5 / 5 ( 1 voice )
The conduction system of the heart is responsible for its main function - contractions. It is represented by several nodes and conductive fibers. The correct functioning of this system ensures normal heart rhythm.
If any disturbances occur, various types of arrhythmias develop. The article presents a system for conducting impulses through the heart. The importance of the conduction system, its state in normal conditions and in pathology are described.
The conduction system is a complex complex of cardiomyocytes
SINUS NODE
The sinus node is a bundle of specific cardiomuscular tissue, the length of which reaches 10-20 mm and width - 3-5 mm. It is located subepicardially in the wall of the right atrium, immediately lateral to the opening of the superior vena cava. The cells of the sinus node are located in a delicate network consisting of collagen and elastic connective tissue. There are two types of sinus node cells - pacemaker or pacemaker (P-cells) and conductor (T-cells). P cells generate electrical excitation impulses, and T cells primarily function as conductors. P cells communicate both with each other and with T cells. The latter, in turn, anastomose with each other and communicate with Purkinje cells located near the sinus node.
In the sinus node itself and next to it there are many nerve fibers of the sympathetic and vagus nerves, and in the subepicardial fatty tissue above the sinus node there are ganglia of the vagus nerve. The fibers to them come mainly from the right vagus nerve. The sinus node is supplied by the sinoatrial artery. This is a relatively large vessel that passes through the center of the sinus node and small branches extend from it to the tissue of the node. In 60% of cases, the sinoatrial artery arises from the right coronary artery, and in 40% from the left.
The sinus node is the normal electrical pacemaker of the heart. At regular intervals, electrical potentials arise in it, exciting the myocardium and causing contraction of the entire heart. P cells of the sinus node generate electrical impulses that are carried by T cells to nearby Purkinje cells. The latter, in turn, activate the working myocardium of the right atrium. In addition, along specific pathways, the electrical impulse is conducted to the left atrium and the atrioventricular node.
Electrical activity of myocardial cells
Under natural conditions, myocardial cells are in a state of rhythmic activity (excitation), so we can only talk about their resting potential conditionally. In most cells it is about 90 mV and is determined almost entirely by the concentration gradient of K+ ions.
Action potentials (AP), recorded in different parts of the heart using intracellular microelectrodes, differ significantly in shape, amplitude and duration (Fig. 7.3, A). In Fig. 7.3, B schematically shows the PD of a single cell of the ventricular myocardium. For this potential to occur, it was necessary to depolarize the membrane by 30 mV. The following phases are distinguished in AP: rapid initial depolarization - phase 1; slow repolarization, the so-called plateau - phase 2; rapid repolarization - phase 3; resting phase - phase 4.
Phase 1 in the cells of the atrial myocardium, cardiac conductive myocytes (Purkinje fibers) and ventricular myocardium has the same nature as the ascending phase of the action potential of nerve and skeletal muscle fibers - it is caused by an increase in sodium permeability, i.e. activation of fast sodium channels of the cell membrane. During the AP peak, the sign of the membrane potential changes (from -90 to +30 mV).
Membrane depolarization causes activation of slow sodium-calcium channels. The flow of Ca2+ ions into the cell through these channels leads to the development of an AP plateau (phase 2). During the plateau period, sodium channels are inactivated and the cell enters a state of absolute refractoriness. At the same time, potassium channels are activated. The flow of K+ ions leaving the cell provides rapid repolarization of the membrane (phase 3), during which calcium channels close, which accelerates the repolarization process (since the incoming calcium current, which depolarizes the membrane, decreases).
Membrane repolarization causes gradual closure of potassium channels and reactivation of sodium channels. As a result, the excitability of the myocardial cell is restored - this is a period of so-called relative refractoriness.
In the cells of the working myocardium (atria, ventricles), the membrane potential (in the intervals between successive APs) is maintained at a more or less constant level. However, in the cells of the sinoatrial node, which acts as the pacemaker of the heart, spontaneous diastolic depolarization (phase 4) is observed, upon reaching a critical level of which (approximately -50 mV) a new AP arises (see Fig. 7.3, B). The autorhythmic activity of these cardiac cells is based on this mechanism. The biological activity of these cells has other important features: 1) low slope of AP rise; 2) slow repolarization (phase 2), smoothly transitioning into the fast repolarization phase (phase 3), during which the membrane potential reaches a level of -60 mV (instead of -90 mV in the working myocardium), after which the slow diastolic depolarization phase begins again. The electrical activity of the cells of the atrioventricular node has similar features, however, the rate of spontaneous diastolic depolarization is much lower than that of the cells of the sinoatrial node, and accordingly the rhythm of their potential automatic activity is less.
The ionic mechanisms of generation of electrical potentials in pacemaker cells have not been fully deciphered. It has been established that calcium channels play a leading role in the development of slow diastolic depolarization and the slow ascending phase of AP in the cells of the sinoatrial node. They are permeable not only to Ca2+ ions, but also to Na+ ions. Fast sodium channels do not participate in the generation of APs in these cells.
The rate of development of slow diastolic depolarization is regulated by the autonomic (autonomic) nervous system. In the case of the influence of the sympathetic part, the transmitter norepinephrine activates slow calcium channels, as a result of which the rate of diastolic depolarization increases and the rhythm of spontaneous activity increases. In the case of the influence of the parasympathetic part, the ACh transmitter increases the potassium permeability of the membrane, which slows down the development of diastolic depolarization or stops it, and also hyperpolarizes the membrane. For this reason, the rhythm slows down or the automaticity stops.
The ability of myocardial cells to be in a state of continuous rhythmic activity throughout a person’s life is ensured by the effective operation of the ion pumps of these cells. During diastole, Na+ ions are removed from the cell, and K+ ions return to the cell. Ca2+ ions that penetrate the cytoplasm are absorbed by the endoplasmic reticulum. Deterioration of blood supply to the myocardium (ischemia) leads to depletion of ATP and creatine phosphate reserves in myocardial cells; the operation of the pumps is disrupted, as a result of which the electrical and mechanical activity of myocardial cells decreases.
INTERNODE PATHWAYS
Electrophysiological and anatomical studies in the last decade have proven the presence of three specialized pathways in the atria connecting the sinus node with the atrioventricular node: the anterior, middle and posterior internodal tracts (James, Takayasu, Merideth and Titus). These pathways are formed by Purkinje cells and cells very similar to the cells of the contractile atrial myocardium, nerve cells and ganglia of the vagus nerve (James).
The anterior internodal tract is divided into two branches - the first of them goes to the left atrium and is called the Bachmann bundle, and the second goes down and anteriorly along the interatrial septum and reaches the upper part of the atrioventricular node.
The middle internodal tract , known as Wenckebach's bundle, starts from the sinus node, passes behind the superior vena cava, descends down the posterior part of the interatrial septum and, anastomosing with the fibers of the anterior internodal tract, reaches the atrioventricular node.
The posterior internodal tract , called the bundle of Thorel, arises from the sinus node, passes downward and posteriorly, passes directly above the coronary sinus and reaches the posterior part of the atrioventricular node. Thorel's bundle is the longest of all three internodal paths.
All three internodal tracts anastomose with each other near the upper part of the atrioventricular node and communicate with it. In some cases, fibers depart from the anastomosis of the internodal tracts that bypass the atrioventricular node and immediately reach its lower part, or reach the place where it passes into the initial part of the His bundle.
Anatomy
The PSS consists of two interconnected parts: sinoatrial (sinoatrial) and atrioventricular (atrioventricular).
node is classified as sinoatrial
(
Kisa-Flyaka node
), three internodal fast conduction bundles connecting the sinoatrial node with
the atrioventricular
and interatrial fast conduction bundle connecting the sinoatrial node with the left atrium.
The atrioventricular part consists of the atrioventricular node
(
Aschoff-Tawar node
),
His bundle
(includes a common trunk and three branches: left anterior, left posterior and right) and
Purkinje fibers.
ATRIOVENTRICULAR NODE
The atrioventricular node is located to the right of the interatrial septum above the insertion of the tricuspid valve leaflet, directly adjacent to the orifice of the coronary sinus. Its shape and size are different: on average, its length reaches 5-6 mm, and its width - 2-3 mm.
Like the sinus node, the atrioventricular node also contains two types of cells - P and T. However, there are significant anatomical differences between the sinoauricular and atrioventricular nodes. The atrioventricular node has much fewer β cells and a small amount of collagen connective tissue network. It does not have a permanent, centrally running artery. In the fatty tissue behind the atrioventricular node, near the mouth of the coronary sinus, there are a large number of fibers and ganglia of the vagus nerve. The blood supply to the atrioventricular node occurs through the ramus septi fibrosi, also called the artery of the atrioventricular node. In 90% of cases it arises from the right coronary artery, and in 10% from the ramus circumflexus of the left coronary artery.
The cells of the atrioventricular node are connected by anastomoses and form a mesh structure. In the lower part of the node, before the transition to the His bundle, its cells are located parallel to each other.
BUNCH OF GIS
The bundle of His, also called the atrioventricular bundle, begins directly at the lower part of the atrioventricular node, and there is no clear boundary between them. The bundle of His runs along the right side of the connective tissue ring between the atria and ventricles, called the central fibrous body. This part is known as the initial proximal or penetrating part of the bundle of His. Then the bundle of His passes into the posterior-inferior edge of the membranous part of the interventricular septum and reaches its muscular part. This is the so-called membranous part of the His bundle. The His bundle consists of Purkinje cells arranged in parallel rows with minor anastomoses between them, covered with a membrane of collagen tissue. The His bundle is located very close to the posterior non-coronary cusp of the aortic valve. Its length is about 20 cm. The His bundle is supplied by the artery of the atrioventricular node.
Sometimes short fibers extend from the distal part of the bundle of His and the initial part of its left leg, going into the muscular part of the interventricular septum. These fibers are called paraspecific Mahaim fibers.
Nerve fibers of the vagus nerve reach the His bundle, but there are no ganglia of this nerve in it.
RIGHT AND LEFT BAND BAND
The bundle of His in the lower part, called the bifurcation, is divided into two legs - right and left, which run subendocardially or intracardially along the corresponding side of the interventricular septum. The right crus is a long, thin, well-segmented fascicle consisting of many fibers with little or no proximal branching. In the distal part, the right bundle branch leaves the interventricular septum and reaches the anterior papillary muscle of the right ventricle, where it branches and anastomoses with the fibers of the Purkinje network.
Despite intensified morphological studies carried out in recent years, the structure of the left bundle branch remains unclear. There are two main schemes for the structure of the left bundle branch. According to the first scheme (Rosenbaum et al.), the left leg is, from the very beginning, divided into two branches - anterior and posterior. The anterior branch, which is relatively longer and thinner, reaches the base of the anterior papillary muscle and branches in the anterosuperior part of the left ventricle. The posterior branch is relatively short and thick and reaches the base of the posterior papillary muscle of the left ventricle. Thus, the intraventricular conduction system is represented by three pathways, named by Rosenbaum et al. fascicles - the right leg, the anterior branch and the posterior branch of the left bundle branch. Many electrophysiological studies support the idea of a three-bundle (trifascicular) intraventricular conduction system.
According to the second scheme (James et al.), it is believed that, unlike the right leg, the left one does not represent a separate bundle. The left leg at the very beginning, moving away from the His bundle, is divided into many fibers varying in number and thickness, which fan-shapedly branch subendocardially along the left side of the interventricular septum. Two of the many branches form more separate bundles - one located anteriorly in the direction of the anterior muscle, and the other posteriorly in the direction of the posterior papillary muscle.
Both the left and right bundle branches, like the internodal tracts of the atria, are composed of two types of cells - Purkinje cells and cells very similar to the cells of the contractile myocardium. Most of the right and anterior two-thirds of the left leg are supplied by the septal branches of the left anterior descending artery. The posterior third of the left leg is fed by the septal branches of the posterior descending artery. There are many transseptal anastomoses between the septal branches of the anterior descending coronary artery and the branches of the posterior descending coronary artery (James). The fibers of the vagus nerve reach both branches of the His bundle, but there are no ganglia of this nerve in the ventricular pathways.
How to determine
To identify cardiac conduction disorders, instrumental diagnostic methods and functional tests are used. It is possible to diagnose disorders even in the fetus.
Table. Methods for determining cardiac conduction:
| Method | Characteristic |
| Cardiotocography | This is a method that allows you to evaluate the function of the fetal heart. How is CTG performed? An ultrasonic sensor is used that records the heart rate. At the same time, the tone of the uterus is recorded |
| Electrocardiography | The main method that records any changes in cardiac conductivity is an ECG. The method is based on recording the electrical potentials of the heart with a special apparatus, then recording them graphically |
| Ultrasound of the heart | Allows to identify changes in the main parts of the conduction system of the heart, organic lesions of the myocardium |
| Transesophageal electrophysiological study | Study of cardiac contractility when exposed to physiological doses of current. How is cardiac TEE performed? To do this, pass the electrode along the esophagus so that its end is opposite the left ventricle. Then an electric current is applied and the myocardial response to stimulation is recorded. |
Based on the data obtained, a diagnosis is established and treatment tactics are determined.
Diagnosis is carried out using electrocardiography and other methods
The conduction system of the heart is a complex of specialized cardiomyocytes that ensure consistent and coordinated contraction of the myocardium. In the presence of organic diseases or when exposed to external causes, the physiology of contractions is disrupted and arrhythmias occur. Diagnosis is carried out using instrumental methods. Treatment depends on the type of arrhythmia.
FIBER NETWORK PURKINJE
The terminal branches of the right and left bundle branches are connected by anastomoses with an extensive network of Purkinje cells located subendocardially in both ventricles. Purkinje cells are modified myocardial cells that directly communicate with the contractile myocardium of the ventricles. The electrical impulse arriving along the intraventricular pathways reaches the cells of the Purkinje network and from here passes directly to the contractile cells of the ventricles, causing myocardial contraction.
The nerve fibers of the vagus nerve do not reach the network of Purkinje fibers in the ventricles. The cells of the Purkinje fiber network are fed with blood from the capillary network of the arteries of the corresponding region of the myocardium.
Possible violations
Under the influence of external and internal causes, various disturbances can occur in the conduction system. More often they are caused by organic lesions of the myocardium or by abnormalities of the conduction pathways of the heart.
Impulse conduction disorders are of two types:
- with acceleration of implementation;
- with slower conduction.
In the first case, various tachyarrhythmias develop, in the second - bradyarrhythmias and blockades.
Atrial conduction disorders
In this case, the sinoatrial node and interatrial/internodal bundles are affected.
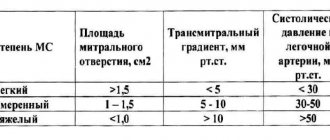
Table. Atrial conduction disorders:
| Form | Characteristic | Treatment instructions |
| Atrial tachycardia | Not considered a disease. There is an increase in the frequency of contractions up to 100 per minute. Usually caused by non-cardiac reasons - fear, tension, pain, fever | Does not require specific treatment |
| Sick sinus syndrome | Reduced ability of self-propelled guns to generate impulses. Causes atrial tachycardia, atrial fibrillation | Treatment is with antiarrhythmic drugs or insertion of a pacemaker |
| Sinoatrial blockade | Slowing down or completely stopping the conduction of impulses from the SAU to the atria. There are three degrees of severity. The third degree is represented by a complete cessation of the SAU function, resulting in asystole or the pacemaker function transfers to the AV node. Causes include dehydration, drug overdose | Treatment is symptomatic; in severe cases, installation of an artificial pacemaker is recommended. |
| Atrial fibrillation | Irregular contraction of individual sections of the atrial myocardium, reaching a frequency of 350-400 per minute. It can be paroxysmal or constant. More often develops against the background of organic heart diseases | Treatment is with antiarrhythmic drugs |
| Atrial flutter | Regular contraction of the atria with a frequency of 250-350 per minute. It can also be paroxysmal or constant, develops against the background of organic myocardial lesions | Treatment is with antiarrhythmic drugs |
Atrial conduction disorders occur less frequently and are milder than intraventricular conduction disorders.
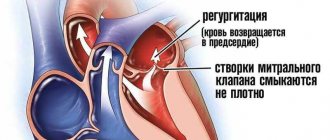
AV block
AV conduction is the process of transmitting impulses from the AC to the ventricles of the heart through the AV node. When impulse transmission slows down or completely stops, AV blockade develops.
There are three degrees of this condition:
- Prolongation of the PQ interval by more than 0.2 s. Observed with dehydration, overdose of cardiac glycosides. It is not clinically manifested.
- This degree is divided into 2 types - Mobitz 1 and Mobitz 2. In the first case, there is a gradual lengthening of the PQ interval until the ventricular complex falls out. In the second case, the ventricular complex disappears without previous prolongation of the PQ interval. The causes of second degree AV block are organic heart lesions.
- In the third degree, the impulse from the self-propelled gun is not carried out to the ventricles. They contract in their own rhythm under the influence of impulses from Purkinje fibers. The clinical picture is represented by frequent dizziness and fainting.
Treatment for the first degree is not required; for the second and third, a pacemaker is installed.
Violation of intraventricular conduction
As a result of slowing down the conduction of the impulse along the His bundle, a complete or incomplete blockade of its legs occurs. Incomplete blockade is not clinically manifested; there are transient changes on the ECG. Complete blockade is more common on the right leg than on the left. It can occur against the background of complete health, or in the presence of organic heart damage.
If ventricular conduction is disturbed in the direction of acceleration, tachyarrhythmias occur.
Table. Types of ventricular tachyarrhythmias:
| Form | Characteristic | Treatment |
| Paroxysmal tachycardia | Ventricular contractions increase to 140-200 per minute. Occurs against the background of organic myocardial lesions. Manifested by dizziness, attacks of loss of consciousness | Specific treatment |
| Ventricular fibrillation | The frequency of contractions of the ventricular myocardium is up to 280 per minute | Reanimation |
| Ventricular flutter | Chaotic rhythm, then circulatory arrest | Reanimation |
If intraventricular conduction is impaired, a worse prognosis is observed than if conduction through the atria is impaired.