Causes
The causes of an enlarged heart in a child depend on the type of cardiomegaly. It can be primary or secondary. The secondary course of the disease occurs due to:
- severe toxic injuries;
- past infectious diseases that provoked various heart complications;
- respiratory failure of the lungs;
- acute viral infections.
If we are talking about the primary type of enlarged heart in a child, then the reasons for its occurrence are still not fully understood.
What symptoms should not be ignored
The following symptoms may indicate an enlarged heart in a child:
- increased heart rate;
- pallor or bluishness of the skin;
- rapid breathing;
- blueness of the nasolabial triangle;
- weak appetite.
Since the heart rate in children is always higher than in adults, it is impossible to say for sure whether your baby’s heart beats often or not. Only a doctor can determine this. But if the pulse is more than 160 beats per minute, then this is clearly not a good signal.
Breathing with cardiomegaly is not just rapid, but also shallow, uneven in inhalation and exhalation.
Pale skin occurs as a result of poor circulation due to poor functioning of the heart muscle and the organ itself.
Dilated cardiomyopathy
Treatment of patients with DCM is currently a difficult task. Since the cause of the disease cannot be established, pathogenetic therapy of patients should be aimed at correcting CHF; treatment and prevention of arrhythmias; treatment and prevention of thromboembolic complications. Patients with DCM are refractory to treatment with inotropic agents, which do not reduce the clinical manifestations of CHF and contribute to the occurrence of cardiac arrhythmias.
Conservative treatment
Treatment of CHF in patients with DCM is based on certain principles. Limiting physical activity and salt consumption, especially in the presence of edema syndrome. ACE inhibitors are the first choice in the treatment of patients with DCM. Prescribing these drugs (in the absence of contraindications) is advisable at all stages of the disease, even in the absence of pronounced clinical manifestations of CHF. ACE inhibitors can prevent necrosis of cardiomyocytes and the development of cardiac fibrosis; promote the reverse development of hypertrophy, reduce the amount of afterload (intramyocardial tension), reduce the degree of mitral regurgitation, pressure in the left atrium and the secretion of PNUF.
Under the influence of long-term regular use of ACE inhibitors, the quality of life of patients with DCM improves. The use of ACE inhibitors significantly increases the life expectancy of patients with DCM. The effect of ACE inhibitors in this disease is explained by the inhibition of excessive activation of the RAAS, SAS, tissue and neurohormonal systems responsible for the progression of the disease. The use of ACE inhibitors in patients with DCM should be cautious due to the possibility of a hypotensive reaction and orthostatic hypotension. Initial dose of the drug: enalapril 2.5 mg 2 times a day; ramipril 1.25 mg once a day; perindopril 2 mg once a day. If well tolerated, the dose should be increased (20-40 mg/day for enalapril, 10 mg for ramipril, 4 mg for perindopril).
It is advisable to combine β-blockers with ACE inhibitors. β-blockers are especially indicated in patients with persistent sinus tachycardia, as well as in patients with atrial fibrillation. In patients with DCM, beta-blockers are used not only as a means of preventing and treating cardiac arrhythmias and heart rate control, but also as drugs that affect hyperactivated SAS and RAAS. Their effect on these systems is accompanied by improved hemodynamics, a decrease in myocardial ischemia and damage to cardiomyocytes. β-blockers improve the quality of life, prognosis and survival of patients with DCM. Use any b-blockers (metoprolol, bisoprolol, atenolol, carvedilol).
Treatment begins with small doses of drugs, gradually increasing them to the maximum tolerated. In some patients, in the first 2–3 weeks of treatment with beta-blockers, a decrease in EF, SV and some deterioration of the condition may be observed, which is mainly associated with the negative inotropic effect of these drugs. However, in most of these patients, over time, the positive effects of b-adrenergic blockers begin to predominate, due to the stabilization of neurohormonal regulation of blood circulation, restoration of the density of b-adrenergic receptors on the cell membranes of cardiomyocytes and a decrease in the cardiotoxic effect of catecholamines. EF gradually increases and the clinical manifestations of CHF decrease. The use of b-blockers in DCM requires caution, especially in patients with NYHA class III–IV CHF, although in principle they are not contraindicated in cases of severe decompensation.
Diuretics are used in the presence of blood stagnation in the lungs and/or in the systemic circulation. Thiazide, thiazide-like and loop diuretics are used according to the usual regimen. In the presence of severe edematous syndrome, it is advisable to combine the listed diuretics with the prescription of aldosterone antagonists (aldactone, veroshpiron). For the treatment of patients with chronic left ventricular heart failure, nitrates—isosorbide disinrates or isosorbide 5-mononitrate—can be used as an additional drug. The latter are characterized by high bioavailability and predictable action (olicard, imdur). These drugs promote the deposition of blood in the venous bed, reduce the amount of preload and blood stagnation in the lungs.
Cardiac glycosides are indicated for patients with a permanent form of atrial fibrillation. In these cases, the positive effects of cardiac glycosides (decrease in heart rate) are explained not by the positive inotropic effect of these drugs, but by their vagotropic effect, manifested by an increase in the refractory periods of the AV node and a slowdown in the conduction of the electrical impulse along the AV junction. As a result, the tachysystolic form of atrial fibrillation can be converted into a normosystolic one, which improves the processes of LV diastolic filling, reduces pressure in the left atrium and veins of the pulmonary circulation, and helps reduce shortness of breath and other manifestations of blood stagnation in the lungs.
The question of the advisability of using cardiac glycosides in patients with DCM with sinus rhythm and severe LV systolic dysfunction (EF = 25-30%) remains controversial. Monotherapy with cardiac glycosides is ineffective, since in most cases there is no morphological substrate for the action of these inotropic drugs, namely: there is significant and widespread damage to cardiomyocytes, a decrease in the number of myofibrils, disturbances in cellular metabolism and severe cardiac fibrosis. The use of cardiac glycosides in severe patients with severe LV systolic dysfunction and sinus rhythm is possible only in combination with ACE inhibitors, diuretics under the control of electrolytes and ECG monitoring. Long-term use of non-glycoside inotropic agents in patients with DCM and CHF is not recommended, as it significantly increases the mortality of these patients. Short-term use of non-glycoside inotropic drugs (levodopa, dobutamine, milrinone, amrinone) is justified when preparing patients for heart transplantation.
The prescription of antiplatelet agents is indicated for all patients with DCM, since in 30% of cases the course of the disease is complicated by intracardiac thrombosis and the development of thromboembolism. For this purpose, constant intake of acetylsalicylic acid is used at a dose of 0.25–0.3 g per day, and the use of other antiplatelet agents according to regimens (trental, dipyridamole, vasobral, tonacan). In patients with atrial fibrillation, the administration of indirect anticoagulants (warfarin) under the control of coagulogram parameters is indicated. Doses of the drug are selected so that the INR value is 2-3 units. Many experts consider the indication for prescribing indirect anticoagulants to be the identification of intracardiac thrombi in patients with DCM.
Surgery
Heart transplantation is a highly effective treatment for patients with DCM who are refractory to drug therapy. Indications for transplant surgery are: rapid progression of HF in patients with DCM, lack of effect from conservative therapy; the occurrence of life-threatening heart rhythm disturbances; high risk of thromboembolic complications. The latest world data show an improvement in the quality of life after heart transplantation and an increase in patient survival to 79% in 1 year, 74% in 5 years, 72% in 10 years.
A serious problem limiting the widespread use of this treatment method is the high cost of surgery and organizational problems. In recent years, the length of the waiting list for heart transplantation has increased significantly in economically developed countries. Careful patient selection is based on identifying preoperative characteristics that are the best predictors of good outcome.
Dual-chamber electrical stimulation of the heart using an implantable pacemaker of the DDD type in some cases makes it possible to improve intracardiac hemodynamics, increasing the systolic function of the ventricles, and prevent the development of severe complications. Dynamic cardiomyoplasty plays an important role in the treatment of patients with DCM. A muscle flap from the left latissimus dorsi muscle is used and wrapped around the heart. Contractions are synchronized using a pacemaker. This procedure allows to improve the functional status of patients, quality of life, and increase exercise tolerance. The need for hospitalization and medications is reduced. However, the survival rate (70%) does not look very optimistic when mortality in the early perioperative period is excluded. Cardiomyoplasty is most effective in patients with class III CHF. For more severe symptoms, the effect of drug therapy is equal to or more pronounced than the effect of surgery.
In the last decade, the population of patients with DCM has changed significantly. The number of patients with preclinical and subclinical manifestations of the disease has increased. This is due to the widespread introduction of echocardiography into clinical practice, which allows for early diagnosis of the disease. However, many unresolved problems remain regarding the causes, mechanisms of development, early diagnosis and specific treatment of DCM.
Who diagnoses the disease and how
As a rule, pathology is diagnosed randomly. An enlarged heart in a child is usually detected on x-ray. The resulting image clearly shows the increased size of the main vital organ.
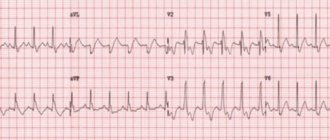
Some changes can also be seen on a cardiogram or echocardiogram. At the same time, the little patients themselves do not experience any unpleasant sensations or discomfort. Such a diagnosis is made against the background of sports activity or other diseases.
If complaints arise and the doctor purposefully orders an X-ray diagnosis of an enlarged heart in a child, then the prognosis is usually unfavorable. This indicates a deterioration of the condition, a severe course of the disease, which in a complicated form can be fatal.
You can perform timely diagnostics at JSC “Medicine”. The clinic is located in the center of Moscow at the address: 2nd Tverskoy-Yamskaya Lane, 10. You can get to it from the metro stations: Mayakovskaya, Belorusskaya, Novoslobodskaya, Tverskaya, Chekhovskaya.
What to do with an enlarged heart?
The first thing that worries parents if an X-ray reveals an enlarged heart in a child is the measures that can be taken.
- First you need to pull yourself together and put aside panic. If the disease is detected by chance, and not by diagnosis based on specific complaints and symptoms, then the baby is clearly not suffering, the organ copes with its task normally.
- It is necessary to contact a cardiologist who will prescribe additional studies and diagnostics to confirm or refute the suspected diagnosis.
- Proceed with the intended treatment. The sooner this happens, the greater the chance of a favorable prognosis.
As for the treatment itself, it is prescribed individually, depending on the symptoms, the baby’s well-being, the severity and cause of the disease.
Diagnostic nuances
Bull heart syndrome is determined using complex diagnostics. It is the combination of several methods and techniques that allows for maximum assessment of the appearance, volume, and function of the heart. The list of studies to make such a diagnosis includes:
- blood analysis;
- chest x-ray;
- electrocardiogram;
- echocardiography;
- CT scan;
- sometimes - a biopsy of the inner surface of the heart ventricles.
All necessary studies are determined by the observing cardiologist. It is based on the severity of symptoms and the person’s condition.
A quieter pulse means you live longer. What should it be like normally? More details