- Causes
- Development mechanisms
- Kinds
- Symptoms and complications
- Diagnostic methods
- Treatment
- Disease prognosis
- Prevention measures
Parasystole is the appearance of additional ventricular contractions that come from an additional pacemaker (paracenter). It is usually not dangerous, but may indicate organic heart pathology. The arrhythmia itself rarely requires treatment. It is necessary only if parasystolic tachycardia develops or symptoms appear that worsen the patient’s quality of life. In Belgium, parasystole can be cured once and for all: doctors use transcatheter radiofrequency ablation to destroy the focus of parasystolic activity.
Where should parasystole be classified in the classification of arrhythmias?
Classifications of arrhythmias are based on different characteristics, each with its own disadvantages:
- according to the anatomical location of the ectopic focus - the mechanism of development of disorders is not taken into account;
- according to the mechanism of violation of automaticity, conductivity or excitability - in most cases there is a violation of all functions at once;
- by rhythm frequency - the algorithm for determining the type begins with the diagnosis of normo-, tachy- and bradyarrhythmia, but it requires further clarification using electrocardiographic (ECG) studies;
- depending on the mechanism of impulse occurrence (in a normal and ectopic focus) - separate identification of conduction disorders and combined disorders.
Parasystole is closest to the last option. Let us clarify that we understand the term as additional contractions of the heart muscle in response to impulses coming from the “paracenter” located in any part of the heart.
Diagnostics: signs on ECG and Holter
A complete examination of a patient with ventricular parasystole includes the following methods:
- History: family, life, illness.
- Physical examination.
- Blood tests: general, biochemical, hormonal profile.
- Urine tests: general.
- ECG studies: simple ECG, under load, CMEG, EchoCG.
- MRI.
- EFI.
In simple cases, it is enough to conduct an electrocardiographic study, which will show all three specific signs of pathology.
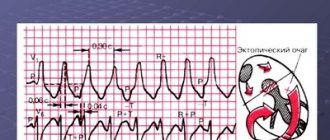
The ECG speed is 25 mm/second. The distances from the normal wave to the pathological wave are not the same, and the difference will be more than 1/10 of a second, which indicates that the parasystole is not associated with sinus contractions. Confluent complexes occur with the simultaneous arrival of sinus and ectopic impulses.
In the image, the upper arrows point to the parasystoles, and the lower ones point to the places where they would be if not for the refractoriness (decreased excitability) acquired by the myocardium after sinus contraction.
The middle line contains three parasystoles in a row, the last of which is a confluent complex.
The second ECG is slightly different.
In this case, sinus rhythm is much more frequent than parasystole; ECG signs of arrhythmia are therefore different. In particular, two pathological complexes in a row are not recorded.
Separately, I would like to point out the presence or absence of the third electrocardiographic sign of ventricular parasystole, the law of “multiplicity”. It is not always detected, or rather, only in 29% of cases. Several circumstances prevent its manifestation:
- the sinus node imposes its rhythm on the paracenter (PC);
- blockade of entrance to or exit from the PC;
- modulation of the PC operating cycle;
- temporary elimination of PC;
- PC arrhythmia;
And in 8% of cases the reason for the absence of the third sign remains unclear. Because of this unreliability of the “multiplicity law”, it can be neglected when diagnosing ventricular parasystole.
Education mechanism
Automatic generation of impulses is a physiological function of myocardial cells. This is how they differ from ordinary muscle tissue. Typically the impulses originate in the sinus node. From here they spread to all parts of the heart and cause the correct rhythm.
The parasystolic center may arise elsewhere and contribute to premature contractions, extrasystoles, or a more complex disorder - atrial fibrillation.
The main reasons for such changes should be sought in the suppression of the main sinus node, its damage (A - normal, B - abbreviation from the underlying node)
Increased tone of the vagus nerve is important. This mechanism predominates in healthy people and athletes.
It is important that in prognostic terms, additional contractions do not contribute, but rather interfere with the normal functioning of the myocardium, since they do not allow complete relaxation in the diastole phase. Parasystolic contractions are premature and do not create the necessary volume of blood to nourish the body.
There is a possibility of internal blockade of the propagation of ectopic waves. But with a weak sinus node, the parasystolic focus turns out to be active. Usually the impulse with the highest frequency “wins”.
Types of parasystoles
Depending on the location of the source of the second rhythm, the following types are distinguished:
- ventricular parasystole;
- atrial;
- from the atrioventricular node;
- polytopic (from different places).
In addition, in relation to the normal contraction, extrasystole can be:
- early and late;
- single, group and allorhythmic (constant rhythmic alternation).
According to the frequency of the ectopic rhythm:
- rare (up to 10 per minute);
- medium (10–30);
- frequent (more than 30).
There are temporary and permanent forms. The type of parasystole can be clarified using the ECG picture.
A serious type of parasystole is atrial fibrillation in the form of atrial flutter or fibrillation. With this pathology, there are either many foci of excitation, or the process forms a vicious circle.
Case from practice
37-year-old patient S. was under outpatient observation for several years with a diagnosis of ventricular parasystole. The disease was difficult to tolerate, and treatment did not bring any visible effect. It was not possible to identify pathologies that could provoke parasystole.
S. was anxious and suspicious. She was asked to consult a psychotherapist and undergo endocardial EPS. The patient refused both. The ECG detected single and paired gastric parasystoles.
In a calm state, arrhythmia did not manifest itself. The patient was prescribed B-blockers, which were effective, but after stopping their use, the parasystoles returned.
An interesting situation was revealed after daily monitoring. While the woman was quietly driving in the car, sinus rhythm was observed. And then she gets into an accident, and parasystolic trigeminy immediately appeared, the heart rate rose to 150 with paroxysmal constant-recurrent ventricular tachycardia.
After the situation returned to normal, the rhythm changed to sinus tachycardia with single ectopic complexes, with various intervals before them.
After analyzing these data, the prescriptions were changed: the dose of B-blockers was reduced and Grandaxin, a daytime tranquilizer, was added. The effect was not long in coming. The patient was recommended to consult a psychotherapist and possible radiofrequency ablation.
Why do parasystole centers appear?
There are cardiac and extracardiac causes. In some cases, it is impossible to establish a connection with any cause, then the extrasystole is called idiopathic.
Cardiac ones include:
- ischemia or necrosis in the sinus node area and other places with coronary heart disease, which forces different areas to become active and “survive” on their own;
- inflammation of a focal or diffuse nature in acute and chronic myocarditis (rheumatic carditis, acute infectious diseases, sepsis);
- metabolic changes during dystrophy;
- replacement of myocytes with connective tissue cells with disruption of their functions (cardiomyopathies, cardiosclerosis);
- loss of the ability to restore the required level of energy (circulatory failure);
- hypertrophy of myocardial tissue (hypertension, decompensation in heart failure, cardiomyopathies);
- disruption of the valves (congenital malformations, acquired changes in the valves due to inflammatory processes, injuries).
Non-cardiac causes include concomitant diseases leading secondary to myocardial dysfunction. Most often, these changes are “guided” by endocrine organs when:
- diseases of the thyroid gland (hypothyroidism or hyperthyroidism associated with deficiency or excess synthesis of thyroid hormones);
- diseases of the adrenal glands;
- diabetes mellitus
Activation of parasystolic foci is detected on the ECG when:
- vegetative-vascular dystonia, neuroses;
- anemia (anemia) of various origins;
- overdose of drugs (cardiac glycosides);
- violation of the necessary balance in the electrolyte composition of the blood between potassium, sodium, magnesium and calcium, they are necessary for the implementation of the normal process of excitation and contraction of myocardial cells.
Primary diagnosis
The patient must undergo a general appointment with a therapist. The doctor will try to find out the connection between parasystole and other diseases and will discover a hidden course. It is necessary to talk about your feelings and their dependence on a specific reason.
If the patient is taking medications, it is necessary to reconsider their appropriateness and the possibility of affecting the heart rhythm.
Family history is always taken into account - the tendency of relatives to similar diseases.
Auscultation of the patient allows you to identify arrhythmia and calculate the number of heartbeats. Hypertension at the appointment indicates the role of increased pressure in myocardial tension.
The Holter monitoring method has expanded the search for intermittent arrhythmias and other disorders in time
General blood tests and biochemical tests are carried out to more accurately identify the mechanism of disorders:
- Reduced hemoglobin and red blood cells indicate anemia.
- An altered balance of cholesterol, triglycerides and lipoproteins suggests the development of atherosclerosis in the vessels of the heart.
- Blood glucose levels are the primary diagnosis of diabetes.
- Determination of electrolyte composition shows nutritional deficiencies.
Sometimes the patient is prescribed more in-depth studies of hormonal levels, and consultation with an endocrinologist is recommended.
Recommendations for self-help with extrasystole
- To prevent rhythm disturbances: It is necessary to take the medications prescribed by your doctor, know their names and dosages.
- You should report any side effects from the medications you are taking to your doctor.
- You should accurately and regularly follow all recommendations prescribed by your doctor.
- You need to calm down, sit comfortably, and if you feel dizzy and severely weak, lie down.
Prepared based on materials from the book “Heart rhythm disturbances” Treshkur T.V., Parmon E.V., Ovechkina M.A. and etc.
Methods to rule out heart disease
To identify cardiac causes, a complete examination is necessary, including differential diagnosis of defects, physiological abnormalities, and the consequences of vascular atherosclerosis.
- The ECG quite accurately shows the localization of the second pacemaker, allows you to distinguish the ventricular type from others, and identify allorhythmia. This method is available at the outpatient and clinic level. Allows you to identify signs of heart disease that cause rhythm changes. Conducting stress tests is recommended to identify the latent form (asymptomatic), the connection with physical activity and the influence of nervous regulation. Bicycle ergometry tests, treadmill walking, and stair tests are used.
- If parasystoles appear rarely, then the Holter monitoring method helps: the patient is fitted with electrodes for a day, from which information is recorded even during night sleep. Decoding allows you to determine the cause of the extrasystole.
- Dopplerography is a very informative method for identifying heart defects, the degree of mitral valve prolapse, and myocardial reserve reserves. The image on the screen visualizes the contraction process and its phases. At the same time, a quantitative analysis of indicators is carried out.
- Magnetic resonance imaging (MRI) is the method of choice for diagnosing the correct functioning of all parts of the heart muscle and identifying replacement with scar tissue.
An ECG recording records different distances between the ventricular complexes, a violation of their shape, and the direction of the teeth
Features of symptoms
Parasystole can manifest itself:
- sudden heartbeat;
- sensations of turning over, pressure and temporary weakness of the heart muscle;
- impotence, fatigue, decreased performance, constant dizziness;
- mental pain accompanied by a feeling of fear;
- Preconscious states are accompanied by rapid heartbeat and cough.
The main electrocardiographic symptoms of parasystole are characterized by:
- the complete set of long intersection intervals;
- umbrella frequency from 25 to 65 beats per minute;
- violation of the regularity of sinus rhythm due to lack of connection with parasystoles;
- instability of the gap between the clutches;
- the presence of fluid ventricular complexes (with the coincidence of sinus and parasystolic syndromes).
In some patients, the disease has virtually no clinical manifestations. It was discovered accidentally during an ECG.
Treatment
After identifying the disease that caused parasystole, you should carefully follow the cardiologist’s recommendations on regimen and treatment. In each specific case, different medications are prescribed, so you should not adopt the experience of neighbors or acquaintances.
In your daily routine, it is imperative to allocate enough time for rest, relaxation, exercise, and sleep.
Treatment will not be successful if you abuse alcoholic beverages (including beer) or smoke. You will have to get rid of these habits.
There is no special diet in nutrition, but nutritionists recommend eliminating strong irritants from food:
- fried and smoked meat dishes;
- high-fat dairy products;
- butter and animal fats;
- strong tea and coffee;
- spicy seasonings and sauces.
You should not overeat; it is better to eat often, but in small portions. Preference is given to boiled and steamed fish, poultry, fresh vegetables and fruits.
Very hot or cold foods are not recommended.
For drug treatment use:
- Soothing herbal remedies made from mint, valerian, motherwort. If necessary, the doctor prescribes sedatives.
- To improve metabolism in myocardial cells, Retabolil, Panangin, Riboxin are prescribed.
- For high concentrations of low-density lipoproteins, statins and nicotinic acid injections are recommended.
- β-blockers (Isoptin, Obzidan) are prescribed for organic changes to suppress impulse transmission from paracentres.
The ablation procedure is carried out under X-ray or ultrasound scanning control
Surgical methods are used when drug therapy is unsuccessful or it is impossible to use them (pregnancy). The least dangerous method is radiofrequency ablation of the source of excitation. A catheter with a radiofrequency emitter at the end is brought to the heart through large vessels. The end of the catheter is placed in the area of suspected heterotopic foci and their targeted destruction is carried out. A scar forms at the site of exposure.
Classification
The classification of the disease depends on the location of the additional nodular lesion:
| Type | Pulse source location |
| Ventricular | Ventricle |
| Atrial | In one of the atria |
| Multiple | In the heart chambers (several extra lesions) |
| Combined | In different parts of the heart |
You can also often see this division into three types:
- Atrioventricular parasystole;
- Ventricular parasystole with localization in a specific one ventricle of the heart;
- Atrial parasystole.
Often the atrioventricular and atrial type are considered a common diagnosis of “supraventricular parasystole” (supraventricular).
The atrial form is less common than the ventricular form.
According to the International Classification of Diseases (ICD-10), parasystole has code I45.3.
In addition to the above classification, this condition is divided according to the electrocardiographic characteristics:
- Artificial.
- Transitional-atypical.
- Intermittent - non-permanent form.
- Tachycardic - the number of extra impulses is greater than the main ones.
- Bradycardic - the number of extra impulses is less than the main ones.
- Multiple.
Consequences of parasystole
The most dangerous consequences of uncontrolled parasystole can be:
- ventricular fibrillation, leading to death;
- the formation of chronic heart failure with a gradual decline in the ability of the heart muscle to contract and push blood.
Clinicians and scientists study heterotopic foci (parasystolic) in the heart. The impact of altered neurohormonal regulation on the heart is well recognized. This process is especially important during the period of child growth, adolescence, and menopause. A person should pay the most attention to health during these sensitive periods of life.