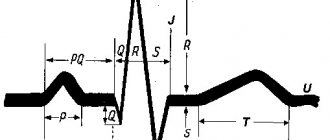
If a local area of the heart muscle fails to work (necrosis, hibernation, sclerosis, stunning), this is manifested on the ECG by the appearance of a pathological Q wave.
A Q wave is considered pathological if its duration exceeds 0.03 s and its amplitude is greater than 1/4 of the R wave. An exception is lead aVR.
Changes in “pathological waves” must be present in two adjacent leads (for example V1+V2, V5+V6, AVL+I, etc.)
If a pathological Q is suspected in lead III, then it should be duplicated in lead aVF and not disappear with a deep breath!
Scar changes cannot be judged in the presence of left bundle branch block
In fact, these are the main criteria and now we will analyze them in more detail.
General information
Electrocardiography is the simplest diagnostic method for studying the functioning of the heart.
The essence of the examination is to record electrical impulses that accompany the contractile and restorative functions of the myocardium, called “depolarization” and “repolarization.” What do myocardial changes on an ECG mean?
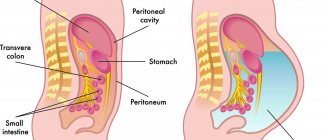
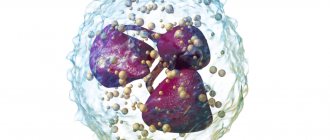
Specific abnormalities in the electrocardiogram can be recorded during a routine medical examination and characterize the condition of the myocardium at the time of the examination. The function of the myocardium is to synthesize by cardiomyocytes , due to which the cavity contracts and ensures normal blood supply to the entire body. This process is carried out due to the cellular exchange of sodium and potassium ions in the cell. The functioning of the cardiac conduction system is recorded on an electrocardiogram using electrodes fixed on the limbs and chest.
Pathogenesis
Changes in the ECG are not a disease, but only a manifestation of some pathological processes occurring in the myocardium. With shifts in the biochemical activity in the heart cells, their contractility changes, which is reflected in the cardiogram when recording the conduction of impulses. Cardiomyocyte function can be impaired during inflammatory processes, for example, with myocarditis . Taking certain medications also affects the functioning of the heart muscle.
Long-term diabetes mellitus can gradually lead to atherosclerosis . Not only large vessels are affected, but also the coronary arteries that supply the myocardium. With inflammatory pathology in the gastrointestinal tract, the absorption of nutrients is impaired, which also negatively affects metabolic processes in cardiomyocytes.
Signs of a problem
Cardiac activity depends on many criteria that affect intracellular metabolism in the tissues of the heart muscle. The constancy of the internal environment can be periodically disrupted, which can lead to disruptions in the functioning of the heart cells. Diffuse changes in the myocardium are not considered a disease; it is a syndrome that means an accumulation of changed cells with impaired conduction of electrical impulses in a given area, clearly displayed on the ECG. It is important to determine the cause of such failures; it may be hormonal in nature, infectious in origin, or a consequence of heart disease of varying severity.
Changes are not always only diffuse, covering sectors in each department of the organ. They can be focal as a result of the formation of scars in the myocardium of any size. The scar is a connective tissue that does not conduct impulses; the electrical inertia of this area is visible on the cardiogram.
The variety of myocardial diseases is very large, but the general signs of problems with the cardiovascular system and symptoms of myocardial changes are as follows:
- burning and pressing pain behind the sternum;
- shortness of breath at the slightest physical exertion or even at rest;
- disturbances of heart rhythm and contraction frequency;
- increased fatigue, general weakness, chronic fatigue.
The primary change in the heart muscle provokes the development of certain processes:
- myocardial hypoxia;
- circulatory disorders;
- disruptions in the transport of oxygen to cells and tissues;
- irreversible necrotic consequences.
A critical case of the development of myocarditis is an acute infarction; its course also varies.
Classification
Depending on the size and location of the changed cardiomyocytes, the following are distinguished:
- Diffuse changes. Such a widespread lesion indicates the presence of multiple foci of altered cardiomyocytes. Characteristic signs are present in all leads on the ECG.
- Focal changes. Lesions are recorded only in certain leads that correspond to specific areas of the myocardium. Focal changes are a kind of clearly limited areas of connective, scar tissue, which are inert to conduct electricity.
When diagnosing changes on the ECG, a functional diagnostics doctor and cardiologist can state:
- early ventricular repolarization, which is manifested by a negative “T” wave;
- a decrease in the voltage of the r wave, which characterizes the contractility of the myocardium;
- rhythm disturbances;
- conduction disturbances.
Depending on these indicators, the causes of changes in the ECG are determined by nature:
- inflammatory;
- cicatricial;
- dystrophic;
- metabolic.
EXAMPLE 1
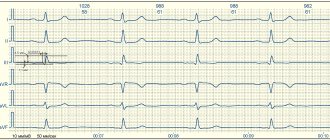
When assessing the ventricular complexes, we notice a more or less pronounced QIII wave. We measure its width and height. As you can see, its width approaches 0.03 s., but does not exceed the norm, we also see that its amplitude (height) is about 1-1.1 mm, which is less than 1/4 of the R wave, which is equal to 4. 5 mm. We also see that in lead aVF the Q wave also falls within the normal range.
Thus, we conclude that these are not scar changes.
Causes
Dystrophic changes in the myocardium
Such changes in the ECG are formed due to insufficient nutrition of cardiomyocytes, which inevitably leads to a decrease in the contractility of the left ventricle. Diffuse-dystrophic changes in the myocardium are observed with:
- pathologies of the endocrine system: diabetes mellitus , adrenal dysfunction, disorders of the thyroid gland;
- pathologies of the renal system and liver: excessive amounts of toxic metabolic products negatively affect the functioning of the heart;
- chronic diseases of infectious origin: changes can be observed with tuberculosis , influenza , malaria , etc.;
- chronic iron deficiency anemia : constant oxygen starvation affects the functioning of cardiomyocytes;
- with an unbalanced diet, with vitamin deficiency in the diet;
- with excessive nervous and physical overload;
- with fever and concomitant dehydration;
- in case of poisoning with alcohol, medications or chemical components.
Metabolic changes in the myocardium
What it is? Characteristic nonspecific changes on the ECG are formed as a result of disturbances in intracellular metabolic processes associated with potassium and sodium ions.
Metabolic changes are associated with dystrophy of the heart muscle and appear when:
- ischemia , which is reflected on the cardiogram in the form of deviations of the T wave. Its polarity and shape changes in the leads corresponding to the damaged areas;
- myocardial infarction : the location of the ST segment changes on the ECG, which is located either above or below the isoline;
- death, necrosis of the myocardium, which is characterized by the appearance of an abnormal Q wave.
Scar changes
Areas of scar tissue form at the site of a former inflammatory process, necrosis, as a result of which normal, healthy cardiomyocytes lost their contractility and were replaced by connective tissue that does not have elasticity. Focal cicatricial changes on the ECG indicate a previous myocardial infarction .
- The lower wall of the left ventricle is characterized by changes in leads: II, III and a VF (indicates damage to the right, less often the left circumflex coronary artery).
- The anterior septal region is characterized by changes in leads: V1 and V2 (the left descending septal branch is damaged), or V2-V4 (the left descending coronary artery or its branches is involved).
- The anterior-lateral region is characterized by changes in leads: I, aVL, V4-V6 (the circumflex artery or the left descending artery is damaged).
- Anterior widespread infarction is characterized by changes in leads: I, aVL, V1-V6 (the left descending coronary branch is damaged).
Moderate inflammatory changes in the myocardium
Characteristic changes are observed in myocarditis, in which the voltage of the waves in all leads decreases and rhythm disturbances are recorded. Moderate left ventricular changes may occur after:
- typhus , diphtheria ;
- rheumatism , after streptococcal infection ( tonsillitis , tonsillitis , scarlet fever );
- infections caused by the Coxsackie virus, rubella , influenza , measles ;
- exacerbation of an autoimmune disease ( systemic lupus erythematosus , scleroderma ).
Brown myocardial atrophy
This is what a macropreparation is called during histological examination. Characteristic pathological changes in the myocardium are formed as a result of a long-term lack of blood supply, which is observed in debilitating diseases, cachexia , drug abuse, increased physical activity, and also in old age. lipofuscin, is deposited . Its granules are a product of impaired metabolism in cardiac muscle cells, weakened by insufficient nutrition and blood supply.
EXAMPLE 2
Here is another Q in the same lead III. But here, after measurements, we see that its amplitude is not just 1/3 or 1/2 R, but almost equal to it - this is not the norm. In addition, the duration (width) of 0.04 s also goes beyond what is permitted. In the adjacent lead aVF, the Q wave is also pathological - it has a height of 1/3 R and a width of about 0.04 s. This gives us every right to talk about scar changes in the posterior wall (this is the area controlled by these leads)
Symptoms
Moderate and minor changes in the ECG may not manifest themselves clinically and may be found on the cardiogram during routine medical examinations and medical examinations. With pronounced changes, special symptoms appear:
- chest pain of a pressing, burning nature, indicating an attack of angina pectoris ;
- swelling of the lower extremities, shortness of breath with minimal physical activity indicate the progression of heart failure ;
- a feeling of interruptions in the work of the heart, arrhythmias ;
- fatigue, pale skin;
- sticky sweat;
- tremors , weight loss in a short time.
Tests and diagnostics
To identify the true cause of changes in the myocardium, it is recommended to undergo a full examination, which includes:
- General analysis and biochemical blood test. Based on the results, it will be possible to talk about the presence of an inflammatory process in the body, the functioning of the renal system and kidneys, and the level of cholesterol , which forms plaques in the coronary arteries.
- ECG. Characteristic changes during the examination make it possible to determine further examination tactics. In some cases, it is recommended to perform an ECG with stress, or organize daily ECG monitoring.
- EchoCG. Ultrasound examination of the heart allows you to assess the condition of the valve apparatus of the heart, identify areas of damage, and evaluate the pumping function of the heart.
- Myocardial scintigraphy. The radioisotope research method shows areas of accumulation of a special substance to identify areas of damage and determine their nature.
Changes in the myocardium on the ECG make it possible to determine further tactics for examining the patient to establish an accurate diagnosis and select the correct therapy.
Diagnosing and fixing the problem
Minor changes in the myocardium will not require drastic measures. The patient will be advised to adjust blood pressure, take a course of vitamins and adhere to a healthy lifestyle.
More serious changes in the myocardium already imply the presence of a disease; for diagnosis, the following measures are usually performed:
- Clinical blood test. Examines hemoglobin levels and inflammation criteria.
- Biochemistry of blood. Determines the condition of the liver, kidneys, the amount of glucose, protein, cholesterol.
- General urine analysis. Evaluates renal activity.
- Ultrasound. Visual examination of internal organs.
- ECG. Diffuse changes are indicated by a decrease in T waves, responsible for ventricular repolarization. Focal changes are indicated by negative T waves in 1–2 sectors.
- Echocardiogram. The most informative method that identifies the causes of changes in the heart muscle thanks to clear visualization of its parts.
Therapy must be combined with correction of diet and lifestyle. Changes in the myocardium of a dystrophic or metabolic nature by default require proper rest, adherence to sleep patterns and diet.
The heart responds well to those present in the diet:
- nuts;
- spinach;
- carrots and potatoes;
- apricots, peaches, bananas;
- lean poultry and meat;
- red fish and caviar;
- cereals, grains;
- dairy products.
Chocolate and confectionery products should be consumed to a minimum. Fatty meat and poultry are extremely rare. Soda, coffee and alcohol are excluded. You should also remove spicy, fatty, salty, spicy and fried foods.
The following drugs help improve metabolic processes in heart muscle cells:
- “Asparkam”, “Panangin”, “Magne B6”, “Magnerot” - potassium and magnesium stabilize the frequency of contractions.
- “Mexidol”, “Actovegin” are antioxidants that eliminate lipid oxidation products in myocardial cells.
- Vitamins A, B, C, E - without them, intracellular metabolism is impossible.
If the cause of myocardial changes is a disease, then appropriate therapy will correct the situation. The lack of hemoglobin is compensated for with iron-containing drugs; for myocardial inflammation, antibiotics and Prednisolone are prescribed; for cardiosclerosis, urinary agents and cardiac glycosides are indicated.
Focal changes in the myocardium mean ischemic damage to the heart muscle, ischemia and necrosis.