Arrhythmia is a disturbance in the normal rate or sequence of heartbeats.
The concept of arrhythmia combines various types of heart rhythm disturbances. For a person aged 20 to 60 years, the average heart rate is 60-80 beats per minute. Contractions of the heart muscle follow each other at almost equal intervals of time. This is the norm. A person gets used to the way his heart beats and does not notice the heartbeat. If the heart rhythm is disturbed, it immediately attracts our attention.
However, arrhythmia is not just a complaint about the feeling of heartbeat. Arrhythmia is established objectively, using instrumental diagnostic tools. Arrhythmia can be detected in the absence of any complaints, and vice versa: complaints of cardiac arrhythmias may not be confirmed instrumentally.
Arrhythmia occurs one and a half times more often in men than in women. Another factor that increases the risk of arrhythmia is age. At 50 years of age, arrhythmia is detected in 1% of subjects, at 60 years of age – already in 10%. However, it can also develop in childhood. Arrhythmia is detected in 0.8% of children.
What is arrhythmia?
The heart works like a pump and ensures continuous blood circulation.
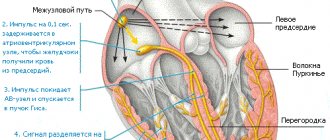
This is necessary to deliver blood enriched with oxygen and nutrients to every cell of the body. In the right atrium of the heart there is the sinus node (SU), the “commander-in-chief” of the heart rhythm. The sinus node generates electrical impulses, under the influence of which the right and left atria first contract, then the right and left ventricles. Other parts of the myocardium can also generate electrical impulses, but in a healthy heart they are suppressed by the sinus node and do not disturb the heart rhythm.
The correct heart rhythm is considered to be sinus rhythm, in which the heart rate (heart rate) is from 60 to 80 beats/min. An arrhythmia is any heart rhythm that differs from normal sinus rhythm.
Heart rate is determined in a state of physical and emotional rest, since this indicator may increase during sports or excitement. It should also be noted that the normal heart rate is a relative value and depends on the individual characteristics of a person. For example, a rapid heart rate can be observed during pregnancy, a slow heart rate in athletes.
Treatment options
There are two treatment tactics: monitoring the rhythm or frequency of the heart. The cardiologist determines how to treat arrhythmia and what to take individually, depending on the case.
Control of the rhythm of contractions - restoration of sinus, that is, normal, heart rhythm. It is achieved by taking antiarrhythmic drugs or electrical stimulation of the heart - cardioversion. Antiarrhythmic drugs have a positive effect on the electrical conductivity of the heart, thereby reducing the likelihood of repeated failures.
They may also prescribe ablation - the impact of radiofrequency pulses on the arrhythmic area of the heart.
Ablation treatment can be successful in 70% of cases or more: it depends on the severity and nature of the lesion, the duration of the arrhythmia, and the size of the heart cavities. Risks associated with the procedure are rare.
Monitoring your ventricular rate helps eliminate heart palpitations and the risk of heart failure. This method is used in cases where it has not been possible to restore a normal heart rhythm, or the patient does not show symptoms.
Frequency control is carried out in several ways:
- reduce the spread of electrical impulses from the atria to the ventricles with the help of drugs,
- ablation is performed to eliminate the delay in pulse propagation,
- a pacemaker is installed to simulate an electrical impulse.
Types of arrhythmia
There are several options for classifying arrhythmias. Depending on the heart rate there are:
- tachycardia (heart rate exceeds 90 beats/min);
- bradycardia (heart rate less than 60 beats/min).
The main classification of arrhythmias is based on what physiological property of the myocardium is impaired - automaticity, excitability, conductivity.
- Violation of myocardial automatism.
Automaticity is the ability of the heart to contract rhythmically without external stimulation under the influence of impulses arising within itself.
Arrhythmias in which the automaticity of the heart is impaired and the sinus node acts as the driver of the heart rhythm are called “nomotopic.” For example, such arrhythmias include sinus tachycardia, sinus bradycardia, and sinus node syndrome. Often nomotopic arrhythmias are diagnosed in absolutely healthy people and are physiological.
Arrhythmias in which the automaticity of the heart is impaired and the pacemaker is located outside the sinus node are called “ectopic” or “heterotopic”. With ectopic arrhythmias, the center of automatism moves to the sections underlying the SG with the formation of abnormal rhythms. Ectopic arrhythmias include:
- atrioventricular rhythm - the pacemaker is the AV node (atrioventricular node);
- migration of the supraventricular pacemaker - gradual displacement of the pacemaker from the sinus node to the AV node;
- idioventricular rhythm - ventricular rhythm.
- Impaired cardiac excitability.
Cardiac excitability is the ability of the myocardium to be excited under the influence of external influences.
Arrhythmias in which the excitability of the heart is impaired include:
- extrasystoles - the appearance of extraordinary contractions of the entire heart or its individual chambers. Depending on the location of the extrasystoles, there are sinus, atrial, nodal, ventricular;
- paroxysmal tachycardia - heart rhythm disturbances, which are characterized by palpitations with a heart rate of 140-220 beats/min. The most common form of this type of arrhythmia is atrial. Less common are atrioventricular and ventricular paroxysmal tachycardias.
- Impaired cardiac conduction.
Conductivity is the ability of the heart to conduct electrical impulses from the point of their origin to the contractile part of the myocardium. If cardiac conduction is impaired, various blockades may occur:
- SA blockade is a violation of myocardial conduction between the sinus node and the atrium;
- interatrial blockade - slow passage of impulses between the atria;
- AV block - arrhythmias in which the transmission of impulses from the atria to the ventricles slows down;
- intraventricular blockade - disruption of the conduction of the His bundle.
Also, arrhythmias in which cardiac conduction is disrupted include Wolff-Parkinson-White syndrome, a congenital heart pathology characterized by the presence of additional conduction pathways, which leads to premature excitation of the ventricles.
- Mixed arrhythmias.
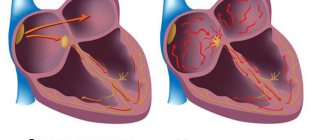
With mixed arrhythmias, several physiological properties of the heart are disrupted. For example, such arrhythmias include ectopic rhythms with exit block and atrioventricular dissociations. One of the most common mixed arrhythmias is atrial fibrillation, in which chaotic electrical activity of the atria is observed with a pulse frequency of 350-700 beats per minute.
Arrhythmia - symptoms and treatment
First aid for an arrhythmia attack
First aid measures depend on the specific arrhythmia, and its type can only be determined by a doctor. Therefore, you should not self-medicate, you need to seek medical help.
Is it possible to cure arrhythmia?
Cardiac arrhythmias vary greatly in prognosis. Some are completely harmless, and some are dangerous. Treatment of cardiac arrhythmias is not always required. First, treatment is appropriate when arrhythmia reduces quality of life. Secondly, it makes sense to treat those arrhythmias that worsen the prognosis, that is, they can lead to premature death or other complications (and the reality of such complications must be proven in clinical studies). Accordingly, asymptomatic cardiac arrhythmias that do not lead to any sensations are not treated in most cases.
In addition, the doctor must try to establish what caused the arrhythmia, and then prove the connection between the suspected causative factor and the arrhythmia itself.
When the decision about the need to treat a particular cardiac arrhythmia is made, the question arises of how to treat it.
Surgery
For many decades, the doctor had no other treatment options for heart rhythm disorders other than medication. Rare exceptions include electrical shock therapy, which delivers a shock using an external defibrillator in a critical situation to eliminate a life-threatening arrhythmia, and transesophageal electrical stimulation of the heart to eliminate some supraventricular tachyarrhythmias.
Since the 90s of the last century, and in Russia since the 2000s, a new treatment method has appeared that is effective for many cardiac arrhythmias - radiofrequency ablation (RFA). The method allows in many cases to permanently relieve the patient of the need to take medications to treat arrhythmias. The essence of the method is a local radiofrequency effect on the source of arrhythmia or on the pathological path of electrical impulse circulation in the heart. The procedure is carried out using a catheter passed to a specific area in the heart through a puncture in a vessel (usually in the thigh). Due to the effect through the tip of the catheter, local heating of the heart muscle area occurs up to 70 °C. As a result, in this place there is a local death of cells involved in the unwanted generation of impulses or in their unwanted conduction. Thus, the conditions for the occurrence and maintenance of certain cardiac arrhythmias, for example, ventricular tachycardia, disappear.
Almost all supraventricular tachyarrhythmias can be treated with RFA: atrioventricular nodal tachycardia, tachycardias involving accessory pathways, atrial flutter, focal atrial tachycardia, and, with less success, atrial fibrillation.[9] In addition, this method treats many types of ventricular tachycardia and ventricular extrasystoles, if it is very frequent (tens of thousands of extrasystoles per day) and comes from one focus.[10]
Another high-tech treatment for potentially fatal ventricular arrhythmias is implantation of a cardioverter defibrillator.[10] This device is capable of eliminating already developed ventricular tachycardia or ventricular fibrillation in two ways: by electrical stimulation of the ventricles at a rhythm exceeding the tachycardia rhythm, or by applying a fairly powerful electrical discharge, which is quite painful, but saves lives. Thus, a cardioverter-defibrillator is used in cases where there is a real risk of sudden death due to ventricular arrhythmias.[13]
Electrocardioversion
Electrical cardioversion (defibrillation) is used when the arrhythmia sharply worsens the patient's condition and is accompanied by a significant drop in blood pressure. It is also sometimes performed routinely to restore sinus rhythm if atrial fibrillation persists.
Pharmacotherapy
However, in many cases, cardiac arrhythmias are treated with medications. Most often, antiarrhythmic drugs are prescribed in the case of atrial fibrillation (atrial fibrillation), in which case the effectiveness of RFA is not so high. Another situation in which antiarrhythmic drugs are often used is frequent premature beats (thousands or tens of thousands of untimely heartbeats per day) accompanied by symptoms. Less commonly, the drug method is used to treat other arrhythmias - for example, ventricular tachycardia, supraventricular tachyarrhythmias.
Unfortunately, few antiarrhythmic drugs are registered in Russia compared to Europe or the USA. Available in our country are “Novocainamide” (still used for intravenous administration in the emergency treatment of paroxysms of atrial fibrillation and rarely ventricular tachycardia), “Lidocaine” (for intravenous administration for ventricular tachycardia), “Etatsizin”, “Allapinin” and “Propafenone”. " These drugs exist in the form of tablets and are prescribed for long-term use in order to prevent the occurrence of a wide range of ari in the form of tablets and solution is also used to eliminate paroxysms of atrial fibrillation - a universal antiarrhythmic drug, but is used mainly as a backup antiarrhythmic. But it can be prescribed for organic damage to the heart (previous myocardial infarction, low cardiac contractility, severe left ventricular hypertrophy, etc.), while Etatsizin, Propafenone and Allapinin cannot be used in these conditions.[11]
Sotalol is an antiarrhythmic drug to prevent attacks of atrial fibrillation, as well as ventricular arrhythmias. Available in tablets.
Another class of drugs for arrhythmia are calcium antagonists - Verapamil and Diltiazem. They are used for some supraventricular tachyarrhythmias, both for long-term use in tablets and to eliminate developed attacks of arrhythmias with a high heart rate.
Beta-blockers form an independent class of antiarrhythmic drugs, although their direct antiarrhythmic activity is low. Their main effect is their ability to reduce the risk of sudden cardiac death, mainly in people with low cardiac contractility and associated heart failure.[11] The most studied in this regard are Metoprolol succinate, Bisoprolol, Carvedilol and Nebivolol.
In the treatment of atrial fibrillation and flutter, the most important place is occupied by antithrombotic drugs, which reduce blood clotting and thereby reduce the risk of blood clots (in these cardiac arrhythmias it is increased). These are Warfarin, Dabigatran, Rivaroxaban, Apixaban, Edoxaban. Accordingly, taking these medications reduces the risk of stroke associated with thromboembolism.
Lifestyle
Some arrhythmias are provoked by stress, abuse of coffee and caffeine-containing drinks, smoking, lack of sleep, physical activity and taking certain medications. Therefore, the doctor first of all looks for a cause-and-effect relationship between lifestyle factors and the occurrence of arrhythmia. Sometimes the patient himself notices this connection. In such cases, if you eliminate the provoking factor, you can get rid of the arrhythmia. However, it is not always possible to detect such a connection.
Folk remedies
If you suspect an arrhythmia, you should consult a doctor, get diagnosed and adhere to the prescribed treatment. Traditional methods of therapy are not scientifically substantiated and can be hazardous to health. Without adequate treatment, arrhythmia can cause serious complications: angina pectoris, myocardial infarction and ischemic stroke.
Causes of heart rhythm disturbances
As a rule, arrhythmia is not the main pathology, but a consequence of other diseases. Causes of heart rhythm disturbances may include:
- sleep apnea syndrome is a disorder of the respiratory system, which is accompanied by temporary cessation of breathing at night, followed by the release of adrenaline and an increase in heart rate;
- arterial hypertension - syndrome of high blood pressure;
- coronary heart disease - a discrepancy between the myocardial need for oxygen and its delivery;
- heart failure - weakening of the pumping function of the heart;
- congenital and acquired heart defects.
- cardiomyopathies - pathologies of the myocardium associated with its mechanical or electrical dysfunction;
- myocarditis - inflammation of the heart muscle;
- myocardial surgery;
- previous heart attack;
- hyperthyroidism - hyperfunction of the thyroid gland;
- lung diseases;
- diabetes;
- infections.
There are arrhythmias that are based on genetic pathologies. For example, the arrhythmia can be caused by congenital long QT syndrome, which leads to ventricular tachycardia.
Risk factors for arrhythmia include:
- physical inactivity or, conversely, excessive physical activity;
- obesity;
- smoking, alcohol abuse;
- chronic lack of sleep;
- hormonal changes in the body. For example, in women, arrhythmia is often diagnosed after the onset of menopause;
- uncontrolled use of drugs that have an arrhythmogenic effect.
Extrasystoles
Extrasystoles (premature contractions) are divided into ventricular and supraventricular.
Ventricular extrasystoles differ from supraventricular extrasystoles:
- wide QRS complex, unlike the usual “correct” complexes
- absence of an atrial P wave (this sign is not absolute, since the atrium can produce a normal excitation wave, and soon after this, ectopic excitation of the ventricles will independently occur, which will be recorded on the ECG as a P wave followed by a wide deformed complex). Holter programs like to mistakenly label such complexes as WPW.
- The absence of the so-called compensatory pause (that is, the RR interval between the previous ES complex and the subsequent one is strictly equal to either double the “correct” interval, or a single such interval in the case of intercalary extrasystole.
↓In this picture there is a single ventricular extrasystole presumably from the LEFT ventricle (the shape of the complex is similar to a RIGHT bundle branch block - see the page on conduction disorders).
↓ Ventricular bigeminy - correct alternation of one normal complex and one ventricular extrasystole (a type of allorhythmia - correct alternation). Extrasystoles presumably from the RIGHT ventricle (have the morphology of a LEFT bundle branch block).
↓ Ventricular polymorphic bigeminy - the shape of the extrasystoles in the center differs from those at the edges, which means that the sources of origin of the extrasystoles are different.
↓ Ventricular trigeminy - correct alternation of two normal complexes and one ventricular extrasystole.
↓ Intercalated ventricular extrasystole is located between normal rhythmic contractions. Some lengthening of the RR interval between complexes adjacent to the extrasystole is explained by the following. The atrial P wave occurred on time, but it was practically absorbed by the T wave of the extrasystole. The echo of the P wave is a small notch at the end of the T extrasystole in lead V5. As you can see, the PR interval after the extrasystole is increased, since there is partial refractoriness of AV conduction after the extrasystole (probably due to reverse conduction of the impulse from the ventricles through the AV node).
↓Paired monomorphic ventricular extrasystole.
↓ Paired polymorphonic ventricular extrasystoles (extrasystoles from different sources, therefore different shapes of the complexes). A paired VES is a “small embryo of ventricular tachycardia.”
Group (from 3 pcs) extrasystoles, according to modern views, refer to the running of tachycardias, supraventricular or ventricular.
↓The ventricular extrasystole, by its refractoriness, blocked the conduction of the normal atrial impulse to the ventricles (a normal rhythmic atrial P wave is visible after the T wave of the extrasystole).
Supraventricular (supraventricular) extrasystoles are narrow (similar to normal) premature QRS complexes. They may have an atrial P wave in front of them (atrial ES) or not (AV nodal extrasystoles). After atrial ES, a compensatory pause is formed (the RR interval between complexes adjacent to the ES is greater than the “normal” RR interval.
↓ Supraventricular (supraventricular) bigeminy - the correct alternation of one rhythmic contraction and one extrasystole.
↓ Supraventricular (supraventricular) bigeminy and aberrant extrasystole (aberrant conduction like blockade of the right bundle branch (“ears” in V1-V2) in the second extrasystole).
↓ Supraventricular (supraventricular) trigeminy - correct repetition of two rhythmic complexes and one extrasystole (note that the P waveform in extrasystoles is different from that of “normal” complexes. This suggests that the source of ectopic excitation is in the atrium, but is different from sinus node).
↓ Intercalated supraventricular extrasystole . In the first “normal” complex after extrasystole, there is a slight increase in the PQ interval, caused by the relative refractoriness of AV conduction after ES. The extrasystole itself may be from the AV node, since the atrial P wave before the ES is not visible (although it may be “absorbed” by the T wave of the previous complex) and the shape of the complex is somewhat different from the “normal” neighboring QRS complexes.
↓Paired supraventricular extrasystole
↓ Blocked supraventricular extrasystole . At the end of the T wave of the second complex, a premature P wave of the atrial extrasystole is visible, but refractoriness does not allow excitation to the ventricles.
↓ A series of blocked supraventricular extrasystoles of the bigeminy type. . After the T wave of the previous complex, a modified atrial P wave is visible, immediately after which the ventricular complex does not occur.
How does arrhythmia manifest?
Arrhythmia may be accompanied by the following symptoms:
- a feeling of interruptions in the work of the heart;
- a feeling of somersault, a jolt in the heart;
- accelerated heartbeat;
- suffocation;
- dizziness;
- general weakness, fatigue;
- exercise intolerance.
The most severe manifestations of arrhythmia are presyncope and loss of consciousness, which are most often associated with a very high heart rate (more than 200 beats/min).
In addition, there are “silent” arrhythmias that are asymptomatic. They are usually diagnosed by electrocardiography.
How is arrhythmia diagnosed?
The main and simplest method for diagnosing arrhythmia is 12-lead ECG
In addition, to detect heart rhythm disturbances, the following are used:
- electrocardiography with physical activity (for example, on a treadmill);
- daily ECG monitoring - continuous recording of an electrocardiogram for a day or more;
- echocardiography is an ultrasound research method aimed at identifying morphological and functional changes in the heart;
- transesophageal electrical stimulation (TEES). During the examination, a special electrode is inserted into the lumen of the esophagus and placed in close proximity to the atria. Next, electrical stimulation of the heart is performed in a certain mode, which leads to physiological tachycardia. In this way, it is possible to quickly and accurately detect the source of the arrhythmia.
Diagnostic methods
To determine atrial fibrillation, a comprehensive examination of the heart and related organs is performed, and the patient’s physical condition is also analyzed.
The examination includes:
- electro- and echocardiography,
- daily or multi-day ECG monitoring,
- Ultrasound of the thyroid gland and hormone analysis,
- clinical and biochemical blood test,
- determination of potassium and magnesium levels,
- lipid profile,
- physical stress testing.
It is convenient to undergo complex diagnostics in a specialized cardiac center: you don’t have to waste energy, time and additional money on visiting doctors in different clinics in your city. The result of the diagnosis should be a detailed plan for further treatment.
How is cardiac arrhythmia treated?
There are several methods for treating arrhythmia:
- drug therapy. The patient can be prescribed both drugs that have antiarrhythmic properties and drugs that do not directly affect the electrophysiological properties of the myocardium. The latter are called upstream therapy. It includes ACE inhibitors, angiotensin II receptor antagonists, statins, corticosteroids, polyunsaturated fatty acids and other drugs. Upstream therapy is aimed at eliminating the causes that lead to arrhythmia: inflammatory processes, high blood pressure, myocardial remodeling;
- implantation of a pacemaker - a medical device that affects the heart rhythm. Most often, a pacemaker is used for slow heart rate and AV block;
- radiofrequency ablation of the heart (RFA) is a surgical intervention during which an electrode is used to destroy the focus of pathological excitation of the myocardium or areas of abnormal impulse conduction.
Paroxysmal tachycardia
Paroxysmal are called tachycardias with a sharp beginning and end (in contrast to gradually “accelerating” and “decelerating” sinus ones). Like extrasystoles, they can be ventricular (with wide complexes) and supraventricular (with narrow complexes). Strictly speaking, a run of 3 complexes, which could be called a group extrasystole, is already an episode of tachycardia.
↓ A run of monomorphic (with identical complexes) ventricular tachycardia of 3 complexes, “triggered” by a supraventricular extrasystole.
↓Running an ideal monomorphic (with very similar complexes) ventricular tachycardia.
↓Start an episode of supraventricular (supraventricular) tachycardia (with narrow complexes similar to normal).
↓This picture shows an episode of supraventricular (supraventricular) tachycardia secondary to persistent left bundle branch block. “Wide” QRS complexes, similar to ventricular ones, immediately attract attention, but analysis of the preceding complexes leads to the conclusion about the presence of permanent LBBB and the supraventricular nature of the tachycardia.
Possible complications and prognosis
First of all, the prognosis of the disease depends on the type of arrhythmia. If the rhythm disturbance is not associated with organic damage to the heart, then it may not cause any particular harm to health. For example, such arrhythmias include supraventricular extrasystoles.
However, there are also very dangerous types of arrhythmias. One of them is atrial fibrillation, which can cause myocardial infarction and heart failure.