How oxygen is delivered to body cells
Arterial blood is completely saturated with oxygen - it is bright red. Venous blood is depleted of oxygen and is dark red. Oxygen deficiency in tissues is called hypoxia . Oxygen enters the blood and combines with hemoglobin in the alveoli (pulmonary air sacs).
Human heart
Arterial blood is pumped to the tissues of the entire body by the heart . Tissues receive oxygen from hemoglobin supplied with blood through the capillary network. In tissue cells, oxygen “burns” to form carbon dioxide, which returns to the lungs along with venous blood and is exhaled from the body. Hemoglobin in the blood captures oxygen in the alveoli of the lungs, carries out subsequent oxidation and transfers it to all structures of the body. When hemoglobin saturation (oxygen saturation) is reduced, this leads to oxygen depletion of all body cells and weakened immunity. To measure oxygen in the blood at home, there is a wonderful device - a pulse oximeter . One type of device is called Fingertip Pulse Oximeter , which allows you to measure pulse and oxygen in the blood by placing it on the tip of your index finger.
An oximeter is a device for measuring oxygen saturation in the blood. The measurement method is called spectrophotometry .
Doctor of Medical Sciences, Professor of the Department of Phthisiology and Pulmonology of the Medical Faculty of Moscow State Medical University, Sergey Lvovich Babak
Degree of oxygen deficiency relative to saturation (SpO2) - pulse oximeter readings
| Degree | SpO2,% (pulse oximetry readings) |
| Norm | more than or equal to 95% |
| 1st degree | 90-94% |
| 2nd degree | 75-89% |
| 3rd degree | less than 75% |
| Hypoxemic coma | less than 60% |
*Recommendations, the required oxygen flow, the regimen and duration of oxygen therapy for COPD are prescribed by the attending physician! Oxygen therapy at home is carried out using oxygen concentrators under the control of pulse oximeter readings.
— My name is Babak Sergey Lvovich. I am a professor at the Department of Phthisiology and Pulmonology of the Medical Faculty of Moscow State University of Medicine A.I. Evdokimov. I have several questions that I would like to devote the remaining time to. The role of oxygen in human daily life. The fact is that those mechanisms that we usually evaluate as oxidative are impossible without oxygen. Life is built around oxygen.
It exists in different forms. There are concepts of atomic oxygen, and there are concepts of molecular oxygen. The most curious thing is that molecular oxygen in the air in the lungs turns into atomic oxygen, which penetrates the blood and delivers it to the muscles. And already inside the muscles, it actively participates in the craps chain, allowing the body to receive the necessary proteins, fats, carbohydrates and nutrients by oxidizing products entering the body with food, water, liquids, and so on. Therefore, this delivery of oxygen by the lungs to the blood performs the function of gas exchange.
This is the most important function, and in short, why we breathe. We breathe only to maintain the constancy of atomic oxygen inside our body. The human lungs are adapted to inhale air at a pressure of one atmosphere containing 21% oxygen, almost 80% nitrogen and not containing any additional other impurities in the form of smoke, in the form of solid particles, and so on. But having a humidity of no higher than 60% at a temperature of about 22 degrees.
There are so many conditions necessary for the lungs in order to transform molecular oxygen into atomic oxygen and create a constant saturation of arterial blood with oxygen. If a person, for example, smokes or inhales some dust particles, or some other impurity components in the air, then the lungs react very harshly to this and do not allow such people to have an adequate level of arterial blood oxygen saturation. That is, it seems to be fighting to ensure that we still breathe the freshest air without pathogenic impurities or foreign particles. The second very important component that should be discussed when we talk about the role of oxygen in daily human life concerns environmental humidity and temperature.
The fact is that humans are adapted to live and survive in different climatic conditions. In conditions of very high humidity, in conditions of low humidity, in conditions of cold temperatures, in conditions of very hot temperatures. In fact, this is a unique creature with a high adaptive reserve. Almost all pulmonary diseases can be accompanied by the development of respiratory failure.
The essence of respiratory failure comes down to the fact that there is a discrepancy between the need for oxygen and the ability to deliver oxygen to the arterial blood. The partial tension of arterial blood with oxygen is less than 55 ml of mercury or an increase in the partial tension of carbon dioxide in the arterial blood is above 45 ml of mercury. These two parameters indicate that a person has experienced some degree of respiratory failure.
To our joy, there is an indirect method, but it is quite accurate, by which we can also find out what the degree of respiratory failure is. This method is called pulse oximetry. Pulse oximetry reflects the saturation of arterial blood with oxygen in the degree of saturation. This degree can also suggest the degree of respiratory failure, for example, arterial blood oxygen saturation in the range from 90 to 93% corresponds to a partial blood oxygen tension of 60 to 80 ml of mercury. Which corresponds to zero degree of respiratory failure.
The parameter of reducing blood saturation to 85% will correspond to the first degree of respiratory failure or a reduction to the level of 50 ml of mercury. A parameter of up to 80% blood saturation usually corresponds to the second degree of respiratory failure and 75% below blood oxygen saturation corresponds to the third degree of respiratory failure. It is believed that no matter how the patient feels, the degree of saturation of arterial blood with oxygen
should not be below 90% arterial blood oxygen saturation. The disease will proceed differently in a person if his arterial blood oxygen saturation is below 90%, that is, a certain degree of respiratory failure will occur.
What diseases are usually accompanied by respiratory failure? First of all, obstructive pulmonary diseases. These include bronchial asthma, they include obstructive bronchitis, they include chronic obstructive pulmonary disease, they include bronchiectasis, they include cystic fibrosis. How common is respiratory failure in the population?
It is impossible to give a direct answer here. Because we are talking about the prevalence of the disease, not the prevalence of the syndrome. Respiratory failure is a syndrome and it is quite difficult to separately calculate the prevalence of the syndrome. If we are talking about the comparison of diseases in which respiratory failure can occur, then this is almost 80% of all pulmonary diseases we encounter among the human population.
Therefore, we can say that the data is extrapolated from the given blood. To say that respiratory failure is a common phenomenon in obstructive pulmonary diseases. What underlies the development of respiratory failure? Primarily there are two main mechanisms. The mechanism of narrowing of the bronchi and the impossibility of bleeding out air containing 21% oxygen and the second mechanism is very important, this is the impossibility of oxygen penetrating through the alveolar membranes.
Here are the two main components influencing the development of respiratory failure. Therefore, we divide it into two different types that occur with obstructive pulmonary diseases, which occur with interstitial lesions of the lung tissue. Let's try to decipher the obstructive component of the development of respiratory failure. What is this connected with? First of all, it is due to the fact that in a number of diseases there is a narrowing of the lumen of the bronchial tree, a narrowing of the lumen of the bronchial tubes.
It's caused by bronchospasm, it's caused by swelling, mucus buildup. These three mechanisms lead to a narrowing of the lumen and the impossibility of air entering the respiratory tract. Therefore, even under normal conditions, when there is enough oxygen in the air to ensure the gas exchange function, it physically cannot penetrate the lower part of the respiratory system and saturate the blood with oxygen. Due to the fact that the development of certain respiratory volumes necessary to maintain the gas exchange function is not achieved.
The second situation is completely different; it is associated with intersocial lesions of the lung tissue. When tidal volume is reduced due to compression of the lung. The lung seems to be compressed a little on one side, and on the other side the membranes thicken and oxygen, at a pressure of one atmosphere, cannot penetrate through the membranes and penetrates worse than it should penetrate, cannot adequately saturate the arterial blood with oxygen. In both cases, increasing the concentration of the oxygen mixture supplied to the lungs leads to a very interesting effect.
Oxygen penetrates into the blood at a higher rate and practically the person loses respiratory failure. Therefore, we are talking specifically about devices in this case that are capable of creating an increased concentration of oxygen in the exhaled mixture; they are called an oxygen concentrator. A separate category is respiratory failure caused not by the oxygen component, but by the accumulation of carbon dioxide, it is called hypercapnic respiratory failure.
The first type of respiratory failure that we talked about before is called hypoxemic or hypoxic respiratory failure, where oxygen does not penetrate into the blood, low concentrations. And the second type of respiratory failure is called hypercapnic, associated with the accumulation of carbon dioxide. The culprit of the protogynesis of the development of this type of respiratory failure is precisely the respiratory muscle. A person cannot physically create an excursion adequate to the need for air oxygen to penetrate the respiratory tract.
This is usually associated with neuromuscular diseases, very often associated with obesity or with damage to the skeletal structure of the chest. Also plays an important role in the expansion of the lungs. How does respiratory failure manifest itself clinically? First of all, a person feels a feeling of lack of air, which has an organic name - shortness of breath. Shortness of breath occurs at rest, shortness of breath occurs during physical activity, so we grade this shortness of breath on a certain scale. We assign a point score, the higher the score, the more severe the person’s shortness of breath
In total, the scale provides four points, starting from two points, shortness of breath is chronic and is a reason to seriously think about the causes of such shortness of breath. Clinical shortness of breath manifests itself, if you look at such a patient with shortness of breath, you will see that there is usually bluish skin, blue lips, and often puffs.
True, in some diseases , chronic obstructive pulmonary diseases, in which shortness of breath is very characteristic, we even distinguish two different phenotypes of such a disease. One phenotype is called pink puffing patients, and the other is called blue panting patients. The pink ones that puff are called Pinkpuffers, and the blue ones that pant are called Blue Blowers.
So, Blue Blowers usually have a hypoxemic type of respiratory failure, they are cyanotic, the air supply is very useful for them. Pink-puffing patients more often have a hypercapnic type of respiratory failure with CO2 accumulation and oxygen in this case is not very useful. But on the contrary, it is necessary to have ways to strengthen the disabling part. That is, by changing the ventilation of the lungs in order to flush out CO2 in such patients, since the accumulation of oxygen in the blood causes an increase in the level of CO2 in the blood.
Frequency and seasonality of diseases causing respiratory failure. If we talk about the frequency and seasonality of these diseases, then, in my opinion, these diseases should still be divided into two main categories: obstructive diseases and restrictive diseases with damage to the lungs. If we are talking about the obstructiveness of the disease, then of course, first of all, they are associated with changes in humidity and ambient temperature.
Since this leads to the fact that sputum can swell in the lumen of the bronchus and clog small bronchi, this causes disturbances in the flow of air through the bronchial tree. Therefore, patients usually have chronic obstructive bronchitis twice a year. COPD has this type of exacerbation associated with climate change. A very important component influencing the frequency of exacerbations is continued smoking; such patients have obstructive diseases.
Regular inhalations of toxic gases and fumes support very pronounced inflammation in the respiratory tract and it overlaps with the course of treatment of the disease itself, causing an increase in the frequency of exacerbations. In this case of exacerbation of the disease, there is a sharp increase in shortness of breath, an increase in the secretion of sputum mucus more than usual, this causes the patient to begin to choke and experience varying degrees of respiratory failure.
With which he usually comes to our hospital or is subject to treatment at home. Seasonality in this case is not as important as maintaining those factors that can maintain inflammation of the respiratory tract. The situation is completely different with such an obstructive disease as bronchial asthma. This is a separate category of patients who are usually allergic and have hay fever, and at the moment of flowering of herbs, plants and flora, to which they react very sharply, they experience an exacerbation of bronchial asthma.
Exacerbations are associated specifically with the allergic component, and much attention is paid to the concept of a hypoallergenic regime in patients with asthma, maintaining this and combating hay fever or a reaction to flowering plants, all kinds of herbs, trees, and so on. If we are talking about restrictive diseases, such as pulmonary fibrosis, then they have neither frequency nor seasonality of exacerbation, the process is associated with something else.
The process is often associated with an additional infection, which the patient can get due to a cold or a viral infection. We are essentially talking about pneumonia, pneumonia. Pneumonia in such patients is very severe and very often patients are tormented by destructive diseases; when they get pneumonia, they get a very pronounced degree of respiratory failure. And they literally die from lack of oxygen in the arterial blood.
It must be said that oxygen is a medicine. Like every medicine, it must be considered as a kind of poison, which is given little by little under certain conditions. Since the principle of doing no harm should work in this case too. You can’t just breathe in a certain volume or flow of oxygen. In this way, you can seriously disrupt the humidity of the respiratory tract and disrupt the structure of the respiratory tract, causing yourself serious harm. Oxygen is a powerful oxidizing agent. I would really like our listeners and viewers to remember that the ozone you are talking about: “It’s very good to breathe ozone.”
- This is a big deal! Tragic mistake! There are many people who specially ozonate the room, creating so-called three-molecular oxygen. They damage the pulmonary apparatus so severely that they can eventually die from severe damage to the lung tissue from ozone breathing. Therefore, any oxygen therapy requires clear, specific intervention from a doctor.
Flow intensity. What flow intensity should be set in order to achieve success in oxygen therapy?
The oxygen flow should be such that arterial oxygen saturation figures range from 90% to 95% arterial oxygen saturation. If you can achieve this flow of one and a half liters per minute, that is enough. There is no need to increase the flow to 2 liters, 3 liters, 4 liters. If 3 liters are needed for this, conditions must be created so that the patient receives 3 liters. Therefore, in each specific case, there is a titration or selection of the oxygen flow that creates normal blood oxygen saturation figures. It is believed that flows in excess of one and a half liters per minute are unsafe. That is, they require a special air humidification system, since they can dry out the respiratory tract. And it requires warming, because it will lead to cooling of the respiratory tract.
Let me give you a simple example. For example, cooling the respiratory tract by one degree, that is, 37.4 there becomes 36.4. This leads to a decrease in air humidity by 12%. A decrease of 12% actually dries out the mucus, it becomes in the form of crusts, these crusts will never leave the lower respiratory tract, and respiratory plugs form. Or we call it a mucus plug.
Therefore, it is very important that we properly deliver oxygen to the airways. Properly humidify and, if necessary, properly warm the delivered air so as not to cause hypothermia of the respiratory tract. You need to consult a specialist, a doctor first of all, who knows this technology. And set the parameters necessary for this type of treatment.
How to prescribe oxygen therapy, which patients to prescribe and how to choose the right level? There is a concept of diphomysioma test, if the diffusion of oxygen decreases, we see a significant decrease. That is, the percentage of blood becomes below 55 ml. mercury, then long-term oxygen therapy is indicated for such patients. What is the best way to titrate the level of such therapy? During titration, the oxyinter course is used, which allows one to accurately determine the oxygen flow that maintains normal levels of oxygen saturation in arterial blood.
The need for long-term therapy arises in all patients with respiratory failure starting from the second stage. Since at this stage the arterial blood oxygen tension decreases, usually below 55 ml. mercury column. In fact, these are all patients admitted to the hospital with exacerbation of chronic obstructive pulmonary disease, exacerbation of obstructive bronchitis or with severe attacks of bronchial asthma. They will need oxygen therapy.
If we are talking about the duration of such a maneuver, the duration of this technique, it is important to look at the life-sustaining technique and the technique carried out for some time. Naturally, if we expect that the patient’s respiratory function will be restored and gas exchange will be restored, then we will cancel such therapy.
Usually when therapy takes about two, three weeks of oxygen therapy. We carry out this therapy in the hospital and upon discharge the patients do not receive further oxygen. But a number of patients, especially with interstitial lung lesions with severe obstructive disorders, when it is impossible to replenish gas exchange, require lifelong use of this type of therapy.
And then they are forced to use oxygen concentrators at home. This is an important factor in prolonging the life of such patients. It has been studied and shown that the use of an oxygen concentrator at home prolongs the patient’s life by 15-20 years. This is significant for such patients, while the degree and risk of exacerbations are reduced by up to four times.
That is, if a patient has a minor exacerbation per year, using long-term oxygen therapy for virtually the entire year, he does not experience any serious exacerbations of disease requiring hospitalization or a change in the amount of drug therapy.
This is a significant contribution of the duration of oxygen therapy or oxygen therapy to the doctrine of treatment of patients with chronic respiratory failure. There are oxygen concentrators operating in the range from one liter to five liters per minute with a high output concentration. Creating conditions for good saturation of arterial blood with oxygen. They are expensive and the patient does not have the money to purchase such a device; he is limited to simple concentrators that either work unstably, with a low oxygen concentration at the outlet, or do not provide a flow of, say, five to three and a half, four liters per minute.
What does this lead to? It leads to the fact that the real oxygen concentration in the inhaled mixture drops to a very low value and is virtually no different from room air. And we know very well that the patient’s room air is not enough to relieve gas exchange disorders in such a patient. And respiratory failure progresses in such patients, despite the fact that they supposedly use oxygen concentrators in their lives and are treated with the help of concentrators. In this case, we suggest renting an oxygen concentrator; the cost of renting an oxygen concentrator starts from 6,000 rubles per month.
Therefore, it is the reliability, the percentage reliable benefit of oxygen, the wide variation of flows of oxygen devices that allows you to have some maneuver. In order to select for each patient, in each specific case, adequate, reliable oxygen therapy for a very long period of use. One of the companies that has legalized such a line is the Agmung company. Which adopted the doctrine of various oxygen concentrators for various treatment methods.
For example, there is a model line of concentrators for hospitals and home use, for example, where fairly high flows are combined with a very high concentration of the inhaled oxygen mixture.
| Atmung 3L-I (LFY-I-3A) | Atmung 03-C (LFY-I-3A-11) | Atmung 5L-H (LFY-I-5F-11) | Atmung 5L-F (LFY-I-5A-01) |
And there are oxygen concentrators for home use, small, portable, low noise, when the flow ranges from one to three liters per minute.
| Atmung Oxybar | Atmung Oxybar Auto | Armed 8F-1 | Armed 7F-1L |
I note that usually for home use, flows of more than one and a half liters per minute are not used. Therefore, oxygen supplied in a flow of even three liters per minute is twice the patient’s needs, which provides a guarantee of reliability and stability for such patients, even in emergency situations happened at home. It is important to understand that sometimes patients themselves must know how to behave correctly in the current situation. For example, with a feverish patient, he puts a thermometer or thermometer under the armpit or in the mouth and determines the temperature for himself, understands that with a temperature of 37. he behaves according to one, with a temperature of 38 for another, 39 for a third.
Question: — How should a patient with respiratory failure who is receiving long-term oxygen therapy behave correctly?
For this, there are the concepts of pulse oximeters, a small portable device located on the phalanx of the finger, and allowing to measure the saturation of arterial blood with oxygen. So, if the patient feels increasing shortness of breath without receiving oxygen, puts a pulse oximeter on the phalanx of the finger and sees that the pulse and oximetry indicators begin to decrease below 90%. This is a reason to reconsider the scope of such therapy, but in the presence or after consultation with your doctor who prescribed this type of long-term oxygen therapy.
If he feels some kind of ailment, some kind of weakness, fatigue, but pulse oximetry is maintained above 90% of arterial blood oxygen saturation, then there is no need to change the volume of such therapy. These symptoms are associated with another manifestation of the disease, for example, with not receiving a bronchodilator, receiving hormonal therapy, or impaired mucus drainage in the respiratory system, but are in no way associated with long-term oxygen therapy.
Such a simple method of monitoring well-being and blood oxygen saturation makes the patient confident in the regularity and reliability of this type of treatment.
How long does it take to supply oxygen to a person's respiratory tract?
Professor Ludo in the early 80s in France conducted a huge clinical study on a huge sample of patients and it was established. That with long-term oxygen therapy, it is necessary to supply oxygen to the respiratory tract twenty hours a day, at least twenty hours a day, so that respiratory failure undergoes correction.
At the same time, if we reduce the number of hours of oxygen therapy to 15 or less, then this is equivalent to as if we did not conduct such sessions of long-term oxygen therapy at all.
That is, the boundaries of behavior range from 15 to 24 hours a day. And the desired duration is twenty hours during which the patient breathes a certain concentration of oxygen to relieve any degree of respiratory failure.
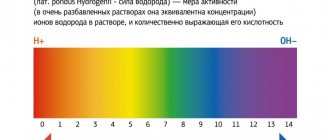
Spectrophotometry
Spectrophotometry (optical spectroscopy) is a method of research and analysis of substances based on measuring absorption spectra in the optical region of electromagnetic radiation.
Spectral analysis
Optical spectroscopy originated in 1802 with the discovery of Fraunhofer lines - dark lines in the spectrum of the Sun, which were described by Joseph Fraunhofer (a German physicist and optician) in 1814 .
In the 60s of the 19th century Gustav Kirchhoff (German physicist) showed that these are absorption lines caused by the presence of various gases in the solar atmosphere, and that a specific line is associated with each gas. In 1853, Anders Jonas Angström (Swedish astrophysicist) compared the emission lines of gases with various chemical elements, which laid the basis for a new method of obtaining information about the composition of substances - spectral analysis .
Joseph Fraunhofer, Anders Jonas Angström, Gustav Kirchhoff.
Absorption spectrum
The absorption spectrum of an object depends on its molecular composition. The Bouguer-Lambert-Beer law is the basic law that describes the absorption of light by a medium. It relates the intensities Il of light passing through a layer of medium with thickness l and the initial light flux I0 .
where kλ is the absorption rate of the substance. For solutions of absorbing substances in non-absorbing solvents, the absorption index can be written as: where: X λ is a coefficient characterizing the interaction of a molecule of an absorbing substance with light of wavelength λ , C is the concentration of the dissolved substance.
Spectrophotometer
The common features of all spectrophotometers are: a light source, a monochromator, a cuvette compartment with a sample, and a recording detector.
Spectrophotometer
The light source is most often mercury or halogen lamps. A monochromator is a device for selecting a narrow part of it (1-2 nm) from the entire emitted spectrum. Monochromators can be built on the basis of light-separating prisms or on the basis of a diffraction grating. Also, some devices may additionally use sets of light filters. The cuvette compartment can be equipped with mechanisms for thermostatting, mixing, and adding substances directly during the measurement process. For studies of small volumes of substances, cellless technology can be used, when the sample is held due to the forces of surface tension of the liquid. The detector converts the light signal into an electrical signal for subsequent processing.
Top of page
a pulse oximeter is used to measure oxygen in the blood at home . To measure, a pulse oximeter is placed on the tip of your index finger. The device measures oxygen levels in both oxygenated arterial blood and oxygen-depleted (deoxygenated) venous blood. And the measurement results are presented as the ratio of these values as a percentage, that is, in SpO2 . To measure these two different types of blood, the device uses light sources of two different frequencies: an infrared light source and a red light source. Infrared frequency is used to measure oxygen-rich blood (arterial blood). The red frequency is used to measure desaturated (oxygen-poor) venous blood. If the highest absorption coefficient is in the infrared range, this means a high degree of saturation (oxygen saturation). And if the highest absorption coefficient is in the red range, then this means a low degree of saturation (oxygen saturation).
Arterial and venous blood
Differences between arterial and venous blood: dark blood flows from the veins, it is thicker, it clots faster, the bleeding is less intense, the stream is smooth and not strained. Venous blood is more suitable for laboratory tests than capillary blood from a finger. It flows through the pulmonary arteries, and in the capillaries of the alveoli it turns into arterial artery.
Which one is darker
Venous blood is darker. Its color depends on the form of hemoglobin. In the arterial blood, it is combined with oxygen (oxyhemoglobin), which gives it a bright scarlet color. The venous contains both oxyhemoglobin and 2 other forms:
- reduced (gave oxygen to cells, but has not yet added carbon dioxide);
- carboxyhemoglobin (a compound with carbon dioxide).
Most of the latter pigment, so the color becomes dark cherry.
Capillary and venous blood: differences
The main differences between capillary blood (from a finger) and venous blood are the contents:
- cells, especially platelets (higher in the venous), leukocytes (higher in the capillary);
- glucose (higher in the veins).
Analysis from a vein is considered more accurate, since it does not contain impurities of tissue fluid or surface epithelium of the skin. Also, circulatory disorders, vascular spasm, and fever can affect the indicators of capillary blood tests. For many types of laboratory diagnostics, a sufficient volume of material is needed, and up to 0.5 ml can be taken from a finger.
Therefore, capillary blood can be used only at the first stage of the examination. It will give reliable results only when determining hemoglobin, red blood cells and ESR. For biochemical and immunological analysis, studies of hormonal levels, as well as, if necessary, an in-depth study of cellular composition, blood from a vein is needed.
Why does venous blood clot faster?
Venous blood clots faster due to high platelet levels. These blood platelets form the basis of the clot, they are connected to each other, and fibrin threads give strength to the formed blood clots.
How to determine the type of bleeding
To determine the type of bleeding, you need to pay attention to the signs that distinguish them:
- Arterial and venous blood: how do they differ in humans?
Through which veins does arterial blood flow?
Arterial blood flows through the veins that leave the lungs to the left atrium. Also, the entire internal venous network of the lungs is filled with hemoglobin, saturated with oxygen. Therefore, the contents in them are exactly the same in characteristics as in the arteries of all other organs (except the lungs).
Where venous blood turns into arterial blood
Venous blood is converted into arterial blood in the capillary network of the alveoli (vesicles) of the lungs. The pulmonary arteries branch into thin capillaries; they entwine the alveolar walls. Carbon dioxide enters the lumen of the pulmonary vesicle, and oxygen from it passes into the blood.
Oxygen molecules join the reduced hemoglobin, which has given up carbon dioxide, and it becomes oxyhemoglobin. Therefore, the blood changes its color and properties - from dark venous to light arterial. Through four pulmonary veins (two left and two right) it goes to the heart.
The operating principle of the device is a pulse oximeter.
The method is based on two phenomena: 1. The absorption of light of two different wavelengths Hb 2. The light signal, passing through the tissue, acquires a pulsating character due to changes in the volume of the arterial bed with each heartbeat. The pulse oximeter has a peripheral sensor that contains a light source of two wavelengths - 660 nm (red) and 940 nm (infrared). The degree of absorption depends on how saturated the blood hemoglobin is with oxygen (each hemoglobin molecule can attach a maximum of 4 oxygen molecules). A photodetector records changes in blood color depending on the oxygen saturation of hemoglobin in the blood. The average filling is displayed by the pulse oximeter monitor.
Pulse oximeter during measurement
The finger is illuminated by light sources and the resulting rays are tracked by a recording device. Some light is absorbed by tissue and blood, and as the artery fills with blood, absorption increases. Likewise, when the arteries become empty, the level of absorption decreases. Since pulsatile blood is the only variable in this problem, static components (i.e. blood and tissue) can be excluded from the calculation. Thus, using 2 wavelengths of light obtained during measurements, the pulse oximeter calculates the oxygenated hemoglobin saturation. One of the types of oximeter - Fingertip Pulse Oximeter BOXYM is shown in the figure above (put on a finger) in the title illustration.
Origin of vascular malformations
Malformations occur in the prenatal period. Geneticists are conducting a lot of research to study this phenomenon, but have not yet come to a definite concept. Therefore, the question of the causes of malformations remains not fully understood.
Congenital angiodysplasia (Parks-Weber-Rubashov syndrome) is characterized by the presence of pathological anastomosis (fistulas) between arteries and veins.
Arteriovenous anastomoses are often multiple and have a variety of sizes and shapes. Depending on the diameter, a distinction is made between macrofistulas, visible to the naked eye, and microfistulas, which are detected only by microscopic examination of the tissues of the limb.
The causes of the development of Parkes-Weber-Rubashov syndrome have not been definitively established. A number of authors consider it to be the result of mutations in the RASA1 gene, which encodes the p120-RasGAP protein, which is involved in the transmission of chemical signals from the extracellular space to the cell nucleus. However, exactly how these changes lead to specific vascular abnormalities in individuals with Parkes-Weber-Rubashov syndrome has not been established.
Pathological anastomosis are most often located in the area of the femoral, branches of the popliteal artery, as well as along the tibial arteries. Intensive discharge of arterial blood through arteriovenous fistulas leads to an increase in blood pressure in the veins.
Due to the increased functional load, the histological structure of the venous wall changes. There is a thickening of its muscular membrane and the formation of an internal elastic membrane (“arterialization” of the vein).
In the presence of fistulas, a significant part of the arterial blood enters the venous bed, bypassing the capillary network, so severe oxygen starvation occurs in the tissues and metabolic processes are disrupted. Due to venous hypertension, the load on the heart increases, which gradually leads to expansion of its boundaries and cardiac decompensation.
Oximeter readings
Blood oxygen saturation level ( SpO2 ) is the ratio of hemoglobin containing oxygen to the total amount of hemoglobin in the blood, measured as a percentage. Here is the range of variation of this parameter: 95% and above – normal 90-94% – I degree, a dangerous level may indicate a health disorder. 75-89% Grade II, extremely dangerous, low blood oxygen saturation, may indicate a serious health disorder. Less than 75% – III degree, hypoxemia. Less than 60% – IV degree, hypoxemic coma.
Pulse oximeter. Measurement result 99%!
Top of page
P.1. What is the circulatory system?
Through the circulatory system, blood is “distilled” by the increased work of the heart, which is the central organ of the system. The human circulatory system consists of a central organ - the heart - and closed tubes of various diameters connected to it - blood vessels . The human circulatory system is a large circle of vessels and a small circle of vessels connecting the heart with all organs of the human body.
Organs of the human circulatory system.
Human circulatory system
Let's start describing the human circulatory system with the main organ that pumps blood through the circulatory system - this is the heart.
Heart.
The human heart (Latin Greek cardia) is a muscular organ (pump) that ensures the movement of blood in the circulatory system.
Human heart
The human heart is capable of pumping 5–30 liters of blood in 1 minute. Over 70 years, the human heart pumps 175 million liters of blood. The average weight of the human heart is 330 grams in men and 250 grams in women. The shape of the heart resembles a streamlined cone, with a wide base, the size of a fist.
Vessels of the circulatory system.
The vessels of the circulatory system are the general name for the pathways through which blood is distributed from the heart and lungs, to all organs of the human body, and returns back to the heart and lungs. Vessels are divided into arteries, veins, and smaller vessels, up to capillaries. Let us consider in more detail the structure of the human circulatory system.
Arteries, veins, their structure and work.
Arteries (red), veins (blue) and their corresponding capillaries
Let us explain some of the terms shown in the figure above: Intima - the inner layer of the vessel. Media – the middle layer of the vessel. Adventitia is the outer shell of the vessel. The vessels of the human circulatory system that carry blood from the heart are called arteries; the initial segment of the arterial system is called the aorta. The aorta is the largest vessel in the entire body, its diameter is 25-30 millimeters. The aorta departs from the left ventricle of the heart, and numerous arteries begin to branch off from the aorta. The farther from the heart, the narrower the vessel becomes. In the thickness of the organs, the vessels pass into the thinnest vessels (arterioles) and further into a dense network of tiny, hairy vessels - capillaries. The vessels that return blood to the heart are called veins. Having entered the right atrium and then the right ventricle of the heart, venous blood is distilled from it into the lungs. In the lungs, venous blood gives off carbon dioxide and is saturated with oxygen, returning back to the heart, to its left atrium. And then, descending into the left ventricle, being pushed out by the force of its contraction into the aorta, it begins a new circuit throughout the body. The artery wall consists of three layers. The inner layer (intima ) is formed from elastic tissue and is lined from the inside with special cells. Elastic tissue allows the vessels to stretch and withstand the pressure of blood, and the endothelium (a single-layer layer of flat cells) makes their inner surface smooth, so blood flows freely without being subject to friction. Friction inside the vessel promotes blood clotting. Arteries and veins, feeding various organs and tissues, themselves need food and oxygen. For the so-called “self-feeding,” the walls of arteries and veins have their own vessels, which have received the figurative name “vessels of blood vessels.” Penetrating through the walls of large arteries and veins, these vessels ensure the vital activity of the circulatory system. In addition, the walls of arteries and veins contain nerve endings connected to the central nervous system, which carries out the nervous regulation of blood circulation. Thanks to this, as much blood flows into each organ as it needs at the moment to perform a particular job. For example, a muscle during exercise receives several times more nutrition than a muscle that is currently at rest. In most organs, the arteries, being distributed into smaller vessels, immediately connect with each other and form a kind of network. Such a device ensures blood supply to the organ even in cases where any part of the vessels, as a result of illness or injury, is switched off from activity. A vessel connecting two other vessels is called an anastomosis or anastomosis. In some organs there are no anastomosis and the vessels directly turn into capillaries. Such arteries that do not have anastomoses are called terminal arteries. When they are damaged, the part of the organ in which they ended stops receiving blood and becomes necrosis, forming a heart attack (from the Latin word infarcire, which means to stuff, to stuff). In cases where in the arteries that have anastomoses, there is any obstacle to the flow of blood, the blood rushes through the lateral, roundabout vessels, called collaterals. And at the site of damage, new vessels begin to form - anastomoses connecting sections of the disconnected arteries or veins. As a result, over time, the impaired blood flow is restored. Thanks to this ability of the body to recreate blood circulation in individual parts of the body, healing of all kinds of disorders occurs.
Capillary network.
Capillary network of the human circulatory system
The capillary network is a system of the finest blood vessels (capillaries) that permeates the entire human body, through which fresh blood reaches every point of the human body, and “waste” is returned for subsequent purification. The capillaries are so small that they are visible only under a microscope. Through their thinnest walls, consisting of only one layer of cells, the “circulation” of blood occurs. Thanks to the dense network of hair vessels, the processes of nutrition of the cells of our body occur. The speed of blood circulation in the body is not the same. And it varies, depending on the thickness of the vessels, almost 1000 times. In the largest vessels (arteries), blood circulates at a speed of up to 500 mm/sec, in large veins – up to 150 mm/sec, and in capillaries – less than 1 mm/sec. Due to the low speed of blood flow in the capillaries, the blood has time to give oxygen and nutrients to the tissues and accept their waste products. The slowdown in blood flow in the capillaries is explained by the fact that their number is huge (about 40 billion) and, despite their microscopic size, their total lumen is 800 times larger than the lumen of the aorta. Connecting with each other, the capillaries gradually transform into small vessels (venules), from which larger vessels of the human circulatory system - veins - are formed. Through them, blood filled with waste metabolic products flows from the tissues and rushes towards the heart.
Top of page
What are arteries
These are vessels that transport oxygen from the heart to the internal organs. By contracting the myocardium, blood circulation is ensured at a speed of 20 cm/s. Purified blood, full of oxygen and nutrients, is necessary for metabolism.
Passing through organ tissue saturates it with carbon dioxide, excreted through venous hematopoiesis.
They are divided into three types:
- diameter;
- structural features;
- topographic principle.
The diameters are:
- large;
- small.
Large in diameter, unlike other components of the vascular system, are: aorta, carotid and subclavian.
The aorta arises from the left ventricle of the heart along the spinal column, dividing into the left and right iliac branches. It begins a large circle of blood circulation, supplying oxygen to the organs and tissues of the body.
General sleep supports the functioning of the brain, providing it with oxygen and microelements necessary for metabolism.
The subclavian vessel supplies blood to the occipital parts of the brain, medulla oblongata, cerebellum and cervical spine. The left arch departs from the aorta, bending around the pleura and, passing through the upper aperture of the chest, exits to the neck and lies in the space of the first rib.
Arterioles are small in diameter. Their task is to regulate blood flow in the SMC.
- Why do the veins in the arms hurt in the elbow bend?
Arteriolar tone determines peripheral resistance, which, along with the stroke volume of the heart, affects blood pressure.
There are three types:
- elastic;
- muscular;
- mixed.
The first type includes mainly the aorta. Its structure is characterized by the predominance of elastic fibers over muscle fibers.
The muscle type contains smooth muscle fibers and is characterized by a weak outer elastic membrane. An example is arterioles.
The muscular-elastic type is distinguished by the presence of muscle and elastic fibers in the structure of the vessel.
P.2. Movement of blood through blood vessels.
The entire blood path is divided into two private sections: the systemic and pulmonary circulation. The diagram of the circulatory system is shown in the figure below:
Diagram of the circulatory system
The great circle is the path from the heart to the organs of the body and back. Otherwise it is called bodily. The great circle begins with the aorta (1), emerging from the left ventricle of the heart (2). Scarlet blood, having passed through the capillaries of the organs (the diagram shows the capillary network of the stomach (3)), becomes dark and returns through the veins to the right atrium of the heart (4). The small circle is the path that blood takes through the lungs. That's why it is called pulmonary. The small circle starts from the right ventricle of the heart (5) and passes only through the lungs (6). In the lungs, the blood releases carbon dioxide and, saturated with oxygen, flows to the left atrium (7). On the left is shown the structure of the walls of an artery (8), vein (9), and also the capillary network (10). The large (corporeal) circle provides nutrition and respiration of tissues, and the small (pulmonary) circle allows the body to get rid of carbon dioxide and supplies the blood with oxygen. The constancy of such blood movement is primarily due to the four-chamber structure of the heart and the activity of the valves located between the atria and ventricles.
The path of blood movement.
Movement of blood in the human body
The entire path of blood is divided into two private circles: the major and minor circles of blood circulation. The great circle is the path from the heart to the organs of the body and back. Otherwise it is called bodily . The great circle begins with the aorta ( 1 ), emerging from the left ventricle of the heart ( 2 ). Scarlet blood , having passed through the capillaries of the organs (the diagram shows the capillary network of the stomach ( 3 ), becomes dark (shown in blue) and returns through the veins to the right atrium of the heart ( 4 ). The small circle is the path that blood passes through the lungs, therefore it is called pulmonary ... The small circle starts from the right ventricle of the heart ( 5 ) and passes only through the lungs ( 6 ). In the lungs, the blood gives off carbon dioxide and, saturated with oxygen, flows to the left atrium ( 7 ). More details about the movement of blood through the blood vessels systems can be viewed on the page “Human circulatory system“.
Top of page
Main Difference – Veins vs Arteries
Veins and arteries are two types of blood vessels in a closed circulatory system. The main function of blood vessels is to carry blood throughout the body. But arteries and veins differ in their structure and function. Veins are made up of a thin, elastic layer of muscle in their wall, while arteries are made up of a thick, elastic layer of muscle. A thick artery wall is important when dealing with high pressure blood released by the heart. Veins carry oxygen-depleted blood to the heart, while arteries carry oxygenated blood away from the heart. The main difference between veins and arteries is that veins are involved in removing cellular waste from the extracellular environment, whereas arteries are involved in providing nutrients and oxygen to the body's cells .
Key areas covered
1. What are veins - definition, features, functions 2. What are arteries - definition, features, functions 3. What are the similarities between veins and arteries - Brief description of the common features 4. What is the difference between veins and arteries - Comparison of the main differences
- The veins behind the knee hurt
Key words: aorta, arteries, arterioles, blood capillaries, blood pressure, closed circulatory system, veins, venules
Author: Oleg Yakupov
I belong to that category of Soviet people who are called “Tashkent Russians.” These are endemics who, surrounded by a foreign culture, have preserved a unique Russian, pre-revolutionary culture, and above all, the language. And also absorbed a lot of good things from the eastern culture that surrounded us in life. They also call us “Scoops”. But this applies not only to former residents of hospitable Tashkent, but to residents of the entire Soviet Union, who were formed as individuals during the Soviet Union. Fate has scattered many of us across the globe. We miss the usual communication. Our children and grandchildren, against their will, become “foreigners.” The blog is a place where I can speak out and, if I'm lucky, talk to people of my generation. Thanks to the Internet, it provides us with such an opportunity. View all posts by Oleg Yakupov