Irregular heart rhythm or Heart arythmy occurs when the electrical impulses that initiate the heartbeat do not function correctly, causing the heart to beat too fast or too slow, or irregularly.
Arrhythmias are common and usually harmless. In most cases, a person feels a loss of one or more contractions, interruptions in the functioning of the heart - “it beats, then it doesn’t,” or a very rapid heartbeat. However, there are arrhythmias, the symptoms of which are dangerous, even life-threatening.
Advances in medical technology have enriched the physician with new therapeutic techniques and procedures that make it possible to control and eliminate arrhythmias. In addition, since arrhythmia can worsen, and in some cases, have a damaging effect on the heart (deplete the heart muscle, disrupt the functioning of the valve apparatus, cause an increase in the size of the cavities of the heart), the risk of arrhythmia can be reduced by adopting a healthy lifestyle, including proper nutrition and exercise.
Symptoms of arrhythmia
Arrhythmias may not appear. A doctor can detect an arrhythmia before it shows any signs during a routine clinical examination. But more often, heart rhythm disturbances cause noticeable changes in the condition, which include signs:
- Feeling of palpitations and chest pains
- Very fast heartbeat
- Extremely slow heartbeat
- Chest pain
- Shortness of breath
- Dizziness
- Loss of consciousness or feeling close to fainting
Even such significant symptoms of ill health do not always indicate a serious problem. Very often, people who experience an arrhythmia do not suffer from severe heart disease, while a person with a life-threatening arrhythmia may not have any complaints at all.
Normal heartbeat
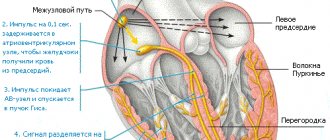
The heart consists of 4 cavities. On each side, on the right and left, there are two pumps: on top of the atrium and below - the ventricles.
During cardiac contraction, chambers with a thin muscle layer and smaller sizes contract, helping to fill the relaxed ventricles with blood. Contraction begins when the sinus node—a small group of cells in the right atrium—sends an electrical impulse that causes both atria to contract. The impulse then travels to the atrioventricular node, located in the very center of the heart and lying at the junction of the atria and ventricles. Leaving the atrioventricular node, the impulse passes to the ventricles. As a result, the latter contract and push blood to all organs.
In a healthy heart, this process occurs evenly and constantly with a heart rate of 60-100 per minute in a calm state. In athletes, especially athletes at rest, the heart rate is usually less than 60, since their heart is much more trained than that of an ordinary person and has great muscle strength, pushing out a large volume of blood per contraction. In children, on the contrary, the pulse is normally more than 100 beats per minute, and in infancy it is 140-160 beats per minute.
Causes of arrhythmia
The most common causes of arrhythmia or the condition leading to its development are heart disease, high blood pressure, diabetes, smoking, excessive consumption of alcohol and caffeine, drug abuse, and stress. In some cases, the causes of arrhythmias may be an overdose of certain medications, the use of dietary supplements and herbal preparations.
Scars can occur for various reasons. The most common of these is acute myocardial infarction. Such a scar prevents the formation of an electrical impulse and/or interrupts the passage of an impulse through the heart muscle.
In a healthy person with a healthy heart, the development of a stable arrhythmia is impossible without the presence of an external trigger, such as an electric shock. This happens primarily because in a healthy heart there are no pathological substrates for the development of arrhythmias, including scar tissue.
On the other hand, in hearts with signs of arrhythmia, the formation and/or propagation of the electrical impulse may be impaired, facilitating the development of the disease.
Any of the following conditions can lead to the development of arrhythmia:
○ Inadequate blood supply
. If blood flow to the heart is reduced for any reason, this can alter the cells' ability to form and conduct electrical impulses.
○ Damage or death of the heart muscle
. Damage or death of the heart muscle leads to a change in the path of electrical impulses propagating through it.
Among the heart disease causes of arrhythmias, the following are of particular importance:
○
Coronary heart disease (CHD)
. Despite the fact that many types of arrhythmias are recorded with ischemic heart disease, the most strongly associated with it are ventricular arrhythmias and sudden cardiac death. The narrowing of the arteries occurs until, as a result of lack of blood supply, part of the heart muscle dies (acute myocardial infarction). This can affect the process of propagation of an electrical impulse throughout the myocardium: small electrical circles of excitation are formed at the border of scar tissue, which disrupt the normal functioning of the heart, causing pathologically fast heartbeat (ventricular tachycardia) and ventricular flutter or fibrillation - ineffective chaotic contractions of the ventricles.
○ Cardiomyopathy
. It manifests itself as primary stretching and thinning of the walls of the ventricles and atria (dilated cardiomyopathy) or excessive thickening and overcontraction of the walls of the left ventricle (hypertrophic cardiomyopathy). With any variant of cardiomyopathy, the efficiency of cardiac output decreases (the amount of blood ejected by the left ventricle into the aorta to nourish all organs and tissues of the body decreases), and part of the blood remains in the left and right ventricles or is thrown back into the atria and the veins flowing into them.
Heart valve diseases. Damage to the heart valves by infectious agents or due to degenerative degeneration leads to narrowing of the valve openings and/or insufficient closure of the valves, i.e. valve insufficiency. When the chambers of the heart become stretched and weakened due to inadequate valve function, the risk of developing various types of heart rhythm disorders increases.
Extrasystole
Extrasystole is an extraordinary contraction of the heart muscle.
Its forms:
| By localization | Sinus Atrioventricular Atrial Ventricular |
| By frequency per hour | Rare (<10) Mid frequency (10–30) Frequent (>30) |
| By density | Single Pairs |
Extrasystoles occur for the same reasons as tachycardia. Often provoke the onset of paroxysm of tachyarrhythmia.
Extrasystole in most cases is asymptomatic, sometimes there are:
- interruptions in heart function;
- a feeling of increased heartbeat or stopping, cardiac arrest.
With heart failure, the course of the disease worsens and the risk of death increases. Single extrasystoles occur in healthy people and do not require correction. They respond well to treatment.
Treatment of extrasystole associated with damage to the heart muscle includes:
- beta blockers;
- ablation of foci of high-frequency extrasystole.
Risk factors for developing cardiac arrhythmia
Risk factors for developing cardiac arrhythmias include:
- ✔ Genetics.
In people with congenital abnormalities of the heart, arrhythmias occur more often. Moreover, a number of arrhythmias (eg, Wolff-Parkinson-White syndrome, some supraventricular tachycardias, some forms of long QT syndrome) are congenital. - ✔ Thyroid diseases.
With increased thyroid function, increased production of hormones occurs, overall metabolism increases, and heart contractions become more frequent and irregular. Atrial fibrillation most often develops. With insufficient thyroid function, metabolism decreases, which causes bradycardia, and in some cases, extrasystole. - ✔ High blood pressure.
This increases the risk of developing coronary heart disease. High blood pressure also causes the wall of the left ventricle to thicken, which can change the way impulses are conducted through it. - ✔ Diabetes mellitus.
Diabetes mellitus in the stage of decompensation (uncontrolled blood sugar levels) greatly increases the risk of developing coronary heart disease and arterial hypertension. In addition, episodes of hypoglycemia (low blood sugar) can be a trigger for the development of cardiac arrhythmias. - ✔ Electrolyte disturbances.
Electrolytes such as potassium, magnesium, sodium and calcium form the basis for the formation, maintenance and conduction of electrical impulses in the heart. Too high or too low concentrations of electrolytes in the blood and in heart cells affect the electrical activity of the heart and can cause the development of arrhythmias. - ✔ Use of stimulants.
Psychostimulants such as caffeine, nicotine, etc. cause the development of extrasystole and can also lead to the development of more severe heart rhythm disturbances over time. The use of amphetamines and cocaine can damage the heart muscle with the development of any of the existing arrhythmias and even lead to sudden cardiac death due to the development of ventricular fibrillation.
Diagnosis of the heart when it works intermittently
- Carefully interview the patient to identify characteristic complaints.
- ECG is the “gold standard” in determining the type of arrhythmia. In paroxysmal forms, an episode of disturbance is not always recorded.
- Registration of ECG throughout the day (Holter monitoring) or week (event monitoring) – diagnosis of arrhythmia paroxysms.
- Ultrasound of the heart through the chest and (or) esophagus. To assess myocardial function, examine the cavities of the heart for clots.
Screening and diagnosis of arrhythmia
To diagnose arrhythmias, the doctor usually asks the patient if they have any heart disease and/or thyroid problems. In addition, specific types of medical testing are always performed to detect arrhythmia. This may be a short or long-term passive recording of an electrocardiogram (a day or more), or an attempt to provoke an arrhythmia while simultaneously continuously recording the heart rhythm.
Passive monitoring methods include:
- Electrocardiography (ECG). During an ECG, electrodes attached to specific locations on the arms, legs, and chest record the electrical activity of the heart. An electrocardiogram examines the intervals and duration of each phase of heart contraction.
- Daily ECG monitoring using the Holter method. A portable ECG recorder is installed for a day or more to record the electrical activity of the heart as a person performs his usual daily activities, as well as during sleep.
- Echocardiography. Allows you to use an ultrasound sensor to obtain an image of the chambers of the heart, clarify their sizes, the movement of the walls and valves and other information.
Arrhythmia can be induced using the following tests:
- Tests with physical activity . Some arrhythmias are triggered or worsened by exercise. During the “stress” test, a treadmill or stationary exercise bike is used. During the test, a continuous ECG recording is made. To perform a “stress” test, medications can be used that stimulate the heart in a similar way to physical exercise. Typically, this method is used when it is impossible to perform physical exercise, as well as to establish a diagnosis of coronary heart disease.
- Tilt table test . When a person has unexplained loss of consciousness, slant tests may be helpful. In this case, rhythm and blood pressure are monitored in a horizontal position for 20-30 minutes. Then a special table is moved to a vertical position and rhythm and blood pressure are also monitored for 10 minutes. In this way, the condition of the heart and the specialized nervous system that controls the functioning of the heart when changing body position and moving from a horizontal to a vertical position is assessed.
- Electrophysiological study and mapping . This study is carried out using the thinnest catheters - electrodes, which are carried into the heart cavity. When electrodes are installed in the area of certain areas of the conduction system of the heart, they can be used to study the propagation of an electrical impulse throughout the heart, induce arrhythmia, while studying its localization and mechanism, and also test the therapeutic effect of various medications. This is the most informative and accurate method for diagnosing most arrhythmias. In addition, when performing EPI, it is possible not only to identify, but also to eliminate the arrhythmogenic focus using a special thermal effect called radiofrequency. In this way, most supraventricular and some types of ventricular tachycardias are eliminated. Currently, this method is also used for atrial fibrillation.
Normally, the regular contractions of our heart are supported by special cells that form the sinus node. This structure is located at the top of the right atrium. (Fig. 1)
Figure 1 Normal formation and propagation of electrical impulses
In some cases, the normal functioning of the heart may be disrupted; patients may experience an irregular, fast or slow pulse, pauses between contractions. All this is called heart rhythm disturbance or arrhythmia.
There are several types of arrhythmia:
Supraventricular rhythm disturbances:
- Atrial fibrillation and flutter
- Supraventricular paroxysmal tachycardia
- Atrial extrasystole
Ventricular arrhythmias:
- Ventricular extrasystole
- Ventricular tachycardia
What is paroxysmal tachycardia?
Under normal conditions, the normal heart rate is between 60 and 100 beats per minute. A heart rate greater than 100 beats per minute is called tachycardia.
With paroxysmal tachycardia, a sudden attack (paroxysm) of rapid heartbeat occurs, usually unrelated to physical activity.
Figure 2 Paroxysm of supraventricular tachycardia with a frequency of 180 bpm.
Paroxysm of tachycardia is a regular heartbeat with a frequency of usually 150 to 200 beats per minute, which is accompanied by weakness and shortness of breath. (Fig. 2) Sometimes patients may lose consciousness. In some patients, these episodes are short-lived and are not accompanied by significant symptoms.
How does extrasystole manifest?
An extrasystole is a premature contraction of the heart, which is felt by patients as a short-term interruption in the work of the heart, after which there may be a short pause followed by the restoration of a rhythmic heartbeat.
Treatment of arrhythmias
Both medicinal and surgical treatment methods are used to treat various types of arrhythmias. Among surgical treatment methods, the most common is catheter ablation.
What is ablation?
Catheter ablation is a minimally invasive operation that eliminates the “source” of arrhythmia using radiofrequency energy (RFA) or local cooling of heart tissue (cryoablation).
The emergence of catheter ablation techniques was the result of intensive development of science and the emergence of new medical technologies over the past 20 years.
Today, the catheter ablation method is widespread throughout the world (more than 1 million operations annually) and is the only treatment method that can radically eliminate a significant portion of cardiac arrhythmias in humans.
Types of catheter ablations
Most often in clinical practice, ultrahigh frequency (radio) frequency current is used - 500 kHz. This type of ablation is called radiofrequency catheter ablation (RFA). The effects of radiofrequency energy are carried out using special controlled catheters installed in the heart under X-ray control. (Fig. 3)
Figure 3 Placement of catheters in the heart during RFA.
Another type of impact on the source of arrhythmia is based on rapid, deep and local cooling of the heart tissue. This type of catheter ablation is called catheter cryoablation. Most often, catheter cryoablation is used to treat atrial fibrillation; a special cryoballoon catheter is used for this purpose. This type of surgery is called catheter balloon cryoablation. (Fig. 4)
Figure 4 Balloon placement in the left atrium during cryoablation.
What types of arrhythmias can be treated with catheter ablation?
All rhythm disturbances in humans are usually divided depending on the location of the “source” of arrhythmia in the human heart into “supraventricular” and “ventricular”. The cause (etiology) of arrhythmias in humans can be various pathological effects on the heart (inflammation, ischemia, etc.), or they can be caused by congenital features (anomalies) of heart development, incl. conduction system of the heart. Often it is not possible to detect the cause of arrhythmia. Such rhythm disturbances (in the absence of other heart diseases) are called “idiopathic”. The catheter ablation method allows in most cases to effectively eliminate arrhythmias that differ in both etiology and development mechanisms.
Benefits of Catheter Ablation
Treatment of heart rhythm disorders can be medication or interventional (surgical). It should be borne in mind that drug treatment involves long-term, often lifelong, antiarrhythmic drugs. Stopping medication or reducing the dose creates conditions for relapse of the arrhythmia. In addition, the use of medications is often impossible due to side effects or contraindicated due to the presence of concomitant heart diseases.
Currently, international and domestic recommendations for the treatment of cardiac arrhythmias consider catheter ablation as the main method of treating a significant part of arrhythmias. Such recommendations are based on the fact that catheter ablation can eliminate arrhythmia without further resorting to the use of antiarrhythmic drugs.
According to the guidelines, ablation is recommended in the following cases:
— as the main method of treatment for arrhythmias, where the use of catheter ablation is accompanied by high efficiency and safety (supraventricular tachycardia, atrial flutter)
-as an alternative treatment, usually when drug therapy is ineffective or side effects of antiarrhythmic drugs develop (atrial fibrillation, ventricular arrhythmias)
About catheter ablation
Preparation
Before performing RFA, the department performs the necessary examination (blood tests, instrumental diagnostic methods) for, as a rule, 2-3 days. On the day of surgery, the patient does not have breakfast; immediately before the operation, he puts on compression stockings (antithromboembolic stockings or elastic bandages).
RFA is performed by interventional arrhythmologists in a cath lab equipped with modern equipment for diagnostics and interventional treatment.
Ablation procedure
As the first stage of the operation, the so-called intracardiac electrophysiological study (ICE), the purpose of which is to clarify the type of tachyarrhythmia and search for the source of the arrhythmia. (Fig.3 and Fig.4)
To do this, a puncture of the vessels (femoral vein and, if necessary, artery) is performed, and special diagnostic electrodes are carried out under X-ray control. When performing VEPI, electrical stimulation of the heart of various parts of the heart is performed in accordance with diagnostic algorithms. This allows you to establish an accurate diagnosis and determine the location of the source of the arrhythmia.
In some cases (with atrial fibrillation), inhalation anesthesia is used as an anesthetic aid; in other cases, local anesthesia is used.
The duration of the operation is determined by its volume and takes from 1.5 to 3 hours.
After ablation
After RFA, a pressure bandage is applied to the puncture site of the vessel and the patient is transferred to the postoperative ward, where he is under the supervision of an anesthesiologist-resuscitator for at least 12 hours. All this time the patient is on strict bed rest.
To exclude possible complications after RFA, all patients undergo a comprehensive postoperative examination.
On average, the hospitalization period for RFA does not exceed 5 days.
Safety and effectiveness
The effectiveness of catheter ablation, depending on the type of arrhythmia, ranges from 70 to 99%. The risk of potential complications after surgery usually does not exceed 1%, but can reach 4-5% for the most complex heart rhythm disorders. The decision to carry out interventional treatment in each case is made by our specialists, taking into account the patient’s opinion, based on full information about the benefits and potential risks of surgical treatment.
Catheter ablation of atrial fibrillation
What is Atrial Fibrillation?
With atrial fibrillation (atrial fibrillation), instead of a regular heart rhythm, multiple electrical waves occur in the atria, leading to chaotic contractions of both atria at a very high frequency. [Rice. 5]
Figure 5. Atrial fibrillation
Atrial fibrillation (atrial fibrillation), as a rule, is manifested by a rapid, irregular heart rhythm, shortness of breath, and poor exercise tolerance. Often, atrial fibrillation is asymptomatic and is discovered accidentally during ECG recording.
Often, patients with atrial fibrillation (atrial fibrillation) are found to have another type of heart rhythm disorder - atrial flutter. [Fig.6]
Figure 6. Typical atrial flutter.
The symptoms of atrial flutter are not much different from atrial fibrillation. The exact diagnosis of these rhythm disturbances and treatment tactics should be determined by a cardiologist-arrhythmologist.
Why and how to treat atrial fibrillation?
Treatment of atrial fibrillation aims to: 1) eliminate the symptoms of arrhythmia, i.e. improving the quality of life of patients; 2) eliminating the threat of developing heart failure; 3) prevention of thromboembolic complications.
According to world medical statistics, atrial fibrillation (atrial fibrillation) is the most common (1-2% in the population) heart rhythm disorder. In a significant proportion of patients (up to 40%), AF is asymptomatic. In this category of patients, drug antiarrhythmic or non-drug treatment (catheter ablation) for AF is usually not carried out. Treatment of these patients consists of monitoring heart rate and administering anticoagulants to prevent thromboembolic complications.
Patients in whom atrial fibrillation is accompanied by the symptoms described above are prescribed continuous antiarrhythmic therapy aimed at preventing relapses of AF. In approximately one third of all patients with AF, it is possible to select an effective antiarrhythmic drug or their combination.
In 30% of patients with symptomatic, poorly tolerated atrial fibrillation, it is not possible to select effective antiarrhythmic therapy, or the use of antiarrhythmic drugs is contraindicated, is accompanied by the development of side effects, or patients do not want to adhere to long-term conservative drug treatment. In this category of patients, in accordance with modern international and Russian recommendations, catheter ablation is indicated.
It should be emphasized that the choice of treatment options in each specific case is the task of a cardiologist-arrhythmologist, taking into account the patient’s opinion and objective medical data.
Catheter and surgical ablation
Depending on the form of atrial fibrillation (paroxysmal, persistent or permanent), the presence of other pathologies of the cardiovascular system and concomitant diseases, 3 types of catheter (or surgical) ablation are used:
Intracardiac catheter ablation is the most widely used non-drug treatment for AF. Catheter ablation is performed in a cath lab using guided catheters moved into the chambers of the heart through vascular access (femoral and subclavian veins). The purpose of the operation is to radically eliminate the “sources” of arrhythmia in the left and (with atrial flutter) right atrium. Currently, two types of catheter ablation have found widespread clinical use: radiofrequency catheter ablation and balloon cryoablation.
· catheter ablation (destruction) of the AV node is a type of intracardiac catheter ablation, which is used in cases where AF is accompanied by a persistently high heart rate when drug control or radical elimination of AF is impossible. Ablation of the AV node is performed only after implantation of an artificial pacemaker (pacemaker).
· Operation “Labyrinth” – surgical ablation of AF. The “maze” operation (MAZE) is used in cases where a patient with AF is indicated for open-heart surgery due to the presence of an “underlying” heart disease: coronary artery bypass surgery, valve replacement, etc. As an independent intervention for AF, the “labyrinth” operation is used in the form of modified minimally invasive operations with thoracoscopic access (through a small incision in the chest) and only if previously performed attempts at catheter ablation are ineffective.
RFA or cryoablation?
According to modern concepts, the key role in the development of AF belongs to the so-called “arrhythmogenic” pulmonary veins (so-called AF triggers) - large vessels flowing into the left atrium. [Fig.7]
Figure 7. Left atrium and pulmonary veins. Multislice computed tomography
That is why most patients with paroxysmal and persistent forms of atrial fibrillation are indicated for catheter ablation (isolation) of the pulmonary veins.
How it works?
With radiofrequency catheter ablation, isolation of the pulmonary veins is achieved by applying a large number of targeted effects using high-frequency current. These effects should form a continuous chain of many sequential coagulative necrosis around each of the veins [Fig. 8A]. When using another technology - balloon cryoablation [video 1], a zone of necrosis around the veins is created due to the effect of low temperature (up to - 60ºC) in a cryoballoon located sequentially in each of the mouths of the pulmonary veins [Fig. 8B].
Rice. 8A - Radiofrequency catheter ablation (RFA); 1-circular diagnostic electrode of the “Lasso” type, 2-catheter for RFA
Rice. 8B — Catheter balloon cryoablation: 3- cryoballoon
Video 1. Balloon cryoablation.
In most cases, complete isolation is achieved with a single cryo-exposure for several minutes, which is an absolute advantage over radiofrequency ablation. Both types of catheter ablations are performed in a cath lab under general anesthesia or deep sedation. These interventions are high-tech types of medical care and should be performed by qualified specialists with sufficient experience in interventional interventions.
Efficiency and safety
The generally accepted definition of the effectiveness of catheter ablation for AF is the absence of any atrial arrhythmias after surgery without the use of antiarrhythmic drugs. Monitoring of effectiveness is carried out clinically (patient self-monitoring) or using long-term ECG recording systems (HM ECG or special implantable heart rate recorders).
One of the main factors determining the effectiveness of catheter ablation for AF is the duration of episodes of fibrillation. In cases where attacks of arrhythmia do not exceed several hours or days (the so-called paroxysmal form) and, as a rule, go away on their own, the operation is most effective. In comparative studies (the international Fire and Ice study), there were no relapses of AF during the first year in 65% of patients both after RFA and after balloon cryoablation. At the same time, there are observations that in individuals without concomitant cardiac pathology, the effectiveness of balloon cryoablation can reach 80-90%.
In patients with persistent AF, i.e. with arrhythmia lasting more than 7 days, and also requiring drug or electrical cardioversion to restore sinus rhythm, the expected effectiveness of catheter ablation is about 50-60%.
If, after catheter ablation, AF recurs with the same frequency and duration, re-intervention is justified.
Complications during catheter ablation of AF can manifest themselves in the form of vascular damage at the puncture site, perforation of the heart wall with the development of tamponade, the formation of blood clots in the heart cavity and thromboembolic complications, thermal damage to the esophagus, the development of phrenic nerve paresis and a number of others. The use of modern high-tech control methods during intracardiac interventions, sufficient experience and qualifications of the doctor allows these interventions to be performed effectively and without a significant risk of complications.
At the same time, it is necessary to clearly understand that the decision to carry out interventional treatment for AF should be made by a doctor with sufficient experience in treating this category of patients, objectively taking into account the pros and cons.
Catheter ablation of AF in the Department of Clinical Electrophysiology and X-ray Surgery of Rhythm Disorders
Interventional arrhythmology has been one of the main directions in the scientific and clinical work of the Department of Clinical Electrophysiology since its founding in 1990. It has almost 20 years of experience in treating various heart rhythm disorders using catheter ablation technology.
Since 2012, the department has introduced a catheter ablation method for AF. Today, the priority method used in the clinical practice of the Department of Clinical Electrophysiology for non-drug treatment of AF is the method of balloon cryoablation. This choice is based on the fact that cryoablation for AF is not inferior in effectiveness to radiofrequency, while being the safest method of interventional treatment of AF, which was proven by analyzing the many years of experience of the world's leading centers in the treatment of AF.
Specialists from the Department of Clinical Electrophysiology conduct a full preoperative examination of patients, perform interventional interventions and provide outpatient monitoring of all patients for at least 1 year after catheter cryoablation of AF. In cases where patients have complex concomitant heart rhythm disorders, complex (one-stage) interventional treatment, or the so-called. “hybrid therapy”, combining catheter intervention and subsequent drug treatment. If AF recurs, repeat balloon cryoablation or radiofrequency catheter ablation may be performed.
Radiofrequency ablation of paroxysmal supraventricular tachycardias
The most common types of paroxysmal supraventricular tachycardias are:
- Paroxysmal atrioventricular nodal reentrant tachycardia or AV nodal tachycardia. It is characterized by the presence of a congenital anomaly - an additional pathway in the AV node, which normally conducts impulses from the atria to the ventricles. This anomaly is the cause of tachycardia (Fig. 9);
Rice. 9. Paroxysm of AV nodal tachycardia on the ECG.
-Paroxysmal tachycardia in Wolff-Parkinson-White syndrome (WPW syndrome) also occurs due to a congenital anomaly - an additional pathway between the atria and ventricles (Kent's point). (Fig. 10);
Fig. 10 Kent bundle of left lateral localization
-Atrial tachycardia can have a source in both the left and right atria (Fig. 11), and can be a consequence of concomitant heart diseases (coronary heart disease, hypertension or valve defects), or have the so-called. idiopathic (without concomitant pathology) nature.
Fig. 11 Sources of atrial tachycardia in the left atrium (indicated by arrows)
An ECG recorded during a paroxysm of tachycardia often does not allow an accurate diagnosis to be made.
It can be clarified by such examination methods as transesophageal pacing (TEPS) or intracardiac electrophysiological study (ECES), which are standard methods for diagnosing arrhythmias.
Surgical treatment of the above types of tachycardias using radiofrequency ablation (RFA) allows you to completely get rid of arrhythmia; the effectiveness of the method is 97-99%. At the same time, the risk of potential complications of RFA, as a rule, does not exceed 1%.
Ventricular tachycardia
With ventricular tachycardia, a pathological impulse circulates in the myocardial tissues of the right or left ventricles.
This type of arrhythmia can occur in healthy individuals without any serious heart pathology. Often these heart rhythm disturbances have a benign course and do not always require treatment.
In other cases, ventricular tachycardia may be the result of serious illnesses such as myocardial infarction, which can cause sudden cardiac death. (Fig.12)
Figure 12 Ventricular tachycardia
Currently, non-drug treatment methods, such as radiofrequency ablation (RFA) or implantation of a cardioverter-defibrillator, are usually used to treat ventricular tachycardia.
To select the optimal treatment method, a comprehensive examination is necessary.
Complications of arrhythmia
.
A number of heart rhythm disorders can increase the risk of developing conditions and diseases such as:
- Stroke
. When the atria fibrillate, they are unable to adequately pump blood to the ventricles. Slowing blood flow in the atria leads to the formation of clots. If a small piece breaks off from the clot, it can enter the bloodstream, spread throughout the body and clog the cerebral arteries, causing the development of ischemic stroke, i.e. damage or death of part of the brain, and sometimes leads to death. - Congestive heart failure
. Due to a prolonged period of bradycardia or tachycardia, such as atrial fibrillation, the heart may not pump efficiently. By controlling your heart rate, you can improve left ventricular contractility and reduce signs of heart failure.
How to get treatment at the Scientific Center named after.
A.N. Bakuleva? Online consultations