High blood pressure before and after childbirth is a common problem that women have to face. Often this negative consequence of pregnancy affects women who have a history of diabetes. However, there are cases when those who are in excellent health are faced with symptoms of hypertension. It is possible to answer the question of why blood pressure rises before childbirth and stays this way for a long time only after a detailed examination, since there are many reasons why a woman has high blood pressure after childbirth, and they require different treatments.
Symptoms
The main symptom is a paroxysmal headache of varying intensity. There is dizziness and darkening of the eyes. Jumps in blood pressure are accompanied by nausea, decreased vision, and fainting. The load on the heart is also great: when blood pressure rises, shortness of breath occurs, darkening of the eyes occurs, and the rhythm increases.
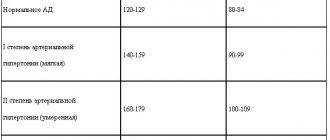
High blood pressure is diagnosed when the blood pressure monitor reads 140/90. If a woman has not previously complained of hypertension, then the presence of symptoms provides grounds for making a diagnosis.
Headache is the main symptom of high blood pressure
Dangers
High blood pressure poses a serious threat to the health of both mother and baby.
Hypertension is an increased tension in the intra-arterial blood flow, which provokes an increased load on the myocardium. After severe exhaustion during the period of bearing a child, the female body requires complete recovery. With increased blood pressure, the general condition of the female body does not improve or recover, but becomes even worse. This phenomenon contributes to the development of severe diseases of internal organs and systems, and loss of vision is also possible.
If measures are not taken in time to restore normal pressure, serious complications may develop in the body. Prominent among them are:
- severe headache that cannot be tolerated. This phenomenon requires drug treatment, which affects the quality of breast milk and can harm the baby.
- loss of consciousness. High blood pressure in women in labor is provoked by a strong load on the heart, which can provoke partial or complete loss of consciousness.
- pulmonary edema.
High pressure in the systemic circulation causes a malfunction of the pulmonary circulation, which leads to the lungs to saturate the blood with oxygen. Increased pulmonary pressure can cause pulmonary edema.
In unproblematic conditions, breastfeeding is the only source of nutrients for the baby. If the mother suffers from hypertension, this affects the quality of breast milk. Violation of blood pressure does not allow the mammary glands to be supplied with the required amount of blood, which leads to inadequate filling of milk with the required substances. This situation does not allow the baby to eat normally.
Main reasons
Women usually report low blood pressure after childbirth, and this is due to the fact that bearing a child and childbirth are energy-intensive processes. The body, which spends energy on maintaining the fetus in optimal conditions, simply cannot cope with normalizing the mother’s condition. As a result, low blood pressure occurs. However, in some cases, the pressure, on the contrary, increases, especially in the later stages (after 20 weeks), and jumps.
If there was no history of the disease initially, then the increase in blood pressure may be due to a number of reasons:
- excess body weight;
- hereditary factors;
- stressful situations;
- drinking alcohol, drugs and smoking;
- hormonal imbalance;
- vegetative-vascular dystonia;
- kidney diseases (chronic and acute);
- thyroid diseases;
- vascular and heart diseases;
- taking certain medications.
High blood pressure after childbirth, as can be seen from the list, can occur for a number of reasons. All of them require different types of therapy.
How to lower blood pressure without medications
To lower blood pressure after childbirth, it is necessary to follow generally accepted recommendations for successful recovery of the body. These rules will help not only lower blood pressure, but also strengthen the general condition of the female body.
- Normalization of the nervous system. To do this, you need to rest more and experience good emotions. Rest includes a good night's sleep and doing what you love (hobbies). To relieve severe stress due to caring for the baby, the child’s father and relatives should be invited to help. And devote the free time to walking in the fresh air.
- Smoking and drinking alcohol are absolutely prohibited.
- You should not overeat. It is better to stick to frequent meals in small portions.
- It is necessary to rationalize the menu, exclude foods that cause high blood pressure after childbirth. You should avoid fried, fatty, very spicy and salty foods, sweet flour products, smoked foods and spices, carbonated water and coffee. To normalize blood pressure, you can increase the amount of fresh fruits and vegetables, oatmeal or buckwheat porridge in your diet, that is, enrich the menu with foods high in potassium, magnesium and vitamin C.
- You need to consume 2-3 liters. liquids per day to fully establish the drinking regime.
- You should avoid strenuous physical activity aimed at losing weight after childbirth. Such restoration of the figure can have an impact on the general condition of the body.
- Doctors recommend avoiding possible rushes of blood to the head. This happens when bending sharply. Therefore, even when changing shoes, it is better to ask loved ones for help.
- You should monitor your breathing. Inhalations and exhalations should be short.
To quickly get rid of hypertensive manifestations, the procedure for warming the limbs, which can be done at home, works well. To do this, you should put a heating pad on your shins, and take warm baths with mustard powder for your hands and feet.
It is important to understand that the condition of the baby depends on the health of the mother. Therefore, at the slightest unpleasant symptoms that can be caused by hypertension or concomitant diseases, you should contact a specialized physician to prescribe treatment.
Self-medication can cause negative complications in the postpartum period and harm the newborn.
The danger of hypertension before childbirth
High blood pressure before childbirth is a signal that a pregnant woman is developing gestosis, a type of toxicosis that causes swelling and an increase in the level of protein in the urine. These factors affect the fetus - oxygen starvation occurs.
High blood pressure provokes premature birth, as placental abruption occurs. If a threat to the fetus is identified, the woman is placed in preservation, tests are carried out in a timely manner and the risk of complications is identified.
Increased blood pressure during pregnancy is a dangerous sign
Hormonal imbalance
Preparing for pregnancy, the period of bearing a baby, childbirth, breastfeeding and further recovery are difficult for the female body due to constant hormonal “shocks”. An additional factor affecting the functioning of a woman’s own endocrine system is the use of hormonal drugs, which are often prescribed during pregnancy. These changes do not always go smoothly - the imbalance of hormones that occurs during this period can cause edema.
Hormonal levels affect vascular permeability. In particular, thyroid hormones play a major role here, as well as the ratio of sex hormones (estrogen and progesterone) and other body hormones.
Please note that hormonal imbalance may be accompanied by a general decrease in body tone. Women often complain of weakness, drowsiness, weight gain, tired legs, and constipation. The presence of these symptoms in addition to edema suggests that the hormonal levels of the young mother have not yet recovered.
The danger of hypertension after childbirth
The main reason why high blood pressure appeared after childbirth, given that it was not observed before and during pregnancy, is postpartum stress. Nervous and mental disorders cause overstrain, which, during the period of recovery of the woman’s body, provokes surges in blood pressure. There are also the following reasons for increased blood pressure after childbirth:
- the effect of restorative drugs;
- hormonal imbalance.
Self-administration of drugs that lower blood pressure is contraindicated, because the active components of the medication can pass into breast milk. Treatment with antihypertensive drugs is prescribed taking into account the fact that they should not have an effect on the newborn.
Persisting arterial hypertension after childbirth as a component of metabolic syndrome
Search for effective correction methods
Metabolic syndrome is a combination of a number of factors that greatly increases the risk of cardiovascular disease. According to various authors, the prevalence of metabolic syndrome continues to increase and currently ranges from 5 to 20%. The history of the emergence of the concept of “metabolic syndrome” begins in the middle of the 20th century, when in 1947
J. Vague described two types of fat deposition - android and gynoid and suggested that android obesity is more often combined with diabetes mellitus, coronary heart disease and gout. In 1988
G. Reaven identified a symptom complex that included hyperinsulinemia, impaired glucose tolerance, elevated triglycerides, low high-density lipoprotein (HDL) cholesterol and arterial hypertension (HTN), calling it “syndrome X.” At the same time, it was suggested that the disorders united within the framework of the syndrome are related by a single origin - insulin resistance and compensatory hyperinsulinemia. In 1989, J. Kaplan, describing the “deadly quartet,” identified abdominal obesity, along with impaired glucose tolerance, hypertension and hypertriglyceridemia, as an essential component of the syndrome.
Today, the generally accepted term “metabolic syndrome” is widely used throughout the world.
In 2004, the All-Russian Scientific Society of Cardiology (RSC) adopted criteria for diagnosing metabolic syndrome, which correspond to the criteria of the US National Cholesterol Education Program (2001). According to these criteria, the basis for a diagnosis of metabolic syndrome is the presence of three or more of the following five components:
- abdominal obesity - waist circumference (WC) > 102/88 cm (men/women);
- high triglycerides: > 150 mg/dL (1.69 mmol/L);
- low HDL cholesterol: < 39/50 mg/dL (men/women) (1.04/1.29 mmol/L);
- AH > 130 and/or 85 mm Hg. Art.;
- plasma glucose level 110 mg/dL (6.1 mmol/L).
Somewhat different criteria for diagnosing metabolic syndrome have been adopted by WHO (1988) and the International Diabetes Federation (2005).
International Diabetes Federation criteria:
- abdominal obesity and at least two of the following criteria:
- fasting hyperglycemia;
- AG;
- increased triglyceride levels;
- lowering HDL cholesterol.
WHO criteria:
- insulin resistance or hyperglycemia and at least two of the following criteria:
- abdominal obesity;
- AG;
- increased triglyceride levels;
- lowering HDL cholesterol;
- microalbuminuria.
Today, the problem of metabolic syndrome is extremely relevant throughout the world. Despite the large amount of scientific research, metabolic syndrome requires further research to understand who, when and how to treat (R. Kahn et al., 2005).
According to the decision of the International Diabetes Federation Consensus Group, the most relevant aspects of the metabolic syndrome that require further study are:
- etiology of metabolic syndrome;
- the relationship between blood pressure (BP) and other components of the metabolic syndrome;
- the relationship of various combinations of metabolic syndrome components with cardiovascular disease outcomes;
- the impact of correction of metabolic syndrome components on the risk of developing cardiovascular diseases;
- searching for ways to improve the efficiency of identifying high-risk patients with metabolic syndrome in different populations.
Numerous scientific studies in recent years show that the moment of “launch” of metabolic syndrome in women can be the period of pregnancy.
The components of metabolic syndrome during pregnancy have their own distinctive features. Hypertension during pregnancy is closely related to insulin resistance, but it has not yet been definitively determined in which type of hypertension insulin resistance is most pronounced. In a study by A. Caruso and S. Ferrazzani (1999), a clamp test showed that insulin resistance is most pronounced in women with gestational hypertension. And in the groups of patients with gestosis and physiological pregnancy, the results were similar. Another study (R. Kaaje, H. Laivuori, 1999) showed that insulin resistance is most pronounced in preeclampsia.
The question arises, what comes first during pregnancy - insulin resistance or hypertension? It is known that hyperinsulinemia increases the activity of the sympathoadrenal system, leads to an increase in the reabsorption of sodium and water in the proximal tubules of the kidneys, promotes the proliferation of vascular smooth muscle cells, blocks the activity of Na-K-ATPase and Ca-Mg-ATPase, increasing the intracellular content of Na+ and Ca++, increasing the sensitivity of blood vessels to vasoconstrictors. All these factors lead to the development of hypertension.
In addition, hyperinsulinemia is detected early in pregnancy, before the development of gestational hypertension or preeclampsia (M. Serer, CD Naylor, 1995; JR Sowers, RJ Sokol, 1996; GM Joffe, JR Esterlitz, 1998; CG Solomon, JS Carroll, 1999; KE Innes, JH Wimsatt, 2001). Obesity and physical inactivity predispose to the development of hypertension during pregnancy. A high body mass index (BMI) before or at the beginning of pregnancy is associated with an increased risk of developing preeclampsia and gestational hypertension (CG Solomon, SW Graves, 1994; KE Innes, JH Wimsatt, 2001; R. Thadhani, MJ Stampfer, 1999; N. Sattar , P. Clark, 2001; A. Saftlas et al., 2000). Increased physical activity in the first 20 weeks of pregnancy, on the contrary, is associated with a decrease in this risk (S. Marcoux et al., 1989).
Components of the metabolic syndrome play an important role in the development of pregnancy complications, which, in turn, are likely to influence the future prognosis of cardiovascular diseases in both mother and child. Data have accumulated to suggest that women with a history of pregnancy complications (preeclampsia, gestational diabetes, hypertension, etc.) are at risk for further development of cardiovascular pathology and diabetes mellitus, i.e. pregnancy can be considered a stress test, predicting a woman’s health in later life (D. Williams, 2003).
A number of foreign studies have revealed a significant increase in the risk of developing hypertension in women with a history of preeclampsia. Jonsdottir et al analyzed the causes of death of 374 women who had hypertensive complications during pregnancy and found that the mortality rate from cardiovascular diseases in these women was significantly (1.4 times) higher than in the general population. In addition, it was found that mortality from cardiovascular diseases in women with a history of eclampsia and preeclampsia is 1.9 times higher compared to women who had increased blood pressure without proteinuria during pregnancy. VA Rodie et al (2004) found that pregnancy complications, especially preeclampsia and chronic intrauterine fetal malnutrition, increase the subsequent risk of developing cardiovascular disorders in women.
Pouta A. et al (2004) showed that women with preeclampsia have an increased risk of developing insulin resistance after childbirth.
A prospective observation of 3799 nulliparous women from 1989 to 1997 with the formation of 168 case-control pairs and observation during pregnancy and for 7–8 years after childbirth revealed that in the group with hypertension during pregnancy the risk of metabolic syndrome was 3–3. 5 times higher than in the group without hypertension (JC Forest, J. Girouard, 2005).
All of the above indicates that hypertension syndrome during pregnancy can be considered an independent risk factor for cardiovascular diseases and, possibly, a factor in the formation of metabolic disorders. Accordingly, women with hypertension syndrome during pregnancy require close medical supervision not only during pregnancy, but also after childbirth. Unfortunately, very often after childbirth, women, due to their busyness, pay little attention to their health and do not consult a doctor. However, it has now been proven that the earlier treatment for hypertension that persists after childbirth is started, the more favorable the prognosis. Therefore, it is necessary to actively monitor the state of the cardiovascular system after childbirth in women with hypertension syndrome during pregnancy and, if hypertension persists, provide appropriate treatment.
How to treat hypertension that persists after childbirth as part of the metabolic syndrome? When choosing optimal therapy, the effect of the drug on the main components of the metabolic syndrome should be taken into account. Medicines used to treat hypertension can be divided into three groups:
- having a metabolically positive effect (ACE inhibitors, selective α1-blockers, angiotensin II receptor antagonists, imidazoline receptor agonists);
- having a metabolically neutral effect (long-acting calcium antagonists, highly selective β-blockers, thiazide-like diuretics);
- having a metabolically negative effect (non-selective β-blockers, thiazide diuretics).
Of course, when choosing the optimal drug for the correction of hypertension that persists after childbirth, preference should be given to drugs that have a metabolically positive effect.
ACE inhibitors have a proven hypotensive effect and are characterized by a pronounced positive effect on the components of the metabolic syndrome. Metabolic effects of ACE inhibitors:
- decreased insulin resistance and improved glucose metabolism, which is associated with increased formation of bradykinin and improved microcirculation;
- a positive effect on lipid metabolism, manifested by a moderate tendency to reduce the level of cholesterol, triglycerides, and a decrease in the atherogenicity coefficient;
- can contribute to the metabolic provision (through the influence on lactate dehydrogenase and glucose-6-phosphate dehydrogenase) of oxygen transport, activating the processes of synthesis of high-energy compounds in erythrocytes;
- increase urate excretion by the kidneys.
Angiotensin II (AT II) receptor blockers modulate the functioning of the renin-angiotensin-aldosterone system (RAAS) through interaction with angiotensin receptors. Recent studies of endothelial dysfunction in hypertension suggest that the cardiovascular effects of ATII receptor blockers may also be associated with endothelial modulation and effects on nitric oxide production. Specific blockade of AT II receptors allows for a pronounced antihypertensive and organoprotective effect.
Clinical studies show that all angiotensin receptor blockers have a high antihypertensive and pronounced organoprotective effect and are well tolerated. However, the main limitation to the widespread use of drugs in this group is their relatively higher cost compared to ACE inhibitors.
Imidazoline receptor agonists are centrally acting antihypertensive drugs. Differences in the therapeutic and hemodynamic effect of centrally acting drugs are due to unequal affinities for different types of receptors. The first-generation centrally acting drug clonidine has an affinity for two types of receptors: central α-adrenergic receptors and imidazoline receptors. It is assumed that its hypotensive effect is largely due to stimulation of imidazoline receptors, while the main side effects are mediated by cortical α1-adrenergic receptors.
The imidazoline receptor agonists rilmenidine and moxonidine are highly selective for I1 receptors. Their affinity for I1 receptors is more than 100 times greater than their affinity for α2 adrenergic receptors. Both drugs are characterized by a pronounced hypotensive effect, sometimes accompanied by a slight sedative effect. The hypotensive effect of imidazoline receptor agonists and the resulting decrease in peripheral vascular resistance are associated with their pronounced peripheral sympatholytic activity. In this case, stimulation of I1 receptors causes only a slight decrease in heart rate (HR). Central I1 receptors of the hypothalamic region are involved in the regulation of blood glucose levels, as shown in an experiment with the selective I1 receptor agonist agmatine, which causes a decrease in blood glucose levels. Moxonidine has a similar effect. In addition, it is assumed that imidazoline receptors are localized in the pancreas and their activation leads to increased insulin secretion. Experimental studies have shown that the use of moxonidine in Zucker rats (obesity model) caused a decrease in the level of hypothalamic neuropeptide Y, which may be one of the mechanisms explaining the decrease in body weight during therapy with this drug. However, the use of drugs in this group is limited due to the presence of side effects associated with their central action (sedation, influence on the ability to drive vehicles and perform work that requires precise coordination of movements), and the high cost of all representatives of this group.
Selective α-blockers block the action of catecholamines on α-adrenergic receptors, which leads to vasodilation and a decrease in blood pressure. Despite the positive metabolic effects, drugs in this group are rarely used as monotherapy. Apparently this is due to their side effects. Preference for drugs in this group as monotherapy should be given to patients with high total peripheral resistance, dyslipidemia, diabetes mellitus, and prostate hypertrophy.
Thus, according to the literature, of all antihypertensive drugs that have a metabolically positive effect, for women with hypertension that persists after childbirth after breastfeeding, the most promising group is ACE inhibitors due to their proven effectiveness, high degree of safety and relatively low cost (which important due to the need for long-term treatment).
Today in Russia the group of ACE inhibitors is represented by a wide range of drugs. The main ones are presented in the table.
All of these drugs can be used to treat hypertension in women with persistent hypertension after childbirth (after stopping breastfeeding). The choice of a specific drug within a group must be made taking into account its current availability and cost. The duration of treatment is determined individually and depends on the dynamics of blood pressure; most often, long-term treatment is necessary.
Thus, based on the above, the following conclusions can be drawn.
- Pregnancy with hypertension and metabolic disorders is a risk factor for subsequent cardiovascular diseases.
- The information available to date is insufficient to fully understand the extent of the impact of metabolic syndrome that begins during pregnancy on long-term prognosis.
- It is necessary to focus the attention of doctors and patients on the importance of the earliest correction of hemodynamic and metabolic disorders during pregnancy and after childbirth.
A. Yu. Galyautdinova , Candidate of Medical Sciences O. N. Tkacheva , Doctor of Medical Sciences, Professor N. S. Samsonenko, K. Yu. Guseva, R. M. Kotenko MGMSU, Moscow
Hypertension due to endometritis
In some cases, increased blood pressure occurs due to postoperative endometritis. A complication occurs if microbes and viruses enter the uterine cavity during childbirth. The main symptoms, in addition to increased blood pressure, are:
- a sharp increase in temperature up to 39 degrees;
- aching pain in the lower abdomen, in some cases it can be cutting;
- severe tachycardia;
- the appearance of brown purulent discharge;
- sleep problems.
Women who are suspected of having endometritis are re-examined with ultrasound. Antibiotics are prescribed and feeding is stopped during treatment.
Lifestyle
This factor cannot be discounted. Despite the fact that many young mothers look for the reasons for swelling of the legs after childbirth in disruption of the body, nutritional habits and the nature of the load are of great importance. After becoming a mother, many women feel that their pregnancy restrictions are over, especially if they are not breastfeeding. Abuse of fried and salty foods, improper protein intake, and an abundance of sweets in the diet certainly contribute to postpartum edema. On the other hand, some women, dreaming of quickly regaining a slim figure, sharply limit themselves in food. Starvation diets lead to metabolic disorders and fluid accumulation in tissues (so-called “hunger edema”). And finally, after the baby is born, you do not need to stop taking vitamins. After all, edema is caused by a lack of sodium and potassium in the body, which are so easy to obtain by taking vitamin-mineral complexes.
We mentioned not only diet, but also activity level. It's no secret that sometimes a young mother spends the whole day caring for her baby. This leads to her legs swelling even after pregnancy. This is all due to excessive stress and lack of normal blood circulation. During the child's daytime sleep, the mother is also recommended to rest for at least 15-20 minutes, and her legs should be elevated at this time.
Is high blood pressure related to hormonal imbalance due to pregnancy and childbirth?
The female body is rebuilt from the first day of conception; after childbirth, not only the menstrual cycle, but also other functions do not return to normal immediately. However, a hormonal imbalance does not cause an increase in blood pressure or surges if it does not affect the psychosomatic state. Reasons for visiting a doctor after childbirth, in addition to high blood pressure, are:
- unmotivated increase in body weight (if a woman does not limit herself in nutrition, then this factor is not so obvious);
- manifestation of signs of virilization - hair growth begins according to the male type (dark hair on the stomach, face);
- there is spotting discharge not during menstruation;
- sudden surges in blood pressure accompanied by severe headaches;
- constant drowsiness and fatigue.
These symptoms may indicate the presence of hormonal imbalance after childbirth. Hormonal levels will not return to normal on their own; you need to contact a specialist.
An increase in blood pressure cannot be attributed to changes in the body. If symptoms persist for more than a few weeks, you should consult a physician. He will refer you for examination to an endocrinologist, cardiologist and neurologist. Experts will tell you what to do to ensure that the treatment is safe for the woman and her child.
Medicines and breastfeeding
When determining an accurate diagnosis, the doctor prescribes hypotonic medications to the woman, which can negatively affect the quality of milk. But you should not categorically refuse natural breastfeeding. You just need to choose medications that have a low level of effect on breast milk. Such drugs include Dopegit, Dibazol, Verapamil.
"Dopegit" . The hypotensive effect of the drug is expressed in its ability to reduce the frequency of myocardial contractions and minute blood volume. "Dopegit" reduces peripheral blood resistance, which contributes to a rapid decrease in pressure. The maximum effect of the drug after internal administration begins after 4-6 hours and lasts for 1-2 days. The prescription and required dosage are carried out under strict medical supervision. The drug is approved for use by pregnant women and during breastfeeding.
"Dibazol" . The drug has a strong vasodilator effect, which helps lower blood pressure. Dibazol also has an antispasmodic effect, which normalizes vascular tone. The therapeutic effect of the drug begins 30-60 minutes after oral administration and lasts for 2-3 hours. The drug should only be prescribed to pregnant and breastfeeding women by a qualified physician.
"Verapamil" . The drug has a strong hypotonic, antianginal and antiarrhythmic effect. "Verapamil" has a beneficial effect on the functioning of the myocardium, preventing unpleasant symptoms in diseases of the heart and blood vessels. Its use during pregnancy or breastfeeding is permitted only if the expected benefit to the mother outweighs the risk of possible complications for the baby.
It should be taken into account that medications that do not allow blood pressure to increase should be taken so that the moment of feeding does not coincide with the time of the maximum concentration of the drug in the mother’s blood. Antihypertensive medications should be taken immediately before breastfeeding. This will prevent the active substances from entering the bloodstream and harming the baby.
Video on the topic
About the treatment of hypertension during pregnancy and lactation in the video:
Hypertension syndrome after childbirth is a problem that absolutely any woman can face. Most often, this condition can be easily corrected and does not interfere with the continuation of lactation. Young mothers should remember this and never self-medicate. Women who are breastfeeding should only be treated by a doctor who has experience working with such patients.
The information on the MyMedNews.ru website is for reference and general information, collected from publicly available sources and cannot serve as a basis for making a decision on the use of medications in the course of treatment.
MyMedNews.ru
And we also have
Scientists have discovered a connection between memory and the stomach
Causes of swollen legs after childbirth
Swelling in the legs after the birth of a child also appears due to an inactive lifestyle. The new mother usually spends the first 3-7 days in the hospital and spends most of the day in the ward. Due to poor health, bed rest may last even longer. After returning home, it’s also not immediately possible to adjust your schedule. To reduce the likelihood of severe leg swelling after childbirth, follow these recommendations:
- Walk with the stroller for at least half an hour every day. Gradually increase the walking time, taking into account the pediatrician’s recommendations, the weather, the baby’s age and your well-being.
- Eat right. To spend minimal time cooking, use a slow cooker or pressure cooker. Simple and healthy dishes are prepared very quickly. The menu can include: seasonal vegetables and fruits, cereals, steamed meat, cottage cheese, kefir, fish. During pregnancy, you can make preparations in the form of dumplings, cutlets and other dishes that can be frozen. After the baby is born, such a supply of semi-finished products will be very useful.
- Treat your skin with a contrast shower. Temperature changes help relax the legs and help fight severe swelling after childbirth.
- Rest when your baby sleeps. Don't take on all the household chores. A happy mother is a calm mother. Not all babies behave calmly in the first months after birth, so count on your strength and put the need to rest first.
- Wear compression garments after childbirth and avoid putting additional stress on your legs. For walking, choose comfortable shoes without heels and narrow toes. It should not put pressure on the leg so as not to provoke swelling.
- Massage your legs and hold them in a position above your head for 10-15 minutes every evening. This helps improve blood circulation and helps women cope with fluid stagnation in the body.
If you follow all the recommendations, physiological swelling after childbirth will become less pronounced after 7-10 days, and will completely go away within a month. If the problem does not go away, you need to consult a doctor. Swelling can also appear after surgery (cesarean section): during the operation, blood vessels are damaged, due to further compression of which, blood stagnation occurs in the legs.
To comfortably wait out the period when your legs are still swollen, you can wear long sundresses for pregnant and nursing mothers, made from natural materials. The Russian brand Proud Mom suggests wearing them in summer, spring and autumn, combining them with cardigans, jackets and light jackets. They look good with both sneakers and sandals. Choose any shades from our catalog on the website: red, gray, black, purple, pink, blue and others.
Swelling in the legs after childbirth is an unpleasant problem that can be easily dealt with if you understand why it appeared. If lifestyle changes do not help, consult a doctor and do not self-medicate. But most importantly, don’t get upset over trifles. Cheer yourself up with good purchases in the Proud Mom online store - the things you will find on the pages of the catalog can be comfortably worn while breastfeeding your baby.
Useful tips
To lower blood pressure, young mothers can resort to the following tips:
- a good hypotensive effect for high blood pressure is provided by herbal infusions and infusions prepared from hawthorn, ginseng, motherwort and other medicinal plants (before using herbal medicines, you should consult a medical specialist);
- to normalize the condition, a woman after childbirth needs to relax, a light massage can help her with this, in which special attention should be paid to working out acupuncture points (this procedure should be carried out by an experienced specialist);
- Cold compresses on the forehead and applying a hot heating pad to the legs will help reduce pressure (such procedures will increase blood flow to the lower body and lower high blood pressure).