Causes of elevated bilirubin
The symptom appears when the following processes occur in the body:
- the breakdown of red blood cells in the blood accelerates;
- primary biliary cirrhosis is formed;
- cholelithiasis develops or other pathologies arise that prevent the outflow of bile from the body;
- a tumor forms in the liver;
- intrahepatic cholestasis develops;
- helminths appear in the body;
- an insufficient amount of enzymes is produced, on which the concentration of direct bilirubin in the blood depends.
A high content of bile pigment can also be associated with infectious inflammation, intoxication, autoimmune or chronic hepatitis.
An increase in direct bilirubin is one of the possible signs of gallbladder and liver cancer, as well as pancreatic cancer. The symptom occurs in cholelithiasis, biliary cirrhosis and other diseases. In addition, acute viral, bacterial, autoimmune, chronic, drug-induced and toxic hepatitis lead to an increase in direct bilirubin.
High levels of indirect bilirubin in the blood may be a sign of the following diseases:
- typhoid fever;
- Gilbert's syndrome;
- malaria;
- blood poisoning.
High bilirubin can also be caused by rare congenital and acquired diseases, during which there is increased destruction of red blood cells.
Why is the research being conducted?
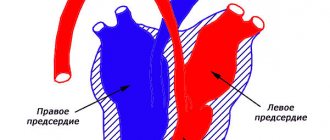
The liver is the largest organ in the human body, which performs many important functions:
- participates in the digestion process. The liver produces bile, which ensures the change from gastric to intestinal digestion,
- neutralizes the effects of allergens and toxic substances;
- regulates carbohydrate, lipid, protein metabolism;
- removes excess hormones and vitamins from the body;
- synthesizes immunoglobulins and antibodies;
- stores and distributes glucose and glycogen;
- replenishes the supply of certain vitamins.
However, the liver is capable of fully performing these functions only in the absence of pathologies. Liver tests - a biochemical blood test consisting of many laboratory tests - allow you to assess the condition of the organ.
The test is rarely carried out as a preventive measure. Most often, tests are prescribed if the doctor suspects that the patient has liver problems. For example, a referral for a study can be issued to those who have symptoms characteristic of liver pathologies - yellowness of the skin and sclera, pain in the right hypochondrium, sudden weight loss, nausea, vomiting, and the appearance of a sour-bitter taste in the mouth. In addition, the study is used to track the results of treatment of liver pathologies.
The indicators included in the liver tests reflect not only the functioning of the liver, but also other organs and systems - the heart, kidneys, intestines, thyroid gland, skeletal muscles. Therefore, the study may also reveal disorders not related to liver function.
Transcription of analyzes online.
cost of service: 500 rubles
Order
General practitioner Khanova Irina Ivanovna will interpret your tests during an online call in the Zoom or WhatsApp application.
- detailed explanation from the general practitioner.
- an alternative opinion from a competent specialist in interpreting the analyses.
- the opportunity to ask questions to the doctor regarding test results.
Symptoms of increased bilirubin in the blood
Excessive concentration of bilirubin in the blood occurs when there is a metabolic disorder in the body. A characteristic manifestation of the symptom is a yellow tint to the skin and mucous membranes. The sign occurs if the level of bilirubin in the serum increases. Based on the concentration of bile pigment, three degrees of symptoms are distinguished:
- 85 µmol/l – mild;
- 86-169 µmol/l – moderate;
- 170 µmol/l – severe.
With a high level of bilirubin in the blood, the following manifestations are possible:
- an unnatural skin tone appears - from bright yellow to greenish;
- the color of urine changes – it becomes orange or brown;
- skin itching occurs;
- there is a bitter taste in the mouth;
- stool becomes white;
- memory impairment;
- the liver increases in size, heaviness is felt in the right side;
- the whites of the eyes turn yellow;
- the patient feels weak.
Manifestations of increased bilirubin may differ depending on the type of jaundice:
- Suprahepatic. A sign of the disease is a yellow-orange color of the skin. Stool and urine darken. Possible skin itching.
- Hepatic. The color of the urine does not change, the stool becomes lighter. There is a slight but prolonged skin itching. Symptoms are mild, which is why the patient may not notice the presence of pathology for a long time.
- Subhepatic. Severe itching appears, the skin acquires a yellow tint. The disease occurs due to high levels of bile acids in the blood. The pathology worsens during hydronephrosis - stagnation of urine when the natural outflow of fluid from the kidneys is disrupted.
On the second or third day after the onset of subhepatic jaundice, the urine darkens and the stool becomes lighter; its shade is difficult to determine.
Treatment
Therapy for hyperbilirubinemia depends on the causes that caused it, i.e., treatment is etiotropic, aimed at the underlying disease.
Disruption of the biliary tract. Stones and obstructing tumors are removed. In some situations, stenting of the bile ducts is carried out - a frame is installed that preserves the lumen.
Hemolysis of red blood cells. Phototherapy and infusion therapy are prescribed to prevent or correct pathological losses. The infusion solutions contain glucose and albumin. These treatments help convert toxic bilirubin into a form that can be excreted from the body.
Kernicterus (bilirubin encephalopathy) in newborns
Pathology occurs in the first week of life. At first it is expressed by the following symptoms: suppression of the sucking reflex, vomiting, lethargy, monotonous cry. If not the signs are mild, if there is a risk of being discharged from the maternity ward without medical assistance. Typically, the disease manifests itself on the 4th day of life and requires an urgent exchange blood transfusion. This prevents the development of irreversible consequences.
After several weeks of development of the pathological condition, symptoms such as stiff neck, “stiff” limbs, convulsive posture with arching of the back, bulging of the large fontanel, hand tremors, convulsions, and a sharp cerebral cry appear.
Since the disease picture develops slowly over several days to weeks, during this time irreversible consequences in the central nervous system often occur. The disease finally manifests itself by 3–5 months of life, leading to paralysis, cerebral palsy, deafness, and mental retardation. To prevent the development of pathology, it is necessary to monitor bilirubin levels. If necessary, reduce the number of breastfeeding procedures. Perform phototherapy or exchange transfusion.
Diagnostics and tests
To determine what is causing the increase in bilirubin, you need to undergo examination by a specialist. After a visual examination (checking the color of the skin, whites of the eyes, plaque on the tongue) and palpation of the abdominal cavity, the doctor prescribes laboratory diagnostics:
- BAC for the content of direct or indirect bilirubin;
- Aspartate aminotransferase and alanine aminotransferase assay;
- Ultrasound examination of the liver.
Blood sampling may be prescribed for a detailed clinical analysis.
Correct therapy can be prescribed only with an accurate diagnosis. In some cases, the help of an infectious disease specialist and gastroenterologist is required.
Why does obstructive jaundice develop?
Malformations of the hepatobiliary system:
- Atresia and hypoplasia of the biliary tract.
- Bile duct cysts.
- Diverticula of the duodenum.
Non-inflammatory and inflammatory diseases of the gallbladder:
- Cholangiolithiasis is gallstones that obstruct the lumen of the bile duct.
- Strictures and stenosis of the bile ducts.
- Cholangitis.
- Cholecystitis.
- Pancreatitis.
- Cysts of the head of the pancreas.
Tumors:
- Cancer of the bile or hepatic ducts.
- Liver cancer.
- Pancreas cancer.
- Metastatic liver damage.
- Benign tumors - papillomatosis of the bile ducts.
Parasitic infestations:
- Echinococcus.
- Alveococcus.
Treatment of elevated bilirubin
To normalize the level of bilirubin in the blood, it is necessary to eliminate the underlying disease. Your doctor may prescribe the following treatments:
- infusion therapy, during which saline solutions and glucose are introduced into the patient’s body;
- taking medications, including phenobarbital, if we are talking about the treatment of Gilbert's syndrome, and hepaprotectors - in the case when the cause of the inflammatory process is liver damage;
- phototherapy, which involves irradiating the body with special lamps;
- change in diet.
When it comes to treating hepatitis, it is aimed at eliminating the causative virus.
If total bilirubin is increased in men
Exceeding the norm in men may indicate the development of such pathologies:
- Prehepatic (hemolytic) jaundice is often observed in newborn boys if their blood is incompatible with the mother’s blood according to the Rh factor or group. It may also be associated with congenital or acquired anemia.
- Hepatic jaundice (parenchymal) - liver damage against the background of viral hepatitis of various natures, toxic and autoimmune lesions.
- Subhepatic jaundice is associated with impaired movement of bile, pancreatic tumors, metastases and other causes.
USE OF REAMBERIN in patients with obstructive jaundice
Obstructive jaundice, which is one of the most serious illnesses, can be caused by complete or incomplete blockage of the bile ducts. With incomplete obstruction of the bile ducts, the development of obstructive jaundice is facilitated by dysfunction of hepatocytes (Shalimov A. A. et al., 1993). Thus, obstructive jaundice develops due to mechanical obstruction and, as a consequence, damage to hepatocytes in
| Figure 1. The drug reamberin is prescribed for the treatment of obstructive jaundice |
as a result of hypoxia, hepatitis and cholestasis.
Surgical trauma and anesthesia contribute to additional impairment of liver function. In some patients, after eliminating cholestasis, not only is the reverse development of jaundice not achieved, but also a tendency to its progression is revealed. The reason is a complex symptom complex of endogenous intoxication, caused by the influence of decompression on the functional state of the liver and various parts of homeostasis. Insufficiency of hepatic blood flow, caused primarily by biliary hypertension, as well as concomitant diseases of the cardiovascular system, together with microcirculation disorders and a decrease in the oxygen capacity of the blood, lead to hypoxia of hepatocytes. Renal disorders develop as a result of endotoxemia, which is associated with the presence of jaundice and microbial toxemia and indirectly causes disruption of microcirculation in the kidneys. In obstructive jaundice, disturbances in the lipid peroxidation system in mitochondrial membranes lead to impaired membrane permeability and cell death; in addition, there is a violation of oxidative phosphorylation, a decrease in the synthesis of ATP and creatine phosphate (Brass CA et al., 1995). This explains the need for an integrated approach in the treatment of this category of patients, taking into account the state of reactivity of the patient’s body and toxic reactions caused by jaundice and cholangitis. Currently, in biology and medicine, it is proposed to use succinic acid and its various salts as a biologically active substance with a wide range of pharmacological properties (Kondrasheva M.N., 1996).
The medical literature contains numerous data on the hepatoprotective and antioxidant properties of succinic acid salts - succinates (Malyuk V.I. et al., 1979; Kosenko E.A. et al., 1994). The cytoprotective and antioxidant effects of succinic acid have been known for a long time (Kondrashova M.N., 1996).
In the Clinic of Surgical Diseases No. 1 of the St. Petersburg State Medical Academy named after. I. I. Mechnikov studied the clinical effectiveness of the drug “reamberin 1.5% for infusion” as a detoxification, antioxidant and hepato-nephroprotective agent in the complex treatment of patients with obstructive jaundice of non-tumor origin in the early postoperative period.
The drug "reamberin 1.5% for infusion" is a balanced isotonic solution containing 1-(1-deoxy-d-glucitol-1-yl)-N-methylammonium, sodium succinate (1.5%), potassium chloride (0.015%), magnesium chloride (0.006%). “Reamberin 1.5% for infusion” has undergone a full course of preclinical studies in accordance with the requirements of the pharmacological committee of the Ministry of Health of the Russian Federation, which showed the complete absence of toxic, mutagenic and other side effects on the body.
| Scheme of administration of the drug "Reamberin 1.5% for infusion" |
| The drug “Reamberin 1.5% for infusion” was administered intravenously in the amount of 400 ml of infusion solution per day, according to the instructions for the clinical study, for 7 days after surgery, starting from the first day of the postoperative period. The administration of the traditional detoxifying drug Hemodez in the control group of patients was carried out in strictly similar volumes and timing of administration to the drug “Reamberin 1.5% for infusion.” |
It has been established that the drug has an antihypoxic effect, having a positive effect on biochemical processes in the cell, reducing the production of free radicals and restoring the energy potential of cells.
It activates the enzymatic processes of the Krebs cycle and Roberts shunt, promotes the utilization of fatty acids and glucose by cells, normalizes the acid-base balance and gas composition of the blood. The drug "Reamberin 1.5% for infusion" stabilizes the main hemorheological parameters of the blood, stimulates metabolic reactions in the liver and the removal of toxins from the body. Clinical studies were conducted using a multicenter trial method according to a single program for endogenous intoxication associated with obstructive jaundice. The study is open, controlled, randomized.
For the test, groups of 30 people were formed (control and main). The patients included 30 men and 30 women (15 in each group). The average age of the patients was 60±1.7 years (P<0.05). All patients with comparable pathology of the biliary tract (Table 1).
Table 1. Causes of bile duct obstruction
| № | Cause of obstruction | Number of patients control. groups | % | Number of patients in the main group | % |
| 1 | Choledocholithiasis | 15 | 50 | 15 | 50 |
| 2 | Cicatricial strictures of hepaticocholedochus | 15 | 50 | 15 | 50 |
| Total patients | 30 | 100 | 30 | 100 |
The patients underwent various surgical interventions, comparable in severity, volume and duration (Table 2).
All patients during the observation period were in a condition of severe or moderate severity. Clinical assessment was based on the identification of complaints, data from clinical examination, palpation, percussion, auscultation, data from clinical blood and urine tests, biochemical and immunological studies. To assess endogenous intoxication, a pool of substances of low and medium molecular weight (LMSMM) and oligopeptides (OP) was determined and the spectral characteristics of blood plasma were recorded in the wavelength zone from 238 to 310 nm according to the method of M. Ya. Malakhova (Malakhova M. Ya., 1995). The intoxication index was calculated using the following formula: plasma II = plasma VNISM x plasma OP.
Table 2. Scope of surgical interventions on the bile ducts
| № | Scope of surgical interventions | Number of patients control. groups | % | Number of patients in the main group | % |
| 1 | Choledocholithotomy. Drainage of the common bile duct with a T-shaped drainage | 15 | 50 | 15 | 50 |
| 2 | Choledochoenterostomy | 15 | 50 | 15 | 50 |
| Total patients | 30 | 100 | 30 | 100 |
For the treatment of all patients in both groups, generally accepted antibacterial drugs were used; the volume of intravenous infusions ranged from 1.5 to 3 liters and included various saline and energy solutions. In the control group, hemodez was used as the main detoxifying solution, in the main group, “Reamberin 1.5% for infusion.”
When taking into account clinical indicators such as pain, jaundice of the skin, darkening of urine, etc., we were faced with the problem of subjectivity in their assessment. At the same time, it is necessary to note some improvement in well-being, sleep, faster relief of skin itching and pain in patients in the main group.
As a result of the laboratory study, we included only indicators whose dynamics of changes in the comparison of the control and main groups were significant (p <0.05). In biochemical parameters (Table 3) when using the drug “Reamberin 1.5% for infusion”, clear positive dynamics were revealed, comparable to one of the main detoxifying drugs used in surgery—hemodesis. Positive dynamics of intracellular liver enzymes (AST, ALT and the most indicative of obstructive jaundice - alkaline phosphatase), more pronounced in the main group, indicates an improvement in liver function, a decrease in damage to hepatocyte membranes associated with the hepatoprotective and antihypoxic properties of the drug "Reamberin 1.5%" -ny for infusions." The positive dynamics of bilirubin in the postoperative period in patients with obstructive jaundice can be explained in terms of both the cytoprotective properties of the drug and its detoxification effect (increased diuresis, direct binding of bilirubin and its excretion in the urine).
Table 3. Biochemical parameters
| № | Index | Norm | Main group | Control group | ||
| Use of the drug | Before | 8th day | Before | 8th day | ||
| 1 | Alkaline phosphatase | up to 120 units/l | 197±15 | 105±9 | 189±12 | 115±11 |
| 2 | Total bilirubin | 3.4-17.1 µmol/l | 247±17 | 19±3 | 231±13 | 21±2 |
| 3 | Creatinine | 44.2-106 µmmol/l | 149±12 | 92±5 | 127±15 | 94±5 |
| 4 | AST | 0.06-0.46 mmol/l | 0,76±0,11 | 0,42±0,09 | 0,71±0,13 | 0,49±0,09 |
| 5 | ALT | 0.12-068 mmol/l | 0,98±0,12 | 0,63±0,11 | 0,92±0,09 | 0,72±0,08 |
In patients with acute renal failure, the use of the drug "Reamberin 1.5% for infusion" also had a positive effect (Table 3), which is confirmed by studies of creatinine, as well as a more rapid transition of acute renal failure from the stage of oliguria to polyuria with an increase in daily diuresis, that is, a faster resolution of acute renal failure (on average two to three days). The use of reamberin in patients with anuria turned out to be especially effective.
| The drug “reamberin 1.5% for infusion” gives a good clinical effect as a detoxification therapy for patients with severe forms of endogenous intoxication with obstructive jaundice; it improves the functional state of the liver (positive dynamics of liver enzymes), has antioxidant and antihypoxic properties, does not cause allergic and vascular reactions |
On the part of peripheral blood, positive dynamics are clearly visible in the example of leukocytosis, comparable to the same dynamics in the control group, which indicates a more rapid resolution of one of the components of obstructive jaundice - cholangitis when using reambirin.
Table 4. Peripheral blood parameters
| № | Index | Norm | Main group | Control group | ||
| Use of the drug | Before | 8th day | Before | 8th day | ||
| 1 | Leukocytes x | 4-9 | 16,7±3,2 | 10,2±2,9 | 16,1±4,1 | 10,9±3,7 |
| 2 | Band neutrophils x 109 | up to 4 | 5±2 | 3±1 | 4±1 | 3±2 |
Level of endogenous intoxication (Table 5). In the main group there was a lower level of VNiSMM in the blood plasma after surgery, with a tendency to normalization in the first week after surgery.
Secondary immunodeficiency associated with endotoxicosis due to obstructive jaundice was assessed using level 1 and 2 tests characterizing immunological parameters of peripheral blood. In the main group, after using the drug “Reamberin 1.5% for infusion”, moderate disturbances in terms of nonspecific resistance were revealed: a lower value of the phagocytic number (compared to the control group), a moderate increase in the phagocytic index and NBT test and spontaneous migration to RTML with FHA.
Table 5. Indicators of endogenous intoxication
| № | Groups | Main group | Control group | ||
| Use of the drug | Before | 8th day | Before | 8th day | |
| 1 | VniSMM u. e. | 41,4±4,2 | 27,9±1,9 | 39,3±8,3 | 31,9±1,2 |
| 2 | Oligopeptides mg/l | 1820±120 | 940±20 | 1950±20 | 1080±110 |
| 3 | Plasma toxicity index | 71,2±0,3 | 25,7±0,2 | 61,5±0,4 | 28,9±0,7 |
| 4 | Catabolic pool e. | 17,8±3,0 | 11,6±1,6 | 12,8±1,7 | 16,7±2,9 |
In the main group in the cellular link, we noted a positive dynamics in the absolute number of lymphocytes with preservation of almost normal percentages in their subgroups, an increase in the absolute number of T-active lymphocytes, a decrease in T-lymphocytes (E-ROC), normal values of theophylline-resistant lymphocytes and a decrease in the number of theophylline-sensitive lymphocytes , increasing the migration index in RTML with FGA.
In the humoral link, positive dynamics were also revealed in the main group: a decrease in the absolute number of B-lymphocytes while maintaining their functional activity; a lower level of circulating immune complexes (which indicates improved elimination from the blood) and normal levels of immunoglobulins A, M and G. Analysis of the results convincingly shows that the state of the immune system and nonspecific resistance of the body depends on the severity of endogenous intoxication in obstructive jaundice and successfully corrected by using Reamberin.
Table 6. Indicators of the antioxidant system
| № | Index | Main group | Control group | ||
| Use of the drug | Before | 8th day | Before | 8th day | |
| Are common | |||||
| 1 | SH | 10,8±2,3 | 8,5±3,2 | 10,5±3,1 | 9,0±2,7 |
| 2 | SS | 3,0±1,2 | 2,3±0,8 | 3,3±1,2 | 4,0±1,1 |
| 3 | SH/SS | 3,4±0,7 | 3,0±0,4 | 3,2±0,7 | 2,2±0,5 |
| Non-protein | |||||
| 1 | SH | 1,3±0,3 | 1,5±0,5 | 1,4±0,4 | 1,4±0,4 |
| 2 | SS | 0,8±0,2 | 0,6±0,2 | 0,7±0,2 | 1,1±0,3 |
| 3 | SH/SS | 1,5±0,4 | 1,9±0,3 | 1,9±0,5 | 1,3±0,3 |
| Protein | |||||
| 1 | SH | 9,2±0,4 | 7,1±0,9 | 9,4±0,3 | 6,6±0,7 |
| 2 | SS | 3,3±0,3 | 3,1±0,5 | 2,9±0,4 | 3,2±0,5 |
| 3 | SH/SS | 2,9±0,5 | 2,1±0,3 | 3,2±0,7 | 2,3±0,4 |
With obstructive jaundice, the formation of oxygen radicals in cells and tissues increases sharply. Due to the high aggressiveness of free radicals, substrates with a wide variety of chemical structure, properties, and biological activity can be subject to oxidation. As a result, the properties of these substances change dramatically, which makes free radicals potentially dangerous and requires the use of specific antioxidant drugs in the treatment of obstructive jaundice. The most indicative from the point of view of assessing the antioxidant effect are thiol-disulfite ratios (Table 6). The higher the total buffer capacity of the antioxidant system, the more the redox equilibrium in the thiol-disulfide system (SH/SS) is shifted to the left (towards reducing equivalents). Analysis of the data on thiol disulfide ratios given for both general and protein and non-protein indicators of the antioxidant system of patients with obstructive jaundice convincingly proves the normalization of the buffer properties of this system when using the drug "Reamberin 1.5% for infusion" in the postoperative period compared with control group.
How is a biochemical blood test performed?
A biochemical blood test is a common type of diagnosis that doctors prescribe to assess the condition of the patient’s body. This is a quick and informative method that allows you to identify signs of asymptomatic diseases.
To obtain accurate data, the patient is recommended to prepare before going to the laboratory. Failure to follow the rules may result in incorrect diagnosis.
Basic requirements for the preparatory process:
- biochemistry is carried out in the morning (8-00 - 11-00);
- you need to come to the laboratory on an empty stomach (the period of fasting should be at least 8 and no more than 12 hours);
- the day before the test, you should not eat heavy food, you are allowed to drink only purified water;
- if the patient is taking medication, first check with the doctor whether a break is required;
- 1 hour before going to the clinic you should stop smoking;
- one day before the procedure, you should avoid outbursts of emotions and physical activity;
- It is recommended to sit directly in front of the door to rest for about 15 minutes.
The process of drawing blood involves applying a tourniquet and placing it above the elbow. The puncture site is treated with cotton wool soaked in an antiseptic. This is necessary to prevent infection. After inserting the needle, the nurse checks that the vein is full of blood. Next, the biomaterial is collected. When taking tests, the patient's body must remain motionless.
If it is not possible to take blood from the ulnar vein, the collection is carried out from other veins available for the procedure. The biomaterial is poured from the syringe into a test tube and sent to the laboratory along with the referral.
Diagnosis of jaundice
- Laboratory examination. Determination of the level of bilirubin in the blood. Direct and indirect bilirubin are determined. Obstructive jaundice is characterized by bilirubinemia due to an increase in direct bilirubin. Levels of cholesterol, lipids and alkaline phosphatase also increase, indicating the development of cholestasis.
- Ultrasound of the liver and bile ducts. This study will detect the expansion of the lumen of the bile ducts, thickening of their walls, and in some cases determine the cause of obstruction (tumor). If anechoic stones are present, ultrasound may not show them.
- CT scan of the abdomen with contrast enhancement. It is carried out to determine the cause of the obstruction, which was not identified at the previous stage.
- Retrograde cholangiopancreatography. This procedure combines endoscopic and x-ray technologies. Using an endoscope, a radiopaque substance is injected into the papilla of Vater and a series of photographs are taken. The study allows you to visualize the ducts and detect places of their obstruction (overlap).
- Percutaneous transhepatic cholangiography. A puncture of the intrahepatic bile duct is performed through the abdominal wall under ultrasound guidance. After this, the duct is filled with a radiopaque substance and photographs are taken.
Complications of jaundice
High hyperbilirubinemia and jaundice are life-threatening conditions and can lead to death, even after eliminating the causes that caused it.
When hepatocytes are destroyed, a large amount of toxic substances are released into the blood, which have a systemic effect. Functional disorders increase, and renal-hepatic syndrome develops. Bilirubin penetrates the blood-brain barrier and causes disruption of the brain (hepatic encephalopathy), which is accompanied by stunned consciousness, even coma.
A toxic effect of bilirubin on surfactant, an important component of the lungs, has also been noted. When it is damaged, respiratory failure develops. Impaired production of blood coagulation factors leads to the development of DIC syndrome.
Clinical manifestations
Jaundice
A characteristic and striking clinical sign is yellowing of the skin, mucous membranes and sclera (whites of the eyes). In fact, all biological fluids of the body turn yellow, except saliva and tears. Yellowness of the skin is associated with the impregnation of tissues with bilirubin due to its high content in the blood.
Cholestasis
Cholestasis is the cessation of bile secretion into the intestines. It remains in the ducts, accumulates there and is eventually absorbed back into the blood. All together this leads to the following manifestations:
- In the blood, in addition to an increase in bilirubin content, there is also an increase in the content of cholesterol, lipids, and cholates. In addition, the activity of some enzymes increases, for example, alkaline phosphatase, GGTP, etc.
- Cholemia. Bile acids entering the bloodstream have a toxic effect, which is accompanied by a decrease in heart rate, a decrease in blood pressure, patients are drowsy and irritable, they may show signs of depression. Due to the toxic effect on nerve endings, itching develops, which is difficult to stop. The entry of bile acids into the urine leads to a change in the properties of surface tension, which causes it to foam during urination. Together with the dark brown coloration, this sign is called “beer urine.”
Acholia
Acholia is a symptom complex that develops when bile does not enter the intestines. This leads to indigestion. First of all, fat digestion suffers. They are not absorbed and are excreted along with feces. This condition is called steatorrhea. The metabolism of proteins and vitamins, especially fat-soluble ones, including vitamin K, which is necessary for the synthesis of blood clotting factors, is also disrupted. This, in turn, leads to bleeding. Also, normally, bile has a bactericidal effect. Accordingly, in its absence, the ratio of intestinal flora begins to be disrupted towards the predominance of anaerobes.
Bile has a stimulating effect on intestinal motility. Accordingly, in its absence, constipation occurs, which is replaced by foul-smelling diarrhea due to the dilution of intestinal contents by putrefactive microflora. The absence of bile pigments in stool leads to its discoloration - acholic stool.
Discholia
Stagnation of bile in the ducts leads to the fact that it changes its physical and chemical properties, which ultimately contributes to the formation of stones.
Prehepatic (hemolytic) jaundice
Prehepatic (hemolytic) jaundice occurs as a result of increased hemolysis of red blood cells caused by intra- or extra-erythrocyte factors: hemolytic anemia, defects of erythrocyte enzymes, hemolytic disease.
The skin is usually lemon-yellow (patients are more pale than jaundiced). In addition to manifestations caused by hemolysis of red blood cells (anemia, reticulocytosis, hemoglobinuria), there is an increase in the content of indirect bilirubin in the blood.
Hereditary conjugated hyperbilirubinemia
Hereditary conjugated hyperbilirubinemia is manifested by moderately severe jaundice, inherited in an autosomal recessive manner. It disrupts the transport of bilirubin and other organic anions from the liver to bile. The disease manifests itself from 2 years of age.
In hepatocellular disease (hepatitis, cirrhosis), three main stages of bilirubin metabolism are disrupted
In hepatocellular disease ( hepatitis, cirrhosis ), three main stages of bilirubin metabolism are disrupted - its absorption by the liver, binding and excretion. Moreover, excretion is the stage that limits the rate of bilirubin metabolism, and it is usually the stage that is disrupted to a greater extent. As a result, in these diseases hyperbilirubinemia predominates, mainly caused by direct bilirubin. Vaccination of children against hepatitis B at the Markushka children's clinic.