The incidence of cardiovascular pathology is growing rapidly, becoming epidemic. Mortality rates from these problems are also increasing, which makes the issue of treatment and especially prevention the most important in modern society. Coronary heart disease, as one of the manifestations of vascular atherosclerosis, has several forms. One of them is called subendocardial ischemia. What is the meaning of this intricate term and what to do if a doctor makes such a diagnosis?
Definition
Subendocardial ischemia is a disease associated with impaired blood supply to the heart muscle (myocardium). The term “subendocardial ischemia” is found in case reports and the cardiology literature. This condition is not permanent, i.e. for a short time. As a result, the ECG shows changes in the processes of ventricular repolarization. In this case, the myocardium acquires a negative charge without depolarization disturbances. Unlike the subepicardial type, with subendocardial ischemia the ischemic process itself occurs in a limited area of the heart muscle.
The concept of “myocardial ischemia” and its types
Ischemia means a discrepancy between the oxygen demand of organs or tissues and its supply, as a result of which hypoxia develops. Arterial vessels supply oxygen to the tissues along with blood. If their patency is impaired, blood flow and, accordingly, the amount of oxygen decreases. If an organ performs constant mechanical work, like the myocardium of the heart, it needs rapid elimination of ischemia, otherwise irreversible changes (necrosis) may occur in it.
Ischemia is aggravated by increased physical activity, as this increases the myocardial oxygen demand
The structure of the heart wall consists of three layers:
- epicardium (external);
- myocardium (medium);
- endocardium (internal).
Based on this, ischemia can be localized under the outer ball of the wall (subepicardial) of the myocardium, under the inner ball (subendocardial) or pass through the entire wall (transmural). Subendocardial zones have a much greater sensitivity to ischemia than others due to the fact that the coronary arteries approach the heart muscle from the epicardium. The smallest caliber arteries are located under the endocardium. Therefore, the subepicardial layers are supplied with blood more powerfully, but the ischemia of these zones is always more significant. In addition, the outer and inner layers of the myocardium are always subject to greater compression during heart contractions than the middle ones.
Reference! Ischemia is a temporary process, and if the action of the damaging factor stops, blood flow resumes, and if not, irreversible changes develop in the heart muscle.
Subendocardial ischemia is transient in nature and limited to a small area of the myocardium. It causes the appearance of a negative charge on cardiomyocytes. The process of formation and propagation of an electrical impulse in the heart occurs thanks to the conduction system of the heart. During the passage of this impulse through the myocardium, complex bioelectric processes occur in the cells:
- depolarization,
- repolarization.
Subendocardial ischemia affects repolarization processes without changes in depolarization. Subepicardial ischemia extends to both the endocardium and the epicardium, covering a larger area of the myocardium.
Causes
Under the influence of hypothermia, severe pain, and hormonal disorders, subendocardial ischemia can also be observed in healthy people. However, more often the cause of the disorder is coronary heart disease. It develops against the background of a lack of oxygen reaching the heart. Oxygen starvation occurs as a result of a malfunction of blood vessels. The most common cause of improper functioning of blood vessels is atherosclerosis. Cholesterol accumulates on the walls of blood vessels, as a result of which their walls become denser, and the lumen of the arteries narrows significantly or becomes completely clogged. Particularly dangerous is vascular occlusion in the area of branching arteries that supply oxygen to all vital organs.
What is important to remember
Treatment of ischemia should be carried out according to a standard regimen, regardless of in which part of the myocardium it occurred. Its goals are to eliminate causes, relieve symptoms, and prevent necrosis. In our practice, we use both medicinal and surgical methods of therapy.
We always focus on modifying the patient’s lifestyle: giving up bad habits, adjusting the diet, and aerobic exercise. It is the reduction of these risk factors that will help keep the artery walls elastic, strong, smooth and ensure adequate blood flow.
Symptoms
Subendocardial ischemia manifests itself in an acute form or remains undetected for a long time, proceeding asymptomatically. Painless myocardial ischemia occurs. It is difficult to identify signs of the disease on your own, because painful sensations appear not only in the area of the heart muscle, but also in the left forearm, arm, intercostal area or scapula. Aching pain and a numb chin are less typical symptoms of this disease. One of the main manifestations of subendocardial ischemia is angina pectoris. It is characterized by aching pain in the chest area after physical activity, after going out into the cold, or after eating a large meal. Emotional outbursts and stress are the causes of exacerbation of this disease. In a calm state, it may not bother the patient or introduce discomfort into his daily rhythm of life.
Subendocardial ischemia
This term refers to a condition that occurs due to insufficient blood supply to the inner layer of the myocardium.
Complaints that patients may make:
- unpleasant or painful sensations in the neck or jaw area;
- paresthesia, tingling in the shoulder or arm;
- fast heartbeat;
- shortness of breath, especially during physical activity, feeling of lack of air;
- nausea and vomiting;
- profuse sweating;
- fatigue, dizziness.
It is worth noting that some people with CAD do not have significant signs or symptoms. This condition is called silent ischemia. Its danger lies in increasing the risk of sudden cardiac events, such as:
- Heart attack. If a coronary artery becomes completely blocked, the lack of blood and oxygen will lead to a heart attack. The consequences can be fatal.
- Irregular heart rhythm (arrhythmia) , which can weaken the heart and cause life-threatening asystole.
- Heart failure. The ability of the heart to effectively pump blood to other organs and systems decreases due to a decrease in the force of contractions and ejection fraction.
ECG signs
Manifestations of this pathology on the electrocardiogram are:
- modification of the amplitude, polarity and shape of the T wave;
- ratio of the RS - T segment to the isoline.
Depending on which wall is affected - anterior, apical, posterior or lateral - the ECG results will differ.
The repolarization wave moves internally, therefore, the vector of rapid repolarization of the anterior wall is oriented towards the positively charged electrodes on the chest, in which we register the T wave directed upward from the isoline.
In case of illness, this process is delayed and the vector has a larger value compared to the norm. The T wave becomes tall and wide, called the coronary wave. .
An ECG sign of this type of ischemia is depression (lowering) of the ST segment. It is reversible if the episode is temporary, but persists if it is severe enough to cause a heart attack.
The key difference between subendocardial ischemia is a flattened and reduced T wave.
Diagnostics
The electrocardiography method helps to detect subendocardial ischemia. This study shows changes in the T wave. However, an ECG alone is not enough to make a diagnosis. Additionally, the patient is prescribed Holter monitoring, when a portable device is used to record the patient’s heartbeats throughout the day. If necessary, stress tests, coronary angiography, and CT scanning are performed during the examination. Based on these and other methods, the cardiologist will draw up a complete picture of the disease and prescribe treatment.
T wave changes in ischemic heart disease
With ischemic heart disease, the T wave can be changed in two situations.
- With ischemia associated with an attack of angina, a negative T wave may be recorded in two (or more than two) adjacent leads.
- In the acute phase of myocardial infarction with ST elevation, a high positive T may be recorded.
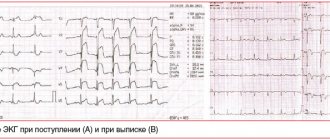
Look at ECG 5 with an example of ischemia and inverted T waves.
ECG 5. Negative T waves in myocardial ischemia
ECG source.
ECG 5 shows inverted T waves in the left leads: V5-V6, I, aVL.
Negative T values indicate ischemia if the following conditions are met.
- The depth of negative T must be at least 1 mm.
- Negative T waves must be recorded in at least two adjacent leads.
- The QRS complex before the negative T has a tall positive R wave.
- Dynamics of change. These should be “new” inverted Ts (they should not be on old cardiograms). Within some time (hours or days) there should be a return of the T wave to the isoline.
In addition, it should be remembered that inverted T wave in leads III, aVR, V1 is a normal variant.
ECG 6 shows another example of a change in the T wave in coronary artery disease: high coronary T wave in the acute phase of myocardial infarction with ST elevation. This is the initial and very short period of a heart attack, so it is not always possible to register it on an ECG.
ECG 6. High positive T wave in the acute phase of myocardial infarction
ECG source.
Treatment
Treatment and prevention of the development of this disease according to the standards of treatment of coronary artery disease is carried out using pharmaceuticals. The patient is prescribed medications that thin the blood, dilate blood vessels and reduce the level of bad cholesterol. Sometimes medications and pills do not help well - in such cases, myocardial revascularization is indicated, i.e. surgery. If indicated, the attending physician will recommend a vascular stenting procedure, which involves the quick and painless implantation of a stent into an artery.
Clinical case
A 74-year-old obese woman was admitted to our department with repeated episodes of chest pain over the past few days.
The photo below shows the ECG result recorded after the exercise. While recording the tape, the patient began to complain of chest discomfort. After the administration of Nitroglycerin, the patient felt better, and an ECG was re-recorded.
Coronary angiography performed on the patient showed severe stenosis of the right coronary artery.
Manifestations on the cardiogram
Subepicardial ischemia on the ECG will be visible as negative, symmetrical and peak T-waves in leads that correspond to the location of the affected area of the myocardium. T-waves can be dynamic, appearing only during pain, and also regress on their own or after the administration of Nitroglycerin.