Determination of hemoglobinpresentation for the lesson
Slide 1
Methods for determining hemoglobin concentration
Slide 2
Assessment of hemoglobin content: clinical significance: ↓ Decrease in hemoglobin concentration: anemia (impaired Hb synthesis, blood loss, hemolysis, lack of red blood cell production, etc.)
Slide 3
↑ Increased hemoglobin concentration: polycythemia, hemoconcentration during dehydration, burns, persistent vomiting; exposure to high altitudes, excessive exercise or agitation;
Slide 4
lung diseases leading to decreased pulmonary perfusion and poor lung aeration; chronic chemical exposure to nitrites, sulfonamides, causing the formation of meth- and sulfohemoglobin. ↑ Increase in hemoglobin concentration:
Slide 5
The term “total hemoglobin” applies to the totality of hemoglobin forms that are present in the blood of healthy people or appear in pathology:
Slide 6
hydroxy hemoglobin (HbO 2); reduced hemoglobin (Hb) (synonyms: hemoglobin (H Hb ++), ferrohemoglobin (Hb 4)); carbo hemoglobin (HbCO 2) (CO 2 - carbon dioxide) Normal forms of hemoglobin
Slide 7
carboxy hemoglobin (HbCO) (syn.: carbonmonoxyhemoglobin (HbCO) 4; met hemoglobin (MetHb), synonyms: hemI globin (Hb +++), ferrihemoglobin (Hb 4 +3); sulf hemoglobin (SHb), synonym - verdoglobin S; hemeIglobincyanide (HiCN) (syn.: cyanmethemoglobin (CNMetHb)); etc. Pathological forms of hemoglobin
Slide 8
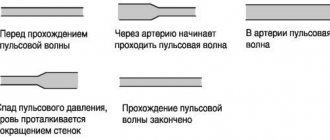
ANALYSIS METHODS Most of all in the blood are: oxyhemoglobin, deoxyhemoglobin, carboxyhemoglobin, methemoglobin. Absorption spectra of oxyhemoglobin (HbO2), deoxyhemoglobin (HbH), methemoglobin (HbMet), carboxyhemoglobin (HbCO)
Slide 9
To determine hemoglobin, hemoglobin derivatives are most often analyzed, formed during its oxidation and the addition of various chemical groups to heme, leading to a change in the valence of iron and the color of the solution.
Slide 10
When quantifying hemoglobin by colorimetric methods, the problem arises in choosing a reagent that would convert all hemoglobin derivatives into only one form before photometric analysis.
Slide 11
The best methods for quantitatively converting hemoglobin into its derivatives turned out to be: hemiglobin cyanide (HbCN), hemichrome (HbChr) and hemiglobinazide (HbN3), which, when photometrically, give the smallest determination error among other methods of analysis.
Slide 12
Hemiglobincyanide method (Drabkin method) (1936) Absorption spectrum of cyanmethemoglobin (CNmetHb) Principle of the method: all forms of hemoglobin are converted to hemiglobincyanide (using a transforming reagent (containing potassium iron cyanide, potassium cyanide and sodium bicarbonate) at a wavelength of 540 nm
Slide 13
Hemohyglobincyanide method (Drabkin method) (1932) A 540 HiCN x 16114.5 x 10 -3 x P Hb (g/l) = =367.7 x A 540 HiCN 11.0 x L A 540 HiCN - absorption of hemoglobin solution at a wavelength of 540 nm, 16114.5 - molecular weight of hemoglobin monomer, 11.0 - millimolar extinction coefficient of cyanmethemoglobin, L - optical path length, equal to 10 mm in most photometers, 10 -3 - conversion of the molar mass of hemoglobin to millimolar mass P - blood dilution (1: 251, ratio of 20 μl of blood and 5.0 ml of transforming solution)
Slide 14
The conversion of hemoglobin to hemiglobin cyanide is carried out by its interaction with a transforming solution containing potassium ferricyanide, potassium cyanide, potassium dihydrogen phosphate and nonionic detergent: The detergent enhances the hemolysis of red blood cells and prevents turbidity associated with plasma proteins. Potassium dihydrogen phosphate maintains a pH level at which the reaction takes place in 3-5 minutes.
Slide 15
Potassium ferricyanide oxidizes all forms of hemoglobin into methemoglobin, which forms, with potassium cyanide, hemeIglobincyanide, which has a reddish color, the color intensity of which is directly proportional to the concentration of hemoglobin in the sample. Oxy hemoglobin Deoxy hemoglobin Carboxy hemoglobin Met hemoglobin
Slide 16
Characteristics of the method The hemiglobincyanide method, developed in 1936 by Drabkin, was approved by the International Committee for Standardization in Hematology (ICSH) in 1963. The main advantage of the hemiglobincyanide method is that HbCN (hemiglobincyanide) is a stable derivative of hemoglobin, and all forms present in the blood hemoglobin can be quickly and quantitatively converted into HbCN; The method provides the ability to obtain results with an error NOT exceeding ± 2%.
Slide 17
Safety requirements when working with a solution containing cyanide compounds Despite all the positive parameters of the hemiglobin cyanide method, its big drawback is that it is based on the use of poisonous cyanide compounds;
Slide 18
Instead of potassium cyanide, many use masked cyanide - acetone cyanohydrin, which, during the preparation of the transforming solution, decomposes to form cyanide ion. The nature of the action of acetone cyanohydrin on humans is similar to the action of hydrocyanic acid, but the effect develops more slowly. Acetone cyanohydrin is absorbed through the skin and can cause severe poisoning. Its maximum permissible concentration (MPC) is 0.9 mg/m3, hazard class 2.
Slide 20
Optical design
Slide 21
Dependence of the readings of the MiniGem-540 hemoglobinometer on the time of incubation of blood samples with the transforming solution. The graph shows that only 15 minutes from the start of the lysis reaction, the readings of the device begin to stabilize and then do not change over the next 2 hours. Therefore, hemoglobin measurement should be carried out no earlier than 20 minutes after adding blood to a test tube with a transforming solution, when all the hemoglobin present in the test tube is converted into the final reaction product - cyanmethemoglobin.
Slide 22
Hemichrome method The principle of the hemichrome method is based on the conversion of all forms of hemoglobin into one - hemichrome. The color intensity is directly proportional to the hemoglobin concentration in the sample. Hemoglobin Hemi-chrome Transform. solution: Fatty acids + Ferricyanide K (or Na dodecyl sulfate)
Slide 23
Hemichrome method Absorption spectrum of methemoglobin (HbMet) The maximum of the hemichrome absorption curve is at a wavelength of 533 nm. The typical wavelength closest to 533 nm is 540 nm, at which photometry is carried out taking into account the conversion factor (factor) for 540 nm.
Slide 24
The main advantage of the hemichromic method is that the forms of hemoglobin contained in the blood can be quickly and quantitatively converted into HbChr while the transforming solution is completely harmless
Slide 25
Optical design
Advantages of the hemichromic method for determining hemoglobin
The method for determining Hb using the hemichromic method has many positive aspects:
- two options for donating blood: collecting capillary or venous fluid;
- express diagnostics, which allows you to get results on the day of the test;
- safety for laboratory employees, since the technique does not use toxic reagents that can harm health;
- use of a semi-automatic analyzer, which completely eliminates the risk of medical error at the cell counting stage;
- simplicity of the method, use of cheap reagents that save money for the clinical institution;
- the accuracy of the obtained indicators, thanks to which the attending physician determines the patient’s condition, prescribes additional diagnostic methods and treatment;
- the need to use a small amount of blood for analysis; if the laboratory technician decides that the analysis is unreliable, repeated testing is possible;
- using a small amount of reagents for one test, which allows chemicals to be distributed over many tests;
- the low cost of one reagent, which allows the clinic to purchase many of these chemicals.
Disadvantages of the hemichromic method for determining hemoglobin
The technique has negative aspects, which are taken into account by the doctor when making a diagnosis:
- the possibility of medical error at the stage of blood donation;
- the possibility of incorrect preparation of the reagent, the use of incorrect concentrations for diluting blood;
- inability to examine the shape and size of cells, the photometer determines only their number.
Indications for use of the hemichromic method
The method for calculating the amount of hemoglobin is carried out in laboratories constantly. Various indications are required to prescribe a study.
- Medical examination of a person to determine the state of his health. In this case, the study is carried out once a year.
- Systemic diseases causing a decrease in hemoglobin. These include a lack of vitamins and folic acid, various forms of anemia, and impaired formation of formed elements in the bone marrow.
- Checking the health of a pregnant woman. During pregnancy, indicators may be slightly or sharply reduced. In the first case, therapeutic measures are not required. If the indicator is significantly reduced, drugs are prescribed to help increase it, since hemoglobin deficiency can negatively affect the growth and development of the fetus.
- Checking the amount of hemoglobin during treatment. The doctor adjusts the dosage of medications or replaces them with other medications.
The essence of the hemichromic method for determining hemoglobin
Hemoglobin has many different forms.
To simplify the calculation of its quantity, the pigment is converted into one form - hemichrome (HbChr). It has an intense red color and a wavelength of 540 nm, making it easy to count. Its number reflects the entire concentration of Hb in the test liquid. To convert hemoglobin into hemichrome, it uses transformation reagents:
- quaternary ammonium bases with surfactants;
- fatty acid salts with added EDTA;
- SDS.
New reagents are being produced that do not contain cyanide. They are based on sodium dodecyl sulfate. The best substance is SDS. The pigment transition rate when used is much higher than that of other reagents. It only takes 5 minutes. With the help of reagents, it is possible to use the study as an express method. That is, it is possible to conduct many analyzes in 1 working day. In this case, the patient receives the finished result on the day of donating the biological fluid.
Laboratories often use hemichromic hemoglobin studies using Olvex reagents. It contains sodium lauryl sulfate, which is completely safe for doctors. Its advantage is low cost with high quality and long shelf life.
The material for research is capillary or venous blood. The latter option is used more often, since the research is more reliable. Find out the difference between finger and vein blood tests.
An anticoagulant, for example, EDTA or heparin, is added to the resulting biological fluid. This will prevent a clot from forming.
The research is carried out in several stages.
- A transforming solution is added to the biological fluid in a ratio of 20:5000 µl. The resulting sample is thoroughly mixed. It is possible to use a centrifuge. The liquid must be thoroughly mixed. The reagent acts on the blood for 5 minutes.
- A photometer is used to determine the hemoglobin concentration. This is an optical device that calculates the indicator at a wavelength of 540 nanometers.
- The result obtained using a semi-automatic analyzer is substituted into the formula C = A×f, where C is the hemoglobin concentration; A – data obtained on the photometer; f is a factor individual for each photometer.
The data obtained is recorded on a study form and given to the patient. He can independently compare the result with the norm. But to make a diagnosis you need to see a doctor. He will identify abnormalities and prescribe treatment.
The results obtained are recorded on the study form and can be compared with the norm. It varies by age and gender. The data is described in the table.
| Age | Female gender, g/dl | Male gender, g/dl |
| 1-3 years | 10,5-12,8 | 10,2-12,6 |
| 3-6 years | 10,5-12,9 | 10,3-12,8 |
| 7-13 years | 10,5-13 4 | 10,8-13,2 |
| From 13 years and above | 11,5-15,7 | 14,8-17,4 |
A slight deviation in the indicator does not indicate the onset of the disease. A deviation from the norm to a lesser or greater extent by several units should be verified by repeated testing. If the result is the same, the doctor must identify the cause of the condition and prescribe treatment.