Myocardial infarction
Diabetes
Atherosclerosis
9062 16 February
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Myocardial infarction: causes, symptoms, diagnosis and treatment methods.
Definition
Myocardial infarction (MI) is the necrosis of an area of the heart muscle due to insufficient blood supply with the development of a characteristic clinical picture.
Causes of myocardial infarction
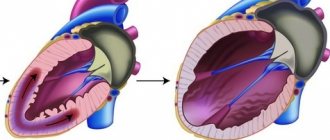
The heart is a hollow muscular organ shaped like a cone. The walls of the heart consist of three layers. The inner layer - the endocardium - lines the cavities of the heart from the inside, and its outgrowths form the heart valves. The middle layer, the myocardium, consists of cardiac muscle tissue. The outer layer is the pericardium. The human heart has four chambers: two atria and two ventricles. The right atrium receives blood from the tissues of the heart itself and all parts of the body (through the superior and inferior vena cava). Four pulmonary veins flow into the left atrium, carrying arterial blood from the lungs. The pulmonary trunk emerges from the right ventricle, through which venous blood enters the lungs. The aorta emerges from the left ventricle, carrying arterial blood to the vessels of the systemic circulation. Oxygen is delivered to the myocardium of the heart through the coronary arteries.
The heart is very sensitive to lack of blood supply (oxygen deficiency). In the case of blockage of a large coronary artery and in the absence of effective alternative blood circulation through other vessels, within 30 minutes the death of cardiomyocytes (muscle cells of the heart) begins in the affected area.
Poor circulation due to atherosclerotic lesions of the coronary arteries in 97-98% of cases is of primary importance in the occurrence of myocardial infarction.
Atherosclerosis can affect either one coronary artery or all three. The degree and extent of narrowing of the artery can vary. When blood pressure increases, the sclerotic inner layer of the vessel (endothelium) is easily damaged, blood penetrates into the plaque, the blood clotting process is activated and a blood clot is formed, which can partially or completely block the vessel.
Where a blood clot can form:
- at the site of rupture of a vulnerable (unstable) atherosclerotic plaque;
- on a defect (erosion) of the endothelium of the coronary artery, not necessarily localized on the surface of the atherosclerotic plaque;
- at the site of hemodynamically insignificant narrowing of the coronary artery.
Coronary artery thrombosis occurs with complete or incomplete parietal occlusion. A thrombus located proximally (closer to the center) in the coronary artery tends to be transported with the blood flow more distally (closer to the vessel wall) and lead to the formation of small foci of necrosis and/or contribute to the expansion of the main area of necrosis.
Great importance in the development of myocardial infarction is attached to the development of spasm of the coronary arteries both with atherosclerosis and with unchanged vessels.
Developing myocardial necrosis can be of various sizes, and necrosis passing through all layers of the heart (transmural) can cause myocardial rupture.
The formation of foci of necrosis in the myocardium is accompanied by changes in the size, shape and thickness of the heart wall, and the remaining myocardium experiences increased stress and undergoes hypertrophy with an increase in volume and mass.
Concomitant conditions such as anemia, inflammation, infection, fever, metabolic or endocrine disorders (in particular, hyperthyroidism) can provoke or aggravate myocardial ischemia.
Risk factors for developing myocardial infarction include:
- hyperlipidemia (violation of the normal ratio of blood lipids);
- smoking,
- diabetes,
- arterial hypertension,
- abdominal obesity,
- psychosocial reasons (stress, depression, etc.),
- low physical activity,
- unbalanced diet and alcohol consumption.
Recurrent myocardial infarction occurs within 28 days of the initial myocardial infarction.
If myocardial infarction develops at a later date, they speak of recurrent myocardial infarction. Classification of myocardial infarction
I. Acute myocardial infarction.
- Acute transmural infarction of the anterior myocardial wall.
- Acute transmural infarction of the lower myocardial wall.
- Acute transmural myocardial infarction of other specified locations.
- Acute transmural myocardial infarction of unspecified localization.
- Acute myocardial infarction, unspecified.
II. Repeated myocardial infarction.
- Repeated infarction of the anterior myocardial wall.
- Repeated infarction of the lower myocardial wall.
- Repeated myocardial infarction of another specified location.
- Repeated myocardial infarction of unspecified localization.
III. Some current complications of acute myocardial infarction.
- Hemopericardium.
- Atrial septal defect.
- Ventricular septal defect.
- Rupture of the heart wall without hemopericardium.
- Rupture of the tendinous chord.
- Rupture of the papillary muscle.
- Thrombosis of the atrium, atrial appendage and ventricle of the heart.
- Other current complications of acute myocardial infarction.
IV. Other forms of acute coronary heart disease.
- Coronary thrombosis not leading to myocardial infarction.
- Dressler's syndrome is post-infarction sclerosis.
- Other forms of acute coronary heart disease.
- Acute coronary heart disease, unspecified.
V. Previous myocardial infarction.
Symptoms of myocardial infarction
During myocardial infarction, as a result of circulatory disorders, metabolic products accumulate in the affected area of the heart, which irritate the receptors of the myocardium and coronary vessels, which is manifested by acute pain. A painful attack leads to the release of adrenaline and norepinephrine from the adrenal cortex.
Pain in the typical course of myocardial infarction is its main symptom. It arises behind the sternum, sometimes it can radiate to the left arm, left shoulder, throat, lower jaw, and to the epigastric region.
In intensity and duration, such pain significantly exceeds a regular angina attack. The pain is not relieved by taking nitroglycerin. The duration of the pain syndrome can vary - from 1 hour to several days. Sometimes myocardial infarction is accompanied by severe weakness, dizziness, headache, vomiting, and loss of consciousness. The patient looks pale, lips turn blue, and sweating occurs.
On the first day of myocardial infarction, tachycardia (rapid heartbeat), rhythm disturbance, and temperature rise to 37-38℃ may be recorded.
In 30% of cases, myocardial infarction in the first hours of its development may manifest itself atypically.
The following clinical options are distinguished:
- asthmatic - occurs as an attack of bronchial asthma (there is shortness of breath, difficulty breathing, a feeling of lack of air);
- gastralgic - characterized by pain in the stomach spreading to the retrosternal space, there may be belching, hiccups, nausea, repeated vomiting, bloating;
- arrhythmic - life-threatening heart rhythm disturbances occur;
- cerebral – characterized by impaired cerebral circulation (nausea, dizziness, impaired consciousness with the development of fainting are observed);
- asymptomatic - myocardial infarction without a typical pain attack. Due to non-compliance with bed rest and lack of proper treatment, the course is unfavorable.
Diagnosis of myocardial infarction
There are clear criteria for diagnosing myocardial infarction:
- clinical picture of myocardial infarction;
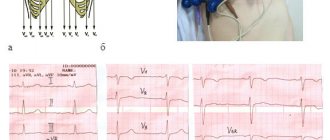
- picture of myocardial infarction according to ECG data;
- the presence of new areas of the myocardium with reduced blood circulation or impaired myocardial contractility according to instrumental studies;
- detection of coronary artery thrombosis according to angiography.
To confirm the diagnosis, the following laboratory tests are performed:
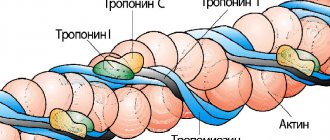
- determination of the level of biochemical markers of cardiomyocyte damage in the blood;
Risk factors
Unchangeable factors include:
- age (risk increases with age);
- gender (in men the risk of heart attack is higher, in women it increases and approaches “male” indicators in the postmenopausal period);
- genetic predisposition (heart disease in close relatives);
- race (for example, African Americans have a higher risk).
Modifiable (changeable) risk factors, i.e. factors that a person can influence:
- smoking (if you smoke, it is important to quit this habit);
- limiting the consumption of alcoholic beverages;
- control cholesterol levels, high blood pressure, diabetes (through proper nutrition, exercise, medications);
- playing sports, any physical activity (walking, cycling, cardio exercises);
- maintaining normal weight;
- a healthy diet (fruits, vegetables, whole grains, lean meats and milk, reducing the amount of salt consumed, eliminating fried and processed foods, foods containing saturated and hydrogenated fats, moderate consumption of sweets and baked goods);
- avoiding stress.
Complications
Complications (or consequences) of a heart attack are associated with damage to the myocardium during a heart attack. These include: heart rhythm disturbances (type 1 arrhythmia can cause sudden cardiac arrest); cardiogenic shock; heartbreak. These complications develop quite quickly and are the main cause of death from heart attack. The prognosis depends on how quickly after a heart attack the patient received first aid, his age, and the severity of the infarction (size and location of the focus of myocardial necrosis).
Diagnostics
The diagnosis of myocardial infarction is established on the basis of the patient's symptoms and complaints, family history, electrocardiographic signs (signs of a heart attack on the ECG) and laboratory diagnostic results (identify certain proteins and enzymes that indicate myocardial damage). Typical blood tests used to diagnose a heart attack include a serum myoglobin test, a troponin test, and a creatine phosphokinase level.
The patient may also be prescribed coronary angiography with a contrast agent to assess the speed of blood flow, the condition of the coronary arteries and identify areas of their narrowing; CT or MRI of the heart - for the same purpose and to assess the structures and function of the organ.
How to give first aid
The main sign of a heart attack is pressing or sharp pain behind the sternum. The patient needs emergency care, so the first action if a heart attack is suspected should be to call the cardiac team.
Pre-hospital assistance:
- Make sure that the victim is not exposed to physical stress.
- Place the patient in bed with the pillows slightly raised under the head.
- Relieve external pressure - take off your shoes, remove your belt or tie, unbutton your shirt collar.
- Provide a flow of fresh air into the room.
- Monitor heart rate and blood pressure. Provide the numbers to the emergency physician.
- Calm the victim, make sure that panic does not increase.
- Give a glass of water to drink.
It is possible to take medications before the team arrives. If a person has previously suffered from angina, he is given the usual drug to improve cardiac circulation. The tablet should be placed under the tongue so that the victim slowly dissolves it. To protect against thromboembolic disorders, the use of blood thinners is recommended. They prevent platelet aggregation and slow down the death of cardiomyocytes.
If there is no consciousness, a weak pulse and unstable breathing, cardiopulmonary resuscitation is performed. This is a complex consisting of indirect cardiac massage and artificial respiration. Its goal is to support life until doctors arrive. To pump blood, rhythmic pressure is applied to the sternum area, and to ventilate the lungs, air is forcibly inhaled into the victim’s mouth while the nose is pinched.