TYPES OF HYPERTROPHY OF HUMAN SKELETAL MUSCLES
Samsonova A.V. Types of hypertrophy of human skeletal muscles // Proceedings of the Department of Biomechanics of the University P.F. Lesgafta, 2021.- Issue. 14.- pp. 32-39
annotation
The article provides a classification of various types of human skeletal muscle hypertrophy based on a number of classification characteristics: time of manifestation and duration of preservation; direction of training impact; specific effects on myofibrils. Based on the time of manifestation and duration of maintenance of the training effect, short-term and long-term hypertrophy of skeletal muscles is distinguished. According to the direction of the training effect, myofibrillar and sarcoplasmic hypertrophy are distinguished. Based on the specific effects on myofibrils, it is proposed to distinguish between transverse and longitudinal myofibrillar hypertrophy.
Keywords
skeletal muscles, hypertrophy
HYPERTROPHY
HYPERTROPHY (from hyper... and Greek τροφή - nutrition), an increase in the volume of an organ, tissue, cells, intracellular structures. It occurs both normally and in various diseases, ensuring the stability of homeostasis. G., along with an increase in volume, is often based on an increase in the number of structural units (organ, tissue, cell), that is, hyperplasia. For example, the G. of a parenchymal organ is based on the G. of parenchymal cells, but at the same time the number of stromal elements can increase, and the formation of new vessels (neoangiogenesis) occurs, providing an increased need for nutrition of hypertrophies. organ. Cell growth also occurs due to an increase not only in the volume of its structures, but also in their number. Thus, G. and hyperplasia are two inextricably linked processes.
Normally, G. develops with increased functional demand or neurohormonal stimulation (for example, myocardial G. in athletes, an increase in the volume of the uterus and mammary glands during pregnancy).
Pathological G. can be true (an increase in the mass and functional activity of an organ due to the G. of cells providing this activity) and false (due to the growth of connective tissue of the stroma and adipose tissue with possible atrophy of parenchymal cells).
True G. is divided into working (compensatory), vicarious (replacement), regenerative, neurohumoral G. and hypertrophic. overgrowth.
Working G. develops with increased work of an organ and is characterized by an increase in the volume of its functionally active structures. For example, the cause of myocardial gastrointestinal tract may be various. hemodynamic factors - arterial and pulmonary hypertension, congenital or acquired heart defects. The weight of the heart can exceed normal values by 3–4 times. G. of the bladder wall develops in men with prostatic hyperplasia, which narrows the urethra and secretes hormonal and growth factors that stimulate G. of detrusor cells (the muscle that expels urine).
Vicarious G. develops in one of the paired organs (lung, kidney, adrenal gland, etc.) following the death or surgical removal of the other.
Regenerative blood forms in the parenchymal cells of the myocardium, neurons, hepatocytes, and others around scars during incomplete regeneration.
With neurohumoral G. and hypertrophic. growths, in fact, we are talking about an increase in the volume of the organ basically. due to the processes of hyperplasia of cellular structures, which simultaneously increase in number and volume.
TYPES OF HUMAN SKELETAL MUSCLE HYPERTROPHY
Alla V. Samsonova , Doctor of pedagogical sciences, Professor, Head of Department
Lesgaft National State University of Physical Culture, Sports and Health, St. Petersburg, Department of Biomechanics
Abstract
This article classifies various types of human skeletal muscle hypertrophy on the basis of a number of features: the time of occurring and the retention time; the type of training effect and the specifics of impact on myofibrils. There are short-term and long-term hypertrophy based on a time of occurrence and a retention time. Myofibrillar and sarcoplasmic hypertrophy are distinguished by the type of the training effect. It is proposed to distinguish between transverse and longitudinal hypertrophy on a difference in impact on a myofibrils.
Key words
skeletal muscle, hypertrophy
INTRODUCTION
Skeletal muscle hypertrophy refers to an increase in their volume under the influence of various factors. Such factors may include damage and mechanical stress to skeletal muscles, as well as metabolic stress [17]. Despite the fairly close attention of researchers to this issue, there is still no complete classification of the types of skeletal muscle hypertrophy. Most publications indicate the existence of myofibrillar and sarcoplasmic hypertrophy [5, 6, 9, 19; 17; 8].
The PURPOSE of this article is to develop a classification of skeletal muscle hypertrophy and explain the mechanisms underlying it.
The structure and functions of muscles are described in more detail in my books:
- Human skeletal muscle hypertrophy
- Biomechanics of the human musculoskeletal system
RESEARCH RESULTS
A classification of human skeletal muscle hypertrophy is proposed according to the following classification criteria: time of manifestation and duration of maintenance of the training effect; the direction of the training effect (strength training or endurance training), the specificity of the effect on myofibrils.
- Based on the time of manifestation and duration of maintenance of the training effect, it is proposed to distinguish between short-term and long-term hypertrophy of skeletal muscles.
- According to the direction of the training effect, myofibrillar and sarcoplasmic hypertrophy are distinguished [5, 6, 9, 19, 17; 8].
- Based on the specific effects on myofibrils, it is proposed to distinguish between transverse and longitudinal myofibrillar hypertrophy (Fig. 1).
Rice. 1. Types of human skeletal muscle hypertrophy
SHORT-TERM AND LONG-TERM HYPERTROPHY OF SKELETAL MUSCLES
Characteristics of short-term hypertrophy and the mechanisms underlying it
Most often, hypertrophy of human skeletal muscles is considered as their long-term adaptation to physical activity of various types. However, there is also short-term hypertrophy of skeletal muscles - that is, a change in muscle volume as a result of one training session. Athletes who compete in bodybuilding or body fitness competitions are well aware that muscle volume can be slightly increased if they use a special training technique - pumping.
Pumping (from the English pump - pump, pump) is a strength training technique in which a large number of repetitions of the exercise are performed in one approach (more than 15) with light weights. Rest pauses between sets are approximately 1 minute. After using pumping, the athlete’s subjective sensations can be described as “blowing” of the muscles, “burning” in the muscles, or that “the muscles have become heavier.”
It is believed that the main reason for short-term muscle hypertrophy is the filling of blood in the capillaries surrounding the muscle fibers. Due to the short rest periods between sets, the outflow of blood from the muscles is greatly hampered. However, there are other reasons that cause short-term hypertrophy of skeletal muscles.
It is known [1] that when performing physical exercises, working hyperemia occurs in skeletal muscles, in which some of the blood capillaries that are inactive at rest begin to function. As a result of an increase in the number of functioning capillaries, the volume of skeletal muscle increases briefly, that is, its hypertrophy occurs.
A significant cause of short-term hypertrophy is skeletal muscle hypoxia. Short rest pauses (up to one minute) lead to insufficient oxygen supply to muscle fibers, that is, to their hypoxia[1]. Hypoxia promotes the accumulation of lactic acid in the sarcoplasm of muscle fibers, which quickly turns into lactate. The hydrogen ions released during this reaction damage the sarcolemma of muscle fibers. As a result, water enters the muscle fibers through the aquaporin-4 channels. The resulting “swelling” of muscle fibers leads to an increase in their volume (short-term hypertrophy of muscle fibers), which causes even greater compression of the blood capillaries and the manifestation of hypoxia. The athlete feels this as a “burning” and “muscle swelling.”
It should be noted that type II muscle fibers are more sensitive to changes in osmotic pressure, since aquaporin-4 transport channels are more pronounced in them [17].
After stopping strength exercises, blood flow is restored. Blood capillaries that open during work “stick together” again. Therefore, the effect of pumping does not last long: from 5 to 10 minutes. This time, however, is quite enough for the athletes on the platform to look more impressive.
This issue is covered in more detail in the video “Why do muscles hurt during training? Should you do cardio after training? on my YouTube channel.
Characteristics of long-term hypertrophy and the mechanisms underlying it
It has been proven that skeletal muscle hypertrophy, as a long-term adaptation of skeletal muscles to various factors, does not appear immediately after exposure to these factors, but after a certain period of time (Fig. 2). This period can reach 12 weeks [14].
Rice. 2. The relationship between various mechanisms of increasing muscle strength (J. Hoffman, 2002)
Scientists attribute the initial increase in strength levels to neural influences on skeletal muscles. The delayed manifestation of skeletal muscle hypertrophy is caused by processes occurring in muscle fibers, which lead to an increase in the number of myonuclei. This significantly affects the increase in protein synthesis in muscle fibers [10]. The factors that initiate these processes are: damage and mechanical tension of the muscle, as well as changes in hormonal levels [17].
MYOFIBRILLAR AND SARCOPLASMIC HYPERTROPHY
It has long been established that long-term hypertrophy of skeletal muscles has two types: myofibrillar and sarcoplasmic hypertrophy [5, 6, 9, 19, 17; 8].
Myofibrillar hypertrophy of skeletal muscles is manifested in their long-term adaptation to power-oriented loads. Sarcoplasmic hypertrophy occurs as an adaptation of muscles to endurance training. With this type of skeletal muscle hypertrophy, the volume of sarcoplasm in the muscle fiber increases (Fig. 3).
Fig.3. Diagram showing changes in the cross-sectional area of muscle fiber depending on the type of hypertrophy
It has been shown [8] that the muscle fiber volume (Vmf) can be influenced by the following factors:
Vmv = Smf · lmf · nmf + Vsark (1),
where: Smf is the cross-sectional area of the myofibril; lмф — myofibril length; nmf – number of myofibrils; Vsarco – volume of sarcoplasm.
If the cross-sectional area of the myofibril (Smf), the length of the myofibril (lmf) and the number of myofibrils (nmf) increase, there is a manifestation of myofibrillar hypertrophy, on the contrary, if the volume of sarcoplasm (Vsarc) increases, there is a manifestation of sarcoplasmic hypertrophy.
Characteristics of myofibrillar hypertrophy and the mechanisms underlying it
Changes in the volume of skeletal muscle during myofibrillar hypertrophy can occur in different ways, depending on the impact on the skeletal muscle.
If you imagine a myofibril in the form of a cylinder, then its volume can increase due to an increase in two factors: its cross-sectional area and length.
It is proposed to call a type of myofibrillar hypertrophy, which occurs due to an increase in the cross-sectional area of the transverse myofibrils. An increase in the cross-sectional area of myofibrils occurs due to the addition of thick and thin filaments at their periphery [3, 16]. An increase in the cross-sectional area of myofibrils leads to an increase in the volume of muscle fibers and the muscle as a whole. Muscle strength also increases.
It is proposed to call a type of myofibrillar hypertrophy, which occurs due to an increase in the length of longitudinal myofibrils . An increase in the length of myofibrils occurs if the muscle is in constant stretch.
In humans this is possible in the following cases:
- Increased limb length
A study of myofibrillogenesis in childhood showed that myofibrils “grow” with increasing limb length [16]. In this case, the skeletal muscles are in constant tension, as the distance between the muscle attachment sites increases.
The longitudinal type of myofibrillar hypertrophy will also be observed in patients whose limb length is increased through the use of the Ilizarov apparatus.
- Stretching a muscle after shortening it
To restore the original length of the muscle after its shortening as a result of fixation of the limb after a fracture, it is necessary to constantly stretch it. As a result, the length of myofibrils, muscle fibers and the entire muscle increases. It has been proven that an increase in the length of myofibrils occurs due to the addition of sarcomeres at their ends [7].
- When performing strength exercises
The longitudinal type of myofibrillar hypertrophy is also observed when performing strength exercises in a dynamic mode. It has been proven [4] that with predominant work in this mode, the length of muscle fibers slightly increases, and the length of the tendon decreases .
The third factor influencing the increase in the cross-sectional area of the muscle fiber is myofibril hyperplasia, that is, an increase in the lMF index. G. Goldspink [12] proved that myofibrils can split longitudinally. They also showed that the myofibrils that were cleaved were approximately twice as large as the myofibrils that were not cleaved. The breakdown of myofibrils can lead to an increase in their number.
Myofibrillar hypertrophy is based on damage and mechanical tension of skeletal muscles, as well as metabolic stress [17]. Damage to muscle fibers leads to activation of satellite cells, their division and an increase in the number of nuclei in muscle fibers. An increase in the number of nuclei leads to an increase in protein synthesis [7]. Mechanical tension in skeletal muscles activates a large number of signaling pathways that increase protein synthesis [17] . In addition to damage and mechanical stress of skeletal muscles, during strength training, the concentration of various hormones in the blood increases [15], such as somatotropic hormone (growth hormone), testosterone, insulin-like growth factor (IGF-1), cortisol, etc. Changes in the metabolic background lead to increased protein synthesis, as well as their catabolism in various time periods after training exposure.
Physiological hypertrophy[edit | edit code]
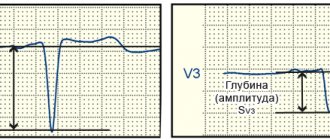
The following signs are typical for physiological cardiac hypertrophy in athletes: 1) certain amplitude characteristics of the teeth of the QRS complex; 2) lack of QRS expansion; 3) normal time of local electronegativity; 4) absence of disturbances in depolarization of mixing downwards of the S-T segment, deformations or inversion of the T wave; 5) increase in heart volume over 11 ml/kg.
The ECG shows signs of hypertrophy predominantly of the left ventricle. The most sensitive electrocardiographic indicators of physiological left ventricular hypertrophy in athletes, in order of decreasing accuracy, are: Rv5-6 > 33 mm, SV1 + Rv5-6 > 53 mm, sum of QRS amplitudes in leads V2, V5, aVF > 93 mm, Ravf 23 mm, Rmax + Smax in precordial leads > 55 mm.
The most sensitive electrocardiographic indicators of physiological right ventricular hypertrophy in athletes, in order of decreasing accuracy, are: Rv1 + Sv5 > 11 mm, SV5-6 > 7 mm, Rv1 > 7 mm. Electrocardiographic signs of right ventricular hypertrophy are less reliable than signs of left ventricular hypertrophy. The combination of several signs of hypertrophy on the ECG allows us to speak with greater confidence about its presence.
It is possible to use separate indexes. Thus, with left ventricular hypertrophy, the Sokolov-Lyon index (mV) and the total voltage of the R waves increases in both standard and left chest leads. Moreover, these signs are more pronounced in men.
When analyzing an ECG, it is necessary to take into account the age-related characteristics of the child’s body. Thus, in children aged 2-12 years, criteria can be used to assess ventricular hypertrophy.
| Left ventricular hypertrophy | Right ventricular hypertrophy | ||
| 1. | R aVL > 8 mV | 1. | R aVR > 4 mV |
| 2. | R V6 > 25 mV | 2. | RV4 > 17 mV |
| 3. | Q V5-6 > 4 mV at R > 20 mV | 3. | RV1 + S V5 > 9 mV |
| 4. | Internal deviation time (IDT) in V5 > 0.045 s | 4. | R/SV1 > 4 mV |
| 5. | EOS deviation to the left | 5. | Shape of the ventricular complex as qR in V1 |
| 6. | T V5-6 flattened or negative | 6. | VBO in V1 > 0.03 s |
| 7. | EOS deviation to the right > 110o |
With myocardial hypertrophy of both ventricles, diagnosis can be difficult due to the fact that the signs of hypertrophy of both ventricles can be mutually leveled.
M.K. Oskolkova (1986) indicates that in the presence of signs of right ventricular hypertrophy, the following criteria indicate hypertrophy of both ventricles:
- dominant RV5 wave (height may be normal) with high positive T waves in these leads;
- increase in q wave amplitude in V5 and V6;
- EOS deviation to the left.
In the presence of signs of left ventricular hypertrophy, the detection of one of the following criteria indicates hypertrophy of both ventricles:
- dominant R or R' waves in lead V1, and its amplitude may be normal;
- the amplitude of the R wave is greater than the amplitude of the q wave in lead aVR;
- The S wave is larger than the R wave in lead V6.
Disturbances in repolarization processes are affected by the state of the autonomic nervous system. Thus, disturbances in the process of repolarization of the ventricular myocardium at rest are detected in children with hypersympathicotonic autonomic reactivity and initial eutonia (in 28%).
During functional tests, disturbances in the process of repolarization of the ventricular myocardium are detected in 25% of children with hypersympathicotonic and in 50% of children with asympathicotonic autonomic reactivity, regardless of the initial autonomic tone.
The severity of respiratory arrhythmia is one of the important indicators of the functional state of the heart: if fluctuations in the duration of the R-R intervals exceed 0.3 s, sinus arrhythmia indicates a violation of the regulation of the sinus node and may be a sign of overtraining.
It is important to identify extrasystole. Along with extrasystole at rest, extrasystole can be observed directly during work and in the recovery period. It is generally accepted that extrasystolic arrhythmia recorded during physical activity indicates a certain prepathological state of the heart muscle. Extrasystole at rest is considered more favorable. Some authors believe that the disappearance of extrasystole recorded at rest during physical activity indicates the “harmless” nature of the latter. However, it should be noted that recent experience in sports medicine, obtained through long-term radiotelemetric observations, indicates that extrasystole is an unfavorable sign, regardless of whether it is recorded at rest or during physical activity.
The causes of extrasystoles in athletes are very diverse. They can develop as a result of myocardial overstrain, in diseases resulting in intoxication of the heart muscle, in violation of the nervous regulation of cardiac activity, disorders of mineral metabolism, etc. It must be borne in mind that in athletes, during muscular work, the content of catecholamines in the blood naturally increases, increasing the excitability of the myocardium.
Subjectively, extrasystole in athletes is usually felt in the form of “interruptions” in the work of the heart. With such sensations, an electrocardiographic study is necessary. The occurrence of extrasystoles in athletes should be analyzed by the coach and the doctor in the light of the individual training regimen.
First-degree atrioventricular block (P-Q interval greater than 0.22 s) is observed in athletes with severe fatigue or overtraining and requires medical intervention and significant correction of the training regimen.
Intraventricular conductivity in athletes is most often at the upper limit of normal, which corresponds to the range of 0.06-0.09 s. In some athletes (especially with myocardial hypertrophy), the duration of the QRS complex may be equal to 0.1 s.
When WPW syndrome is detected, careful monitoring is necessary. Classes are often prohibited due to the development of a dangerous rhythm disorder - paroxysmal tachycardia, which should not be underestimated.
Athletes often have first-degree or second-degree Mobitz type I atrioventricular block, which primarily reflects increased vagal tone. An increase in P wave voltage and QRS complex in combination with T wave inversion in the lateral leads may also be detected. QRS prolongation, deviation of the electrical axis of the heart, supraventricular and ventricular tachycardia are not characteristic signs and may require further research.
Many athletes experience a decrease in the voltage of T-waves in the standard and left chest leads, and also have low rates of relative metabolic support of the myocardium. These changes are especially pronounced during accelerated training in adolescence.
Detailed data on ECGs for athletes are given in the book JI.A. Butchenko et al. (1980). According to their data, the electrical axis of the heart (EOS) is normal in 50% of athletes, vertical in 30%, deviated to the right in 4%, horizontal in 12%, and deviated to the left in 3%. Vertical EOS is more often observed in football players, skiers, swimmers, water polo players and asthenics under 20 years of age. Horizontal EOS and deviated to the left are more typical for wrestlers, weightlifters, long and middle distance runners and hypersthenics aged 30-49 years.
P-Q is longer in athletes developing the quality of endurance. A number of features concern the teeth of intervals and ECG segments.