall of the left ventricle and to the apex. A.V. Shpector and E.Yu. Vasilyeva (2009) note that 75% of patients with myocardial infarction have multiple lesions of the coronary arteries, which often leads to the development of collateral circulation. At this stage, the extent of myocardial infarction may not correspond to the classical anatomy of the coronary bed. Thus, if the patient had subtotal stenosis of the anterior interventricular artery and the blood supply to its zone was provided largely by collaterals from the right coronary artery, then thrombosis of the right coronary artery can lead to the development of a huge circular myocardial infarction.
Right ventricular myocardial infarction is diagnosed on the ECG using additional ECG leads - the so-called right chest leads: V3R-V4R-V5R-V6R. These leads must be removed in all cases of posterodiaphragmatic and posterobasal myocardial infarction, as well as when the localization of myocardial infarction according to standard ECG leads is unclear (Candell - Riera J. et al., 1981; Wenger N. et al., 1981; Goldberger A., 1984 ; Wagner G., 1994; Shevchenko N.M., 1994; Doshchitsin V.L., 1999; Mazur N.A., 2009). Registration of V3R-V6R or at least V4R in the first hours of the disease is very important for recognizing right ventricular myocardial infarction (N.A. Mazur, 2009).
In order to remove additional right chest leads, the active electrode is applied to the right half of the chest “mirror”, symmetrically with respect to the traditional chest leads (Fig. 1). In this case, electrodes V1-2 are left unchanged, and electrodes V3-6, transferred to the right half of the chest, form the right chest leads.
Figure 1. Additional right chest leads
a - diagram of the application of additional right chest leads
b — application of chest electrodes on the patient
c - ECG taken with left chest leads and additional right chest leads in a practically healthy person
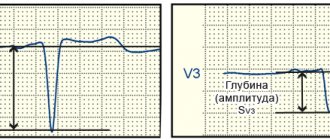
In case of myocardial infarction of the right ventricle, the following changes are detected in the right precordial leads:
1) the presence of ST segment elevation of 0.5-1 mm in these leads is highly specific (however, ST segment elevation in half of the patients persists for no more than 10 hours from the onset of the disease);
2) pathological Q wave; the QRS complex has the form QR or QS (V.L. Doshchitsin, 1999). ON THE. Mazur (2009) notes that pathological Q in the right precordial leads has low specificity;
3) negative T wave;
4) in the case of necrosis of the lateral and anterior walls of the right ventricle, the same changes are recorded when electrodes V3R-V4R-V5R-V6R are applied two ribs above (Lyusov V.A. et al., 2008).
In addition, ST segment depression in leads V2 and aVF has a high predictive accuracy (about 80%); Right bundle branch block and atrioventricular block often occur.
We observed patient Sh., 70 years old, in the 11th city hospital of Kazan with extensive circular myocardial infarction, when an ECG during the first day of hospitalization initially revealed an elevation of the ST segment by 3 mm in leads V1-V4, depression of the ST segment in I, aVL, then a complete block of the right bundle branch developed, and then ST segment elevation occurred in III and aVF. ECG signs of inferior myocardial infarction (ST segment elevation in III and aVF) prompted us to take the right precordial ECG leads. When removing the right chest leads, pathological Q, ST segment elevation and negative T in V3R-V6R were detected, which indicates the development of myocardial infarction in the right ventricle as well.
We present an ECG of patient Sh., 70 years old (Fig. 2).
Figure 2. ECG of patient Sh., 70 years old.
Extensive circular myocardial infarction with a Q wave: myocardial infarction with a Q wave of the anteroseptal region of the left ventricle spreading to the apex and lateral wall of the left ventricle, myocardial infarction with a Q wave of the inferior wall of the left ventricle and right ventricle; complete right bundle branch block
Subsequent selective coronary angiography (at the Moscow Clinical Clinical Center) revealed a right coronary type of coronary circulation. The details of the angiographic study are as follows: left coronary artery - trunk without features, LAD - occlusion in the middle segment, distal LAD is not contrasted, subocclusion of the 1st arterial artery in the proximal section, OB - stenosis of the high-outgoing 1st arterial artery in the proximal segment up to 50%, stenosis of the left artery in the middle segment up to 75%. Right coronary artery - stenosis in the middle segment up to 50%, stenosis of the RV ostium up to 90%, WMA - stenosis in the middle segment up to 90% and 80%. ZMZhV - occlusion in the proximal part, the distal parts are contrasted by intrasystemic anastomoses.
So, with this message we want to draw attention to the issue of ECG diagnosis of right ventricular myocardial infarction. In routine clinical practice, with ECG signs of myocardial infarction of posterior localization, it is necessary to take an ECG in additional right chest leads V3R-V6R, which makes it possible to diagnose right ventricular myocardial infarction when a pathological Q wave, ST segment elevation and a negative T wave are detected in these leads. right ventricular myocardial infarction makes a significant correction in the management of patients with myocardial infarction.
V.N. Oslopov, O.V. Bogoyavlenskaya, Yu.V. Oslopova, M.A. Makarov, R.T. Khabibullina, M.G. Tregubova
Kazan State Medical University
City Clinical Hospital No. 11 UZ Kazan
Bogoyavlenskaya Olga Vladimirovna - Candidate of Medical Sciences, Associate Professor of the Department of Propaedeutics of Internal Diseases
Literature:
1. Mazur N.A. Practical cardiology. - M.: Medpraktika-M, 2009. - 616 p.
2. Shpector A.V., Vasilyeva E.Yu. Cardiology: clinical lectures. - M.: AST: Astrel, 2008. - 765 p.
3. Candell-Riera J., Figueras J., Valie V. et al. Right ventricular infarction. Relationships between ST segment elevation in V4R and hemodynamic, scintigraphic and echocardiographic findings in patients with acute inferior myocardial infarction. - Am. Heart J., 1981. - V. 101. - P. 281.
4. Wenger NK, Mock MB, Ringqvist I. Ambulatory electrocardiographic recording. — Chicago: Year Book Med. Publ., 1981. - 456 p.
5. Goldberger AL Myocardial infarction. Electrocardiographic differential diagnosis: 3rd ed. —St. Louis: Mosby, 1984. - 336 p.
6. Wagner GS Marriot's practical electrocardiography. 9th ed. - Baltimore: Williams & Wilkins, 1994. - 434 p.
7. Shevchenko N.M. Fundamentals of clinical electrocardiography. Qualification tests for ECG interpretation. - M.: Overley, 1994. - 156 p.
8. Doshchitsin V.L. Clinical electrocardiography. - M.: Medical Information Agency, 1999. - 373 p.
9. Lyusov V.A., Volkov N.A., Gordeev I.G. Myocardial infarction. In the book: Guide to Cardiology: Textbook in 3 volumes / ed. G.I. Storozhakova, A.A. Gorbachenkova. - M.: GEOTAR-Media, 2008. - T. 1 - P. 514-515.
Journal "Emergency Medicine" 1(20) 2009
Isolated right ventricular myocardial infarction (RMI) is extremely rare, but in the group of patients with acute posterior infarction, concomitant right ventricular damage is detected by ECG data with a frequency of 30–50% [1, 2]. The combination of posterior infarction with UTI is more often observed in elderly people and is associated with an increase in in-hospital mortality and the number of complications. Approximately 5% of patients with right ventricular infarction develop cardiogenic shock with a high risk of death [3]. Management of patients with hemodynamically significant VRT differs from that adopted for isolated left ventricular lesions and includes limiting the use of vasodilators and diuretics, volume loading, inotropic support, control of rhythm and heart rate [4]. To select the optimal patient management tactics, early recognition of UTI is extremely important.
This report presents a clinical observation of a hemodynamically significant right ventricular infarction in a patient with acute posterior myocardial infarction. In this case, timely detection of UTI significantly influenced the treatment strategy and made a certain contribution to the favorable outcome of the disease.
Patient G., 66 years old, was delivered to the clinic as an emergency on July 17, 2005 at 12:10, 2 hours after the appearance of intense burning pain in the chest. Pain of this nature appeared for the first time, for no apparent reason, was accompanied by general weakness and did not decrease after taking 2 tablets of nitroglycerin, which forced the patient to seek medical help. There is a history of increased blood pressure to 160/100 mm Hg. for 3 years, smoking experience for more than 20 years.
The ECG recorded by the ambulance team 50 minutes from the onset of the pain syndrome (Fig. 1) shows signs of acute posterior phrenic myocardial infarction, subendocardial ischemia of the apical-lateral sections of the left ventricle; escape rhythm of the atrioventricular (AV) connection with a heart rate of 46/min, complete right bundle branch block (RBBB).
At the prehospital stage, nitroglycerin, no-spa, analgesics (analgin, omnopon), dexamethasone and mezaton were administered, after which the patient was taken to the ICU of City Clinical Hospital No. 8 in Kharkov with a diagnosis of coronary artery disease, acute myocardial infarction of the posterior wall of the left ventricle. Cardiosclerosis. GB III Art.
Upon admission to the ICU, the patient's condition is serious. Lethargy, acrocyanosis, and cold extremities were noted. There is vesicular breathing over the lungs, isolated dry rales. Respiratory rate 16/min. Heart sounds are muffled, blood pressure 80/60 mm Hg, severe bradycardia (heart rate 42/min). The liver is not enlarged. There is no peripheral edema. According to laboratory data, leukocytosis was 11.7 x 109/l, aneosinophilia, hyperglycemia (blood glucose 9.0 mmol/l), a slight increase in creatinine level (166 μmol/l).
In order to stabilize hemodynamics, atropine 1 mg was administered intravenously, then prednisolone 60 mg, dopamine infusion and inhalation of humidified oxygen were started. Aspirin was prescribed at a dose of 325 mg, enoxaparin 80 mg subcutaneously 2 times a day. At 12:20, 2 hours 20 minutes after the onset of anginal pain, thrombolysis was performed with streptokinase - 1.5 million units as an intravenous infusion over 50 minutes.
As a result of the therapy, it was possible to completely relieve the pain syndrome. ECG dynamics confirmed the effectiveness of the thrombolysis performed.
The ECG taken at 15:35 shows a significant decrease in the ST segment displacement in all leads, the beginning of the formation of a negative T wave in leads III and aVF. There are no pathological Q waves. Bradycardia persists, the replacement rhythm of the AV junction with a heart rate of 42/min, complete blockade of the PNPG. In leads II, III and V6, individual P waves are detected, not associated with QRS complexes, the frequency of sinus impulses is 40/min (Fig. 2).
However, despite the presence of signs of reperfusion, the ongoing infusion of dopamine and repeated administration of atropine, the patient’s general condition remained severe, the clinic of cardiogenic shock persisted (arterial hypotension with a blood pressure level of 70–90/40–60 mm Hg, signs of peripheral hypoperfusion, anuria ). Based on clinical data, hemodynamically significant right ventricular myocardial infarction was suspected. To test this assumption, an ECG was recorded with additional right chest leads.
An ECG taken at 4:00 p.m. maintains the rhythm of the AV junction with a heart rate of 43/min. The disappearance of PNPG block changes the repolarization pattern in lead V1, where the initial downward depression of the ST segment is replaced by its significant elevation. Registration of additional leads on the right side of the chest reveals a pathological form of the ventricular complex in the form of QS from V3R to V6R and significant, up to 3 mm, ST segment elevation in all right chest leads (Fig. 3). Identification of UTI required a change in patient management tactics: 1 ) a volume load was undertaken under the control of hemodynamic parameters (BP, central venous pressure) in the form of intravenous administration of 1100 ml of liquid - 900 ml of physiological sodium chloride solution and 200 ml of rheopolyglucin); 2) in parallel with the administration of fluid, dopamine infusion was continued; 3) electrical cardiac pacing (PAC) was started to eliminate pathological bradycardia. As a result, after 2 hours the blood pressure increased to 100/60 mm Hg, and by morning - to 130/80 mm Hg.
On the ECG on July 18, 2005 at 09:00 - pacemaker rhythm, asynchronous ventricular stimulation with a frequency of 60/min. No signs of atrial electrical activity. ST elevation in the inferior and right precordial leads (Fig. 4).
Due to the increase in the patient's own heart rate to 50–60/min and stabilization of hemodynamics, electrical stimulation of the heart was stopped.
Over the next 3–4 days, the severity of the patient’s condition was due to acute renal failure (ARF), which complicated the course of the disease. The patient complained of nausea and general weakness. In the objective status: slight general cyanosis, dry skin, dilation of the jugular veins. The function of external respiration is compensated, without signs of pulmonary congestion. Increase in blood pressure to 160–170/80 mmHg, heart rate 60–80/min, increase in central venous pressure to 240–270 mmHg. The liver is enlarged - the lower edge is 4 cm below the costal arch, painful on palpation. There was no peripheral edema. Oligoanuria (from July 18 to July 21, the volume of urine excreted per day was 0–250–300–1000 ml, respectively).
During this period, according to laboratory data, hyperazotemia was observed (the level of plasma creatinine from 19.07 to 22.07 increased from 475 to 896 μmol/l), an increase in the level of liver enzymes (as of 19.07 ALT - 2.64 mmol/h l, AST - 2.01 mmol /h·l, without decrease by 22.07); leukocytosis 16.0 x 109/l, aneosinophilia, neutrophilia with a shift of the formula to the left on July 19, with positive dynamics by July 22 in the number of leukocytes and formula, but with an increased ESR. Clinical urine analysis: specific gravity 1010, proteinuria 0.6 g/l, leukocytes - thick, erythrocytes - throughout the entire field of view. The patient was examined by a urologist: a prostate adenoma was detected, which did not require catheterization of the bladder. X-ray of the chest organs 20.07: pulmonary emphysema, diffuse pneumosclerosis. Left ventricular hypertrophy. Significant expansion of the aorta with atherosclerosis and severe calcification of the walls.
Therapy was supplemented with intravenous bolus and then drip administration of furosemide up to 160 mg/day against the background of infusion of dopamine solution in diuretic doses. Detoxification therapy was carried out (reosorbilact, glucose solution with insulin, soda enemas).
On the ECG recorded during this period, attention was drawn to the unusual shape and duration of the P waves, however, the low voltage of the atrial waves during standard ECG recording made it difficult to analyze their configuration.
ECG on July 20, 2005 was taken with additional amplification (1 mV = 2 cm): sinus rhythm with heart rate 60/min, 1st degree AV block. Signs of atrial infarction in the form of elevation of the PQ segment, especially distinct in leads II, III and aVF (Fig. 5).
The next stage of the disease (from July 22 to July 26, 2005) is associated with the resolution of acute renal failure. On these days, against the background of polyuria (2500–3000 ml of urine per day), there was a decrease in central venous pressure to normal and reduced levels (50–100 mm H2O) with the development of tachycardia up to 100–120/min, and moderate arterial hypertension persisted. Positive dynamics of laboratory parameters were observed, namely a decrease in azotemia (07/25/2005 - creatinine 412 µmol/l, urea 24.4 mmol/l), normalization of liver enzymes, decrease in proteinuria and the number of urinary sediment elements.
On the ECG recorded on July 25, 2005 before the patient was transferred from the ICU: sinus rhythm with heart rate 86/min, duration of the PQ interval = 0.20 s. Subacute stage of Q-positive posterior diaphragmatic MI. Complete blockade of PNPG.
Infarction of the right ventricle and atrium was verified by echocardiography on 08/04/2005: significant dilatation of the right atrium was detected - 5.2 cm, zones of hypo- and akinesia of the free wall of the right ventricle with a tendency to increase its cavity, hypokinesia of the basal posteroseptal segments of the left ventricle with normal sizes of the left chambers of the heart (left atrium - 3.4 cm, end-diastolic size of the left ventricle - 4.6 cm, end-systolic size of the left ventricle - 3.4 cm, myocardial thickness of the posterior wall and interventricular septum - 1 cm) and relatively preserved systolic function of the left ventricle (ejection fraction - 51%).
In the infarction department, the patient received beta-blockers, statins, and antiplatelet drugs. There were no complaints, the condition was assessed as satisfactory, the expansion of the motor regime was tolerated well.
During a scheduled ECG on 08/05/2005, an irregular form of atrial flutter with a varying degree of AV block was recorded: 2: 1–4: 1. Complete block of PNPG. Subacute stage of extensive posterior phrenic myocardial infarction involving the right ventricle (Fig. 6).
On the 19th day of illness, 08/05/2005, the patient was transferred to the rehabilitation department in satisfactory condition.
In conclusion, I would like to note some features of the presented case. First, the patient's acute posterior myocardial infarction was accompanied by URI, sinus node dysfunction, atrial infarction, and atrioventricular block. This complex of disorders is characteristic of proximal occlusion of the dominant right coronary artery and is associated with a high risk of developing cardiogenic shock and death. Timely recognition of right ventricular infarction and correction of the therapy allowed the patient to survive the critical period of cardiogenic shock, and the long-term prognosis of such patients is the same relatively favorable as with a posterior infarction without involvement of the right ventricle [5]. This is due to the fact that acute ischemic injury to the right ventricle does not actually always result in necrosis and its function is usually completely restored over time [6, 7].
Another feature of the patient was the development of acute renal failure, the severity of which did not correspond to the duration of arterial hypotension. It can be assumed that kidney damage during the period of cardiogenic shock was aggravated by concomitant atherosclerotic damage to the renal arteries (taking into account the elderly age of the patient, signs of aortic atherosclerosis and coronary atherothrombosis, the recent onset of arterial hypertension and the lack of data on a history of kidney disease).