Gymnastic exercises for coronary heart disease
Everyone knows such clinical forms of coronary heart disease (formerly known as “angina pectoris”), such as angina pectoris or myocardial infarction, resulting from spasm of the coronary vessels and disturbances in the blood supply to the heart.
Performing available gymnastic exercises in quiet intervals between attacks will help improve your condition, prevent the occurrence of critical situations and further aggravation of the disease. Depending on the tolerance of physical activity during angina pectoris (that is, the appearance of pain in the heart or pathological changes in the electrocardiogram), 4 functional types are distinguished.
The first functional type includes patients who tolerate physical activity well. They rarely have angina attacks, and heart pain occurs only when performing unusually heavy loads or under significant neuropsychic stress. They are capable of performing muscular work with a power of more than 100 W. Patients with coronary heart disease with the first functional class can walk for a long time at any pace. Many of them also do slow running.
The second functional type includes patients with rare attacks of angina pectoris (that is, appearing during muscular work), which occur, for example, when walking too fast or climbing 2-3 floors. Their exercise tolerance ranges from 50 to 100 watts. They tolerate walking well at a moderate pace. To increase their performance and improve their condition, they can train in walking at a leisurely pace twice a day for 30-40 minutes.
The third functional type includes people with coronary heart disease with frequent attacks of angina pectoris that occur during minor muscle strains, for example, climbing the 1st floor, walking at a moderate pace on level ground, etc. Their tolerance to physical activity is less than 50 W. They tolerate walking at a slow pace and can do it for 40-60 minutes.
Representatives of the fourth functional type are characterized by frequent attacks of angina at rest and stress. Thus, pain can occur even with minor loads, say, walking 100-150 m. Long walks can be recommended for them, but with mandatory rest periods.
Let us recall that among a number of risk factors for “angina pectoris” is limitation of physical activity. Adequate physical exercise will help expand the coronary vessels, improve the nutrition of the myocardium (heart muscle), improve the emotional and mental state, activate metabolic processes and ultimately help the body resist the development of atherosclerosis, against which coronary heart disease usually occurs.
Below is an approximate set of exercises available for patients with the first or second functional type. If during exercise you suddenly feel pain or discomfort in the heart area, you should reduce the load or even interrupt the exercise.
A set of exercises for coronary heart disease
- Sitting on a chair, hands down. Stretch your arms to the sides to shoulder level, take a deep breath, lower them down and exhale. Repeat 3-5 times.
- While sitting, keep your hands on your waist. Raise your right arm across the side to shoulder level, inhale, return to the starting position, exhale. Same thing for the left hand. Repeat 3-5 times.
- Standing, spread your legs, bend your arms horizontally at the elbows and hover in front of your chest. Rotate the body with arms raised - inhale, return to the starting position, exhale. Repeat 4-6 times.
- Normal walking (30 seconds), then with a slight acceleration (1 minute).
- Standing, legs slightly to the sides, arms also to the sides and raised at shoulder level. Perform first in one direction, then in the other, circular movements with your shoulders. Repeat 5-7 times forward and backward.
- Standing, hands on the back of the head in a lock. Place your left foot to the side on your toe, tilt your body to the left, straighten up and take the starting position. Same thing with the right leg. Repeat 3-5 times.
- Standing, hands rest on the back of the chair. Sit down - exhale, stand up - inhale. Repeat 4-6 times.
- Standing, hands on waist. Spinning the head with full amplitude to the right, then to the left. Perform 3-5 times in each direction.
- Walking is simple, alternating with acceleration (3 minutes).
- Walking is simple (30 sec), then with a high hip lift (30 sec).
- While standing, alternately bend the body to the right, then to the left while bending the arm of the opposite side (the so-called “pump” exercise), the amplitude is maximum. Repeat 4-6 times in each direction.
- While standing, we hold our hands in front of us and spread them slightly. Raise your left leg and touch your right palm, returning to the starting position. Same thing with the right leg. Repeat 4-6 times.
- We lie on our stomach, stretch our arms along the body and rest our palms on the floor. We raise our straightened legs one by one. Perform 4-6 times with each leg.
- Sitting on a chair, we clasp our hands in a “lock” and hold them on our knees. Turn your palms out, raising your arms in front of you to shoulder level. Repeat 6-8 times.
- Sitting on a chair, right leg in front, left leg under the chair, hands resting on the seat. Changing the position of the legs. Perform 8-10 times.
Exercises, gymnastics and performance features
The main goal of rehabilitation for ischemic heart disease is to restore normal functioning of the cardiovascular system. In addition, the exercise therapy complex increases immunity, improves the general condition of the body and returns it to its previous activities. The following stages are distinguished:
- adaptation – assess the patient’s health status;
- the main one is to select an individual training program;
- the final period is the final examination of the patient and the selection of exercises to practice at home.
Exercise therapy for IHD is prescribed depending on the functional class of the disease (for IHD there are four gradations).
In group I, exercise is selected for all muscles with full range of execution. Classes are structured according to the type of training regime. In addition to standard exercises, this category of patients is allowed short-term exercises with greater intensity. For walking, first use a distance of 5 km and gradually increase it to 8-10. A special feature of the complex for this group is jogging, which is contraindicated for the rest. Swimming is also included. Aqua training is gradually increased to 65 minutes. Supplement with sports games (basketball, ping-pong, etc.). The maximum permissible heart rate is 140 beats per minute.
A gentle training regimen is necessary for patients of group II . Charging is carried out at a moderate pace. They start walking at a distance of 3 km and gradually increase to 6-7 km. Swimming lasting no more than 50 minutes is allowed. The level of increase in heart rate should not exceed 10%.
Patients of group III are shown a gentle exercise regime. Measured walking begins at a distance of 450 m, increasing its size daily by 200-400 m. This category of patients can exercise with minimal intensity. The increase in heart rate should not exceed 110 beats/min. At the first symptoms of tension, deterioration of the condition, the occurrence of tachycardia or pain in the heart, immediately stop exercising.
Recently, patients with the fourth functional class were not allowed exercise therapy due to the risk of complications. Today, thanks to the development of modern medicine, a special form of treatment has been compiled for these patients. Classes for this category are held exclusively in a hospital and only after stabilization of the condition.
Physical activity for coronary heart disease
According to modern medical data, a large number of factors can contribute to the development of IHD (coronary heart disease). Among the most common and “aggressive” ones are poor heredity, alcohol abuse, smoking, chronic stress, metabolic disorders due to poor nutrition, chronic fatigue, and physical inactivity. Of course, it is almost impossible to get rid of a hereditary predisposition to IHD, and you cannot completely protect yourself from stress. But you can adjust your lifestyle so as to avoid the other factors mentioned above. First of all, you should quit smoking, optimize your diet and ensure proper physical activity on the body.
The benefits of physical activity:
- Regular physical activity allows you to stay toned and in good shape.
- With regular physical activity, the amount of “useful” lipids in the blood increases, which helps reduce the risk of developing atherosclerosis.
- The likelihood of blood clots is reduced.
- Blood pressure is normalized, which helps reduce the risk of cerebral hemorrhage (stroke).
- Physical activity promotes weight loss and prevents the development of diabetes.
- Regular exercise helps improve mood, normalize sleep, and make it easier to cope with stressful situations.
- Regular physical activity reduces the risk of developing osteoporosis, the most common cause of bone fractures in old age.
Regular physical activity is beneficial for everyone, as it allows you to protect yourself from the development of many unpleasant diseases. But, unfortunately, it is only the illness itself that often pushes us to change our lifestyle and regular exercise.
Only certain types of physical activity are suitable for patients with coronary heart disease.
IHD develops as a result of acid starvation, which leads to the formation of atherosclerotic plaque. The plaque causes the artery that supplies the heart to narrow, causing less oxygen-rich blood to reach the heart muscle. In this case, the intense work of the heart becomes difficult and, under heavy loads, angina pectoris develops - a painful attack of the heart muscle.
Naturally, angina attacks require limited physical activity. Often, in order to get rid of angina, it is necessary to resort to medication, or even surgical treatment. In the case of a severe heart attack - a heart attack, patients even begin to be afraid of physical activity and, in an effort to “protect” the heart, often limit movement to the point of giving up walking.
For patients with angina and those who have had a heart attack, physical activity can have twofold meaning:
- On the one hand, excessive physical activity and intense physical activity can provoke attacks of angina pectoris and lead to a second heart attack - such excessive activity should be avoided.
- On the other hand, moderate physical activity and periodic exercise (no more than 40 minutes 5 times a week) are very beneficial.
Moderate physical activity helps increase the level of good cholesterol, which prevents the further development of atherosclerosis, reduces the rate of development of heart failure, strengthening the cardiovascular system. Regular aerobic exercise helps normalize the functioning of collateral blood flow - an interarterial connection that serves to redistribute blood flow, which helps to increase the amount of oxygen-rich blood reaching the heart muscle.
As medical studies show, physical activity in patients who have had a heart attack helps reduce the risk of a second heart attack by 7 times, and reduce mortality by 6 times, compared with patients who prefer to reduce physical activity as much as possible.
Therefore, for patients who have had a heart attack, performing normal household activities (light daily housework) is mandatory. After an inpatient course of treatment, it is preferable for such patients to undergo a course of physical rehabilitation under the supervision of specialists in a cardiological sanatorium. If rehabilitation in a sanatorium is impossible for one reason or another, it is necessary to undergo a course of physical rehabilitation on an outpatient basis under the supervision of a cardiologist.
The easiest option for physical activity in this case is daily walking. At the same time, you should not overload yourself: the walk should take place at a slow or moderate pace (depending on how you feel), for half an hour to an hour, but not less than 5 days a week. If during a walk you feel weak or tired, you need to take a break - sit down on a bench or return home at a slow pace. Don't be upset - you will be able to go through more and more during the rehabilitation process. However, an increase in physical activity, just like the beginning of physical exercise, after hospitalization must be agreed upon with a physical therapy specialist or the treating cardiologist.
Physical activity should never lead to another attack of angina. During exercise, severe shortness of breath or rapid heartbeat is unacceptable. During physical activity, you need to monitor your heart rate - its frequency should increase in accordance with the increase in load. In this case, the optimal increase in heart rate should be determined by the attending physician on an individual basis, according to the severity of coronary artery disease and associated pathologies.
In the first stages of physical rehabilitation, heart rate can increase by no more than 20 - 30%, approximately 15 - 20 beats per minute. If the loads are tolerated without complications, an increase in heart rate can be allowed by more than 30%, however, no more than the value calculated using the following formula: 200 - the patient’s age. For example, for a patient with coronary artery disease aged 60 years, the maximum permissible heart rate should not exceed 140 beats per minute.
Leading Russian specialist in the field of rehabilitation of patients with heart diseases, Professor D.M. Aronov, developed recommendations for physical activity, depending on the functional class (severity of manifestation) of the disease. According to the tables below, developed by Professor D.M. Aronov, it is possible to determine the permissible load in each specific case.
Remember that, depending on the severity of the manifestation, angina is divided into four functional classes, where I is mild angina, in which attacks occur only during very intense physical activity, and IV is the most severe angina, in which an attack occurs at the slightest physical activity and even at rest. Prohibited loads, permitted loads - with the sign “+„. The number of “+” signs indicates the permissible intensity and volume of loads.
Daily physical activity
The role of exercise therapy in rehabilitation for ischemic heart disease
In the treatment of cardiac pathology, a key role belongs to drug therapy and surgical interventions.
In addition, the importance of preventive measures cannot be underestimated: rational nutrition, avoidance of bad habits. And in no case do they forget about the importance and healing properties of physical activity. A properly selected set of exercises has a good therapeutic effect and helps to avoid complications. Awareness of this fact formed the basis of the method of physical therapy, which today is widely used in the fight against the consequences of heart disease. With cardiac rehabilitation:
- blood pressure levels are normalized;
- the efficiency of the heart increases;
- myocardial trophism improves;
- immunity is strengthened;
- con increases;
- the level of cholesterol, triglycerides and blood glucose decreases;
- the frequency of heart attacks decreases.
Recently, American scientists have proven the fact of the reverse development of atherosclerotic changes when performing physical activity. And although the experiments were carried out exclusively on animals and in the future the value of this theory in relation to humans may be refuted, today it is stated with 100% probability that regular physical activity slows down the rate of the atherosclerotic process.
Exercise therapy should become a daily norm of life for patients with cardiovascular pathology. However, you cannot practice on your own and uncontrollably. In each case, you need your own training program and a specially designed set of exercises. That’s why this type of recovery is prescribed by a cardiologist or rehabilitation specialist.
Exercise therapy for diseases of the cardiovascular system
It is known that the heart ensures the movement of blood through the vessels. But the force of contraction of the left ventricle alone is not enough to ensure normal functioning of the heart. Extracardiac factors play a major role in blood circulation. For diseases of the cardiovascular system, along with drug treatment, therapeutic exercises are recommended. Exercises allow you to maximize the effect of extracardiac (non-cardiac) circulatory factors and contribute to the normalization of impaired functions. Therapeutic exercise is often used for diseases of the circulatory system in the acute period, as well as during recovery, and is subsequently used as maintenance therapy.
The main contraindications to physical therapy include: acute phase of rheumatism, endo-, myocardium; serious disturbances of the cardiac conduction system and rhythm; circulatory failure in the third stage, acute heart failure.
Methods of influence
The method of exercise therapy directly depends on the characteristics of the course of the disease, as well as the degree of insufficiency of the coronary and general circulation. Physical exercises, starting positions and the amount of load are selected based on the motor mode assigned to the patient.
The effect of exercise therapy in diseases of the cardiovascular system
Myocardial infarction: exercise therapy
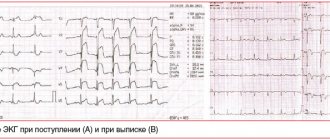
Myocardial infarction is focal or multiple necrosis of the heart muscles, which is caused by acute coronary insufficiency. The tissue susceptible to necrosis is replaced by a scar after some time. A heart attack is characterized by severe pain in the heart area, increased heart rate, decreased blood pressure, drowsiness, and suffocation. An ECG allows you to determine the location of the infarction and its severity. The first three days are characterized by an increase in body temperature, acceleration of ESR, and the appearance of leukocytosis.
Rehabilitation of patients with myocardial infarction is divided into three stages. At each stage, the patient undergoes a course of physical therapy.
The main form of physical therapy at the first stage is massage, walking up the stairs, and measured walking. If the patient’s course of a heart attack is not complicated, then classes can begin on the 2-3rd day, by which time the acute signs of a heart attack have subsided. The timing of the start of classes, as well as the load, is determined strictly individually and directly depends on the nature of the stage and the severity of post-infarction angina.
Forms of therapeutic physical education at the second stage: therapeutic exercises, walking in strictly defined dosages, walks and exercises on exercise machines, walking on stairs, lightweight elements of games, applied sports exercises, massage, occupational therapy. The classes are practically no different from those conducted in the hospital at the first stage. The pace of classes and the number of repetitions are accelerated, exercises are used at the gymnastic wall, exercises with various objects. The procedures are carried out in groups, the duration of the lesson is 30 minutes.
Exercise therapy at the third stage: physical exercises recommended for people with poor health and reduced physical performance are used. Therapeutic walking, walking on stairs, which involves climbing to the 3rd-5th floor, 2-3 times, light sports games and exercises on exercise equipment, and massage are used.
Arterial hypertension is a fairly common disease characterized by increased blood pressure. There are three stages of hypertension.
The first stage involves an increase in blood pressure without involvement of target organs. The second stage – blood pressure is increased and target organs are involved: kidneys, fundus, heart. The third stage is increased blood pressure and damaged target organs: kidney failure, stroke, heart attack, heart failure.
The objectives of exercise therapy for arterial hypertension are to lower blood pressure, prevent crises, and generally improve the patient’s condition. Exercise therapy for arterial hypertension includes: dosed walking, therapeutic exercises, general exercise equipment, therapeutic swimming and exercise in the pool, massage.
Heart defects: exercise therapy
Physical therapy for heart defects is a combination of active and breathing exercises. Classes are conducted at a slow pace, without intensification, lasting 10-15 days. In the next 2-3 weeks, patients are prescribed therapeutic exercises.
Coronary heart disease: exercise therapy
Means of physical therapy for coronary heart disease: therapeutic exercises, physical exercises in water, swimming, dosed walking.
Doing exercises
A set of exercises for coronary heart disease :
- Starting position – hands on the belt, standing above the seat of the chair. We move our hands to the sides - inhale, return our hands to the belt - exhale.
- The starting position is the same. We raise our hands up and inhale, bend forward and exhale.
- Starting position – standing, hands in front of the chest. We move our arms to the sides - inhale, starting position - exhale.
- Starting position: standing by a chair. Sit down - exhale, stand up - inhale.
- Starting position - sitting, bend your right leg - clap, return to the starting position. Do the same with the left leg.
- Starting position – sitting on a chair. Do not hold your breath, squat in front of the chair, then return to the starting position.
- The starting position is the same, legs straight, arms forward. Bend your legs at the knees, place your hands on your belt, then return to the starting position.
- Starting position – standing. We move our right leg back, arms up – inhale, starting position – exhale. Repeat for the left leg.
- Starting position – standing, hands on waist. Perform tilts to the right and left.
- Starting position – standing, hands in front of the chest. We move our arms to the sides - inhale, starting position - exhale.
- Starting position – standing. We move our right leg and arm forward. The same with the left leg.
- Starting position – standing, arms up. We sat down, then returned to the starting position.
- The starting position is the same, arms up, hands in the lock. We rotate the body.
- Starting position – standing. Take a step forward with your left foot - arms up, return to the standing position. Repeat for the right leg.
- Starting position – standing, hands in front of the chest. Make turns left and right with arms outstretched.
- Starting position – standing, hands to shoulders. Perform alternate straightening of arms.
- Walking in place.
Monitoring the patient and monitoring the results
Exercises and rehabilitation methods are prescribed by the attending doctor. He is responsible for their appropriateness and necessity.
Classes are prescribed below the level of threshold loads for the patient, and at the same time they are with the maximum possible effect of stress and training of the heart. The most important criterion for dosing physical effort is heart rate. Changes in heart rate most quickly and accurately reflect the work of the heart and the adequacy of the load being performed. If the permissible limits are exceeded, the exercise is performed with less intensity or replaced with another. The deterioration of the patients' condition is unacceptable. In this case, classes are temporarily canceled and the plan is changed.
The rehabilitation program for patients with coronary heart disease lasts approximately one year. If no complications arise during this period, more complex exercises are prescribed. Additionally, some patients are recommended cycling, working out in the gym, and skiing.
Be sure to remember that even with correctly selected treatment and its effectiveness, constant medical monitoring of the patients’ condition and preventive examinations every two to three months are necessary. The exact frequency is determined by the attending physician.