Heart blocks are pathological conditions in which the conduction of nerve impulses inside the heart muscle is disrupted or completely stopped. In a normal heart, electrical impulses occur at a certain frequency in the natural pacemaker, the so-called. sinus node. The impulse originating in the sinus node spreads through the conduction system of the heart, passing through the atria and ventricles. The function of the conduction system is to ensure coordinated work of different parts of the heart, ensuring maximum contraction efficiency.
Causes of heart block
Heart blocks can occur with almost any damage to the heart: coronary heart disease, myocardial infarction, myocarditis, cardiosclerosis, increased stress on the heart
muscle (for example, in athletes or with high blood pressure), as well as in overdose and misuse of certain medications.
Heart blocks can be caused by a hereditary predisposition or a disorder of intrauterine development.
At CELT you can consult a cardiologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
Causes of the disease
There are many known diseases that can cause the development of incomplete and complete blockade of the right bundle branch.
Today it is generally accepted that the condition in question is not hereditary, but a predisposition to cardiac conduction problems can still be transmitted at the genetic level. The following factors can provoke the development of a pathological process inside the ventricles:
- IHD;
- heart defects and tumors;
- myocarditis and endocarditis;
- blockage of one pulmonary artery (PE);
- cardiosclerosis;
- intense enlargement of the myocardium due to chronic hypertension;
- respiratory diseases causing the formation of a “pulmonary” heart;
- myocardial infarction;
- presence of bad habits;
- constant stress.
There are many conditions for the appearance of NBP; they are divided into congenital and acquired. The first type of blockade includes:
- unfinished development of the PNG segment;
- stenosis of the pulmonary artery;
- Lenegra syndrome, which is diagnosed in children if their mother had type II diabetes mellitus during pregnancy;
- Lev's disease.
The extent of damage to the nerve pathways determines the type of blockade:
- Single-bundle - signal transmission along the right branch of the His bundle, one of the branches of the left, is difficult;
- Double-bundle - the branches of the left leg are blocked or the right leg is blocked from one of the branches of the left;
- Three-bundle - all three pathways are involved at once.
10 charming celebrity children who look completely different today Time flies, and one day little celebrities become adults who are no longer recognizable. Pretty boys and girls turn into...
9 Famous Women Who Have Fallen in Love with Women Showing interest in people other than the opposite sex is not unusual. You are unlikely to be able to surprise or shock anyone if you admit it.
Top 10 Broke Stars It turns out that sometimes even the biggest fame ends in failure, as is the case with these celebrities.
How to look younger: the best haircuts for those over 30, 40, 50, 60 Girls in their 20s don’t worry about the shape and length of their hair. It seems that youth is created for experiments with appearance and daring curls. However, already last.
Classification of blockades
Heart blocks are classified either by the area where the signal does not pass, for example, between the atria and ventricles, or by the degree to which conduction within the ventricles is slowed down.
Atrioventricular blockade comes in three degrees:
- 1st degree blockade - impulses, for example, from the atrium to the ventricle are conducted more slowly than normal (impulse delay);
- 2nd degree blockade - only part of the impulses are not carried out;
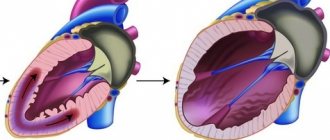
- 3rd degree block - when all impulses from the atria to the ventricles are not carried out, the chambers of the heart contract uncoordinatedly (complete transverse block). The heart rate can drop to 30 per minute and intervals between contractions can reach several seconds and loss of consciousness is possible (Morgagni-Adams-Stokes attacks), which can result in a life-threatening condition.
When the propagation of impulses inside the ventricles slows down, they speak of blockade of the branches or branches of the bundle of His (named after the anatomist who described the nerve bundles of the heart).
All blockades can be transient (appear briefly) or persistent (exist permanently).
Classification
There are several classifications. According to the degree of violation there are:
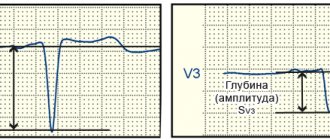
- Incomplete blockade (partial), when the passage of the impulse only slows down, and the QRS complex has a length of 0.10-0.11.
- Complete blockade, when the conduction of the impulse completely stops and the QRS complex expands more than 0.12.
- According to the location of the violation, they are distinguished:
- Monofascicular or single-start, when a conduction disorder is formed in one branch of the His bundle - in the right leg, the left leg of the anterior branch, or the left leg of the posterior branch.
- Bifascicular or bifascicular block, when conduction is disrupted in the left leg, the left leg of the anterior branch and the right leg, or the left leg of the posterior branch and the right leg.
- Trifascicular or three-fascicle blockade, when the disorder occurs in all three branches.
- Local, peri-infarction or focal blockade, when local splitting of the QRS complex occurs. That is, the lesion occurs in some limited area of the left ventricle, in a certain area. As a rule, a lesion forms in the area adjacent to the resulting necrotic area during myocardial infarction. In other words, it arises distal to the main branches of the left and right bundle of His.
- Peripheral intraventricular block is called if the peripheral branches of the legs are involved in the process.
- Proximal, when the lesion is located inside the His bundle.
- Distal blockade is called if the lesion is localized at the level of the branches of the left leg or in the right.
By nature, intraventricular blockades are divided into:
- Permanent, when there is a constant disturbance in the conduction of the impulse.
- Variable or intermittent. You can also find names such as alternating, transitional or latent. All these are names of the same disorder, when the passage of the rhythm slows down, less often stops, for some reason, and then is restored again.
There is also the concept of nonspecific intraventricular blockades or arborization ones, when the electrocardiogram data in any one or several branches does not fit the currently available signs. At the same time, the width of the QRS complex does not change significantly. This picture is observed when the patency of the impulse along the distal (terminal) branches of the legs is impaired. However, with diffuse lesions of the heart muscle, the ventricular complex always expands. They are also distinguished by the degree of damage: first, second, third and fourth degrees. All types of intraventricular blockades can be combined with each other. In clinical cardiology, it is customary to indicate in detail what type of disorder. This further helps in prescribing adequate treatment. Symptoms As a rule, the disease does not have pronounced symptoms, except for general fatigue and tiredness. With transverse incomplete blockades, loss of pulse and/or heart sounds may occur. Patients sometimes complain of a feeling of a sinking heart. In cases of complete transverse blockades, persistent bradycardia occurs with all its clinical manifestations. In these cases, Dahms-Stokes-Morgagni syndrome often occurs. If the transverse complete block is also distal, then the risk of developing angina or heart failure, and sometimes sudden death, increases. Diagnostics Usually one ECG is enough to make a diagnosis. If necessary, the doctor may prescribe an ultrasound of the heart. And for intermittent blockades - Holter ECG monitoring. Causes
- Myocarditis.
- Ischemic myocardial disease (CHD).
- Congenital heart defects.
- Cardiomyopathies.
- COPD
- Aortic stenosis, especially complicated by calcification.
- Heart bruise.
- Hyperkalemia.
- Hypertonic disease.
- Heart operations.
- Neoplasms of the heart.
- Muscular progressive dystrophy.
- Lenegra's disease.
- Syphilitic gumma.
- Lev's disease.
- Overdose of procainamide, quinidine, strophanthin K.
- Acquired defects, especially with rheumatoid lesions, usually cause the formation of a right leg.
- Cor pulmonale also usually causes damage to the right leg.
Treatment Mild bundle branch block usually does not require any treatment. Moreover, it is not amenable to drug therapy. It should only be taken into account when prescribing medications. For proximal blockades, atropine or its analogues are sometimes prescribed, but the effect is short-lived. Therefore, all therapy ultimately comes down to treating the disease that caused the blockade. In other words, to eliminate the cause. In case of Dams-Stokes-Morgagni syndrome or the occurrence of heart failure and/or peripheral circulation, as well as angina, permanent or temporary ventricular stimulation is prescribed. Treatment prognosis and prevention. The prognosis of treatment largely depends on the degree of damage to the myocardial conduction system and the timely administration of adequate treatment for the causative disease. Prevention consists of timely treatment of the disease, which can lead to intraventricular blockades, maintaining a healthy lifestyle and regular professional activities. examinations by a doctor.
consultation with a cardiologist
Treatment
Blockades of individual branches of the cardiac conduction system sometimes do not require special treatment, but may indicate the presence of some kind of heart disease that requires therapy. Some blockages are eliminated by prescribing medications. On the other hand, there are medications that themselves contribute to the occurrence of blockades. Therefore, before “treating” the blockade, it is necessary to clarify whether the patient is taking any medication, or a combination of drugs that affects intracardiac conduction, their dosage and time of administration.
Blockades of the 3rd degree, or complete blockades, as a rule, significantly worsen the patient’s well-being and also affect the prognosis of the disease. In these cases, implantation of an artificial pacemaker (pacemaker) is absolutely necessary.
In the multidisciplinary CELT clinic, a complete examination of the patient is possible to identify and timely treat blockades and, if necessary, implantation of an artificial pacemaker (PAC).
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Clinical picture
Clinical manifestations develop only with complete blockade. In other cases, the heart is able to activate adaptive mechanisms and the person does not feel any abnormalities.
With a heart rate of 40–50 beats, patients complain of dizziness and a tendency to faint.
The degree of brain hypoxia depends on the length of pauses between contractions. With Morgagni-Edams-Stokes syndrome, the pulse rate reaches 25–20 per minute. The patient consistently develops the following symptoms:
- sudden general anxiety;
- severe dizziness;
- loss of consciousness (the patient falls);
- the face first turns red, then a “dead” pallor with cyanosis appears;
- pulse is not detected;
- breathing becomes rare and deep;
- spasms begin with twitching of the facial muscles, then move to the limbs and back muscles;
- pupils dilate;
- urine and feces pass out involuntarily.
A long pause between ventricular contractions necessitates defibrillation.
There are 3 types of attacks:
- in a mild form - the patient does not experience loss of consciousness, symptoms are limited to dizziness, a feeling of “tinnitus”, numbness of the extremities;
- moderate severity - there is loss of consciousness, but there are no convulsions or urination;
- severe - each attack occurs according to the described symptoms, without therapeutic measures it is life-threatening for the patient.
Seizures occur in approximately 25–60% of patients with atrioventricular block. The frequency of repetitions varies individually from one every three years to several dozen per day.
Intraventricular blocks
Previous | Contents | next Intraventricular blockades are caused by partial (more often) or complete (less often) disruption of the conduction of impulses along one or more branches of the His bundle. This leads to a delay in the excitation of the contractile myocardium of the corresponding ventricle or part thereof and disruption of the normal sequence of depolarization and repolarization of the ventricles of the heart, which is reflected in changes in the ECG.
Although the idea of a three-bundle structure of the cardiac conduction system has recently been criticized, this concept continues to be used for practical purposes.
In accordance with it, the following options for intraventricular blockades are distinguished depending on the location:
I. Unilateral blockades:
1) single-bundle, or monofascicular:
a) blockade of the anterosuperior branch of the left bundle branch;
b) blockade of the posteroinferior branch of the left bundle branch;
c) right bundle branch block;
2) two-bundle, or bifascicular - blockade of the left bundle branch.
II. Bilateral blockades:
1) two-bundle, or bifascicular:
a) blockade of the right leg and anterosuperior branch of the left bundle branch;
b) blockade of the right leg and the posteroinferior branch of the left bundle branch.
III. Three-fascicular, or trifascicular. There is an opinion that blockade of the left bundle branch in
the proximal part, i.e., before branching into the legs, is not a true bifascicular block. This question is of mainly academic interest.
Depending on the course, intraventricular blockades can be: a) persistent; b) transient and intermittent, when periods of blockade alternate with periods of unchanged intraventricular conduction; c) alternating, when the ECG shows a blockade of one or the other leg. A number of authors also divide intraventricular blocks into complete and incomplete, which, however, is to some extent arbitrary.
Epidemiology. The frequency of bundle branch blocks among the population averages 1.5-2.4% and increases with age (J. McAnulty et al., 1981, etc.). The most common blockade is the anterosuperior branch of the left leg. It is located in the area of the outflow tract from the left ventricle near the aortic valve annulus and, as a result, is susceptible to increased intraventricular pressure and pathological processes affecting the aortic valve. The second place in frequency is occupied by blockade of the right knife
ki. Unlike other intraventricular blockades, in a significant proportion of cases it is not combined with visible structural cardiac pathology. On the contrary, blockade of the left bundle branch, as a rule, accompanies widespread myocardial damage. Blockade of the posteroinferior branch of the left bundle branch is rare, especially isolated, which is partly due to its location in the area of the left ventricular inflow tract and blood supply simultaneously from the anterior and posterior descending coronary arteries.
Etiology. The causes of intraventricular blocks are basically the same as other conduction disorders. In most cases, they are caused by organic heart diseases - congenital and acquired defects, including calcification of the aortic and mitral valves, acute and chronic forms of ischemic heart disease, arterial hypertension, various cardiomyopathies of known and unknown etiology, endocarditis, heart tumors, as well as idiopathic fibrosis of its conduction. systems characteristic of Lev's and Lenegra's diseases. Potentially reversible causes include iatrogenic factors (class IA and 1C antiarrhythmic drugs), hyperkalemia, hypoxia, acidosis, and cardiac injury. Unlike atrioventricular blocks, the possible etiological factors of intraventricular blockades do not include dysfunction of the autonomic nervous system. In some cases, electrocardiographic signs of such blockade, mainly of the right branch of the His bundle, less often of the anterosuperior branch of the left leg, are observed in the absence of visible causes, both reversible and irreversible, in practically healthy individuals.
Pathogenesis. Impaired conduction along the His bundle branches may be due to their focal organic damage, for example, compression due to edema, necrosis resulting in sclerosis, or changes in excitability, the duration of the refractory period, a decrease in the value of the membrane potential in phase 4 AP and other electrophysiological factors. In this case, the nature of ECG changes does not depend on the mechanism of the blockade and its exact localization in the His bundle branch.
Clinic. There are no symptoms, since intraventricular blockades do not cause changes in heart rate and rhythm.
An objective examination of patients with complete block of the right bundle branch is characterized by pathological splitting of the first and second heart sounds, and with blockade of the left leg - paradoxical splitting of the second sound (P2A2).
Diagnosis and differential diagnosis are based on 12-lead ECG data.
When the anterosuperior branch of the left bundle branch is blocked, ventricular excitation begins with depolarization of the interventricular septum, which occurs downward, to the right and anteriorly. This results in the formation of initial small q
in leads I and aVL and wave
g
in leads II, III and aVF.
The initial q
in leads I and aVL are, however, variable and may be absent, which explains the change in the direction of the initial excitation of the interventricular septum from the right side to the left, as well as diffuse myocardial fibrosis in the septal area.
Next, the excitation covers the ventricles, spreading in a counterclockwise direction, as a result of which the apex of the R
in lead aVL is recorded earlier than in lead
aVR.
Due to the initial direction downward and to the right, the excitation vector of the ventricles is projected onto the positive part of the axis of lead III in the first half of the depolarization period, reaching the positive part of the axis of lead II much later. As a result, wave
g
reaches its apex in lead III earlier than in lead II and the average excitation vector of the ventricles is directed upward and to the left.
The first causes a decrease in the amplitude of the R
and the formation of deep waves 5 in leads V 5 _6, and the second causes a deviation of the electrical axis of the heart to the left in the frontal plane, which is the main electrocardiographic criterion for blockade of the anterosuperior branch of the left bundle branch. The minimum value of angle a, which can serve as a diagnostic sign of this blockade, according to various experts, is in the range from -30 to -60°. Most of them propose using the value as this criterion
angle -45°, which provides an optimal balance of sensitivity and specificity. With angle a values ranging from -30 to -45°, blockade of the anterosuperior branch of the left leg can be diagnosed with sufficient accuracy only if the appearance or disappearance of such a deviation of the electrical axis of the heart is documented during dynamic observation. Due to the numerous connections between both branches of the left bundle branch, when one of them is blocked, the width of the QRS
increases relatively little - no more than 0.025 s.
Therefore, when a graphic of anterosuperior or posteroinferior branch block is detected in combination with wide QRS
, one should look for signs of bifascicular or parietal block.
In general, electrocardiographic diagnosis of blockade of the anterosuperior branch of the left bundle branch is based on the following signs {Fig. 39);
1) deviation of the electrical axis of the heart in the frontal plane to the left by more than -45°;
2) slight - within 0.9-0.11 s - increase in the width of the QRS complex;
3) the presence of a ventricular complex of type qR
with an increase in the internal deviation time > 0.045 s in lead aVL and in most cases also in lead I;
4) the presence of a ventricular complex of the type rS / r < S
in leads II, III and aVF;
5) tip of tooth g
in lead III precedes that in lead II;
6) apex of the R wave,
being the last tooth of the ventricular complex, in lead aVL precedes that in lead aVR;
7) decrease in the amplitude of the R
and an increase in the depth of the
S
in leads V 5-6.
Blockade of the anterosuperior branch of the left bundle branch must be differentiated
with other causes of deviation of the electrical axis of the heart to the left by more than -30° and upward. These include:
a) extensive myocardial infarction of the posterior wall of the left ventricle. Its distinctive features are the Qr-
(Q > g) or
QS
in lead II, per hour
ty cases with ST
and (or) T wave inversion
,
as well as the presence of a pathological
Q
and ST segment elevation
in
lead D according to Neb. These changes in leads II and D persist even when a posterior myocardial infarction is combined with a blockade of the anterosuperior branch of the left bundle branch;
b) Wolff-Parkinson-White syndrome with posteroseptal localization of the accessory atrioventricular tract. This is indicated by a shortening of the P
—
Q
and the presence of a delta wave, and in a significant part of cases also an increase in the width of the
QRS
(> 0.12 s);
c) left ventricular hypertrophy. Diagnosed on the basis of the presence, in addition to a deviation of angle a of more than -30°, voltage criteria for hypertrophy in the precordial leads and changes in the ST
and the
T wave,
characteristic of left ventricular overload (see Part I).
Signs of left ventricular hypertrophy in a patient with blockade of the anterosuperior branch of the left bundle branch, which itself causes an increase in the amplitude of Ry
and Sm, can be:
— Svi + (Rv 5 + Sv 5) > 25 mm (sensitivity 69%, specificity 92%; M. Gerstch et al., 1988);
— Sjjj 4 - maximum sum of the amplitude of the R
and S in one of the chest leads > 30 mm (sensitivity 96%, specificity 87%; M. Gerstch et al., 1988);
d) hyperkalemia. It is also characterized by an increase in the width of the QRS
and tall, pointed
T waves;
e) ECS from the apex of the right ventricle. Easily diagnosed by preceding QRS
stimulator impulses.
When blocking the posteroinferior branch of the left leg, the His bundle, the interventricular septum is first excited upward and to the left, then in the anterolateral region of the left ventricle, which leads to the formation of the initial R
in leads I and aVL and narrow
O
in leads II, III and aVF.
The posteroinferior part of the left ventricle is the last to be excited. The excitation vector is directed downward, posteriorly and to the right, as evidenced by deep S
in leads I and aVL and high terminal R waves
in
leads II, III and aVF.
The electrical axis of the heart is deviated to the right. T
waves are not changed.
Thus, diagnostic electrocardiographic signs
Blockades of the posteroinferior branch of the left bundle branch are:
1) deviation of the electrical axis of the heart to the right by more than +90°, as a result of which Rm > Rn;
2) width of the QRS
within 0 t 09—0.11 s;
3) ventricular complex type qR
with increasing time of internal deviation in leads III and aVF.
Q
wave in these leads is 0.04 s or less;
4) ventricular complex type rS
with deep
S
in leads I and aVL.
Since these changes, reflecting a pronounced deviation of the electrical axis of the heart to the right, are nonspecific, the diagnosis of blockade of the posteroinferior branch of the left bundle branch is made only after excluding other possible causes of such a displacement of the electrical axis of the heart. These include primarily hypertrophy and acute overload of the right ventricle, for example with some heart defects or TEVLA, as well as a vertical anatomical location
hearts in persons of asthenic build and with congenital deformities of the chest.
Blockade of the left bundle branch causes a change in the direction of excitation of the interventricular septum to the opposite direction - from right to left, which leads to the disappearance of the initial Q
in the left chest leads.
Excitation of the left ventricle spreads from the interventricular septum, first to its anterosuperior region, and then successively to the lower and posterolateral walls. This causes the formation of monophasic ventricular complexes - in the form of QS
in leads Vj and
R
- in leads I, aVL and V 6.
Due to the delay in excitation of the left ventricle, the R
in lead V 6 has a widened apex.
Depending on the width of the QRS
There are complete and incomplete blockade of the left bundle branch.
At the same time, an increase in the width of the QRS
to 0.12 s or more does not necessarily indicate a complete block of conduction along this leg, but only indicates that the source of excitation of the entire left ventricle is the right leg. The electrical axis of the heart is either unchanged or deviated to the left within the range from -30 to -90°.
Secondary disturbances of repolarization are very characteristic, caused by a change in the direction of its vector to the opposite, as a result of which the vectors of excitation of the ventricles and their repolarization acquire the opposite orientation. This simulates the picture of ischemic damage to the left ventricle and does not allow us to judge its presence or absence if acute forms of IHD are suspected.
The following diagnostic electrocardiographic criteria
complete blockade of the left bundle branch (Fig. 40):
1) increase in the width of the QRS
(0D2 s);
2) wide, jagged at the apex, which can also have a plateau shape, R
in the absence of Q and 5 waves in leads V 6 (be sure to check the correct position of the electrode!), I and (less often) aVL. Time of internal deviation in lead V6 > 0.06 s;
3) ventricular complex in the form of QS
or
rS
S
wave in lead VI and in the form
of rS
- also in leads V 2, III and aVF;
4) discordant with respect to the main wave of the QRS
changes in the
ST
and
T
in all leads.
In this case, oblique depression of the ST
with a transition to a negative
T
is recorded in leads with a dominant
R
(I, aVL and V 6).
On the contrary, in a lead with a leading S wave,
for example Vj „_2>, an obliquely ascending rise of the
ST segment is determined,
turning into a high-amplitude positive
T
. Incomplete blockade of the left bundle branch is distinguished from complete block only by the smaller width of the QRS
(within 0.10-0.11 s) and weak severity of discordant changes in the
ST
and
T
. In a significant proportion of cases, left bundle branch block is a consequence of myocardial hypertrophy. The presence of left ventricular hypertrophy in the left bundle branch block diagram can be judged by the following signs: RavL - * * mm<
SV 2 > 30 mm; Rv 6 > 40 mm; Sv 2 + Rv 6 > 45 mm. According to A. Kafka et al (1986), their sensitivity is 75% and specificity is 90%.
Great difficulties arise in the electrocardiographic diagnosis of the combination of left bundle branch block with acute myocardial infarction (see Vol. I).
Electrocardiographic changes characteristic of left bundle branch block must be differentiated
with signs of Wolff-Parkinson-White syndrome.
-O is crucial
With right bundle branch block, the initial excitation of the interventricular septum is not changed, which is manifested by the preservation of the initial r wave in lead Vy
and the
q
wave in leads I, aVL and V 5 _6< Since the depolarization vector of the left ventricle determines the position and magnitude of the electromotive force of the heart during most of the period of excitation of the ventricles, after depolarization of the septum, the excitation vector retains its normal direction to the left, downward and somewhat anteriorly or
posteriorly As a result, an S wave is recorded in the right chest leads ,
deeper when the vector is directed posteriorly and low-amplitude when it is directed anteriorly.
Excitation of the right ventricle occurs with a delay after the completion of depolarization of the left ventricle. The vector of its excitation directed to the right and forward causes the formation of the final R
in the right chest leads and a wide and usually shallow
S
in leads V 5 _6. A noticeable deviation of the electrical axis of the heart is not typical for a pure right bundle branch block. If it is present, it is necessary to look for signs of concomitant blockade of the anterosuperior or posteroinferior branch of the left bundle branch or severe hypertrophy of the right ventricle.
Based on the width of the ORS complex,
Blockade of the right leg (as well as blockade of the left leg) is divided into complete and incomplete. In this case, an increase in the duration of the ventricular complex is observed with a significant, although not necessarily complete, disruption of conduction along the right leg, when both ventricles are excited, mainly by impulses propagating along the left bundle branch. Disruption of the depolarization process is accompanied by changes in the sequence of ventricular repolarization, which causes deformation of the limb part of the ventricular complex.
Thus, the following diagnostic electrocardiographic signs
complete blockade of the right bundle branch (Fig. 41):
1) increase in the width of the QRS
( > 0.12 s);
2) ventricular complex in the form of rSR
or
rsR
at
R > r
with increasing time of internal deviation (more than 0.05 s) in lead Vj. In most cases, such changes are also noted in lead V 2 and (less often) also in leads III and aVF;
3) an increase in the width of the S wave, which exceeds the duration of the R wave,
in leads V 6 and I and often also in lead aVL, where the ventricular complex looks like
qRS;
4) discordant with respect to the main wave of the QRS
changes in the
ST
and
T
. They are most pronounced in leads V 1 _2rAe; depression of the
ST
and negativity of the T wave
QRS complex as with its complete blockade
primarily in lead Vp when the duration of this complex is in the range of 0.08-0.11 s.
Discordant changes in the ST
and
T
are weakly expressed and may even be absent.
Right bundle branch block is the most common manifestation of aberrant intraventricular conduction caused by transient functional changes in the electrophysiological properties of various parts of the ventricular conduction system in response to prolongation of the preceding cardiac cycle. It represents a physiological reaction, while the appearance of a leg block when the heart rate increases above a certain value (the so-called leg block, depending on the heart rate) is inherent in organic heart diseases.
It is almost impossible to differentiate right leg block from moderate hypertrophy of the right ventricle with its diastolic overload, for example, with an atrial septal defect, using an ECG. This pathology is often combined, since dilatation of the right ventricle causes stretching of the right bundle branch, which leads to its block. Differential diagnosis
with Wolff-Parkinson-White syndrome with localization of accessory pathways in the area of the free wall of the left ventricle or the posterior part of the interventricular septum is based on identifying a shortening of the
P
-O interval and delta waves.
QRS
complex in the form of rSR in leads U1-2, as a normal variant, differs from incomplete blockade of the right bundle branch by the greater amplitude of the initial r wave compared to that of the r wave.
Electrocardiographic signs of bilateral two fascicular blocks consist of changes characteristic of the blockade of each fascicle separately. In this case, the direction of excitation of the ventricles in the first 0.08 s determines the position of the electrical axis of the heart and the schedule of blockade of one of the branches of the left bundle branch. Delay in right ventricular depolarization spreading
from left to right and from back to front, the vector of which is not counteracted by the excitation vector of the left ventricle, causes changes in the terminal part of the QRS complex characteristic of right bundle branch block .
Diagnosis
blockade of the right bundle branch and the anterosuperior branch of the left bundle is based on the following most characteristic electrocardiographic signs:
1) deviation of the electrical axis of the heart to the left in the range from -40...-45° to -120°;
2) increase in the duration of the QRS
(>0.12 s);
3) ventricular complex in the form of rSR
in lead
Ut2)
with oblique depression of the
ST
and negative G waves;
4) ventricular complex in the form of rS
with deep teeth 5 in leads I, III, aVF.
Electrocardiographic diagnosis
blockade of the right leg and the posteroinferior branch of the left bundle branch is reliable only in the absence of clinical indications of the possibility of right ventricular hypertrophy.
It is installed based on the following
1) deviation of the electrical axis of the heart to the right by more than +90°;
2) increase in the width of the QRS
(> 0D2 s);
3) changes in the ventricular complex in leads Up, characteristic of right bundle branch block,
4) ventricular complex in the form of rS
with deep
S waves (S > r)
in leads I and aVL.
Most experts refer to double-bundle block and blockade of the left bundle branch (the so-called unilateral double-bundle block). In cases where the conduction disturbance is localized proximal to its branching, the validity of this statement is controversial.
Three-fascicle block with atrioventricular conduction 1:1 is characterized by alternating complete blockade of the right and left bundle branches or persistent complete blockade of the right leg with alternating blockade of the anterosuperior and posteroinferior branches of the left leg. Combination of bilateral two-fascicle blockade with prolongation of the P
—
O
can be a manifestation of three-fascicle blockade only if
it is due to the prolongation of the interval I
— V on intracardiac ECG. At the same time, the severity of the conduction disturbance in both branches of the His bundle is different. The three-bundle block also includes complete sub-stem atrioventricular block.
Increasing the duration of the QRS
(> 0.11 s) with changes in its graphics that do not fit into the typical picture of right or left bundle branch block is called nonspecific intraventricular block.
An example is blockade of the left bundle branch with a sharp deviation of the electrical axis of the heart to the left. The preservation of normal Q
makes it possible to interpret such changes on the ECG as a blockade of the anterosuperior branch of the left bundle branch at the level of its distal parts.
The term parietal, or arborization, blockade, or local disturbance of intraventricular conduction refers to jaggedness of the QRS complex,
R
wave in one or more ECG leads with its unchanged duration and the absence of graphic changes characteristic of a single-bundle blockade.
It is believed that these changes are associated with a slowdown in conduction in a limited area of the myocardium, not necessarily in the Purkinje fibers. A special case of parietal block is the so-called peri-infarction block, in which jagged R wave,
usually in the descending segment, is noted in leads in which direct signs of infarction are recorded in the form of pathological
Q
ST
segment elevation or negative
T
Diagnostic value of EPI
for intraventricular blockades consists mainly of distinguishing three-bundle blockade and a combination of nodal and atrioventricular blockade with blockade of one or two branches of the His bundle by recording an intracardiac ECG.
Recommendations from the American College of Cardiology, the American Heart Association, and the Pacer and Electrophysiology Society of North America {P. Zipes et al., 1995) provide the following indications for EPI in patients with chronic intraventricular blockades:
A. Absolute - the presence of symptoms, primarily fainting or presyncope, which may be caused by cerebral hypoperfusion during brady- or tachyarrhythmias. The study includes a programmable pacemaker for
induction of sustained ventricular tachycardia.
B. Relative (not recognized by all specialists) - clarification of the localization and degree of blockade and its connection with pharmacotherapy in asymptomatic cases, if, in the opinion of the doctor, this is important for treatment and assessment of prognosis.
EPI is not indicated for asymptomatic bundle branch blocks and in cases where the connection of symptoms in such patients with brady or tachyarrhythmias is established using a conventional electrocardiographic study.
Course and prognosis. In patients with bilateral two-fascicle blocks, especially those involving the posteroinferior branch of the left bundle branch, there is a slight increase in the risk of complete atrioventricular block with Morgagni-Adams-Stokes attacks (up to 6%). This risk is significantly higher with a three-bundle block with prolongation of the H
-
V
(more than 100 ms) or when subcommissural atrioventricular blockade develops in patients with double-fascicular block during frequent atrial pacemaker.
In this regard, in such cases, some experts consider it advisable to implant a pacemaker for preventive purposes.
With left bundle branch block and single-fascicle blocks not associated with acute myocardial infarction, the likelihood of complete atrioventricular block is no greater than in the absence of intraventricular conduction disorders.
The prognosis is determined by the nature of the organic heart disease. In patients with left bundle branch block, it is worse than with blockade of its anterosuperior branch or right bundle branch, due to the presence in most of these cases of widespread myocardial damage. Their mortality rate over 10 years is 50%, which is 5 times higher than in persons without left bundle branch block (J. McAnulty et al., 1982).
In patients with acute myocardial infarction, the occurrence of blockade of the left or right bundle branch leads to an increase in hospital mortality to 40-50 %.
She reaches
60—70 %
with bilateral two-fascicle blockade. This is due to the increased risk of high-degree atrioventricular block and the greater prevalence of infarction.
Treatment involves preventing complete atrioventricular block with a rare rhythm and Morgagni-Adams-Stokes attacks in patients with an increased risk of its occurrence by implanting a permanent pacemaker.
According to the recommendations of the American College of Cardiology and the American Heart Association (L. Dreifus et al., 1991), the absolute indications for permanent pacemaker during intraventricular blockades are:
1) two-bundle block with intermittent symptomatic complete atrioventricular block;
2) two- or three-fascicle blockade with intermittent asymptomatic atrioventricular blockade of the second degree, type II.
There is an opinion, which is not, however, generally accepted, about the advisability of implanting a pacemaker also in the following cases:
1) two-bundle or three-bundle block with a history of fainting, the cause of which may be complete atrioventricular block (after excluding other possible causes);
2) two-bundle blockade with prolongation of the H
-
V
(more than 100 ms)g, i.e. three-fascicle blockade;
3) two-bundle blockade with sub-branch atrioventricular blockade induced during atrial pacemaker.
Permanent pacemaker is not indicated for asymptomatic bundle branch blocks, including those combined with first-degree atrioventricular block.
VENTRICULAR ASSYSTOLIA
Diagnosis of the disease
Carrying out a standard ECG with incomplete blockade of the right bundle branch is the main diagnostic method. Further examination depends on what type of blockade is detected:
- Incomplete right - without the presence of heart disease is considered as a physiological norm.
- Double-beam – requires more thorough diagnosis.
- Complete left or three-bundle - require immediate hospitalization to determine the cause, even without the patient complaining of certain symptoms.
Other diagnostic methods are biochemical and clinical blood tests, urine tests, daily ECG monitoring, echocardiography, MRI and MSCT (magnetic resonance and multispiral tomography).
Without diagnostics, it is impossible to begin full treatment of the blockade. When a significant number of ventricular contractions are lost, their number decreases. This phenomenon can be observed both with partial and complete violation. If impulse obstruction is suspected, the doctor prescribes ECG studies and blood hormone levels.
When the bundle branches are partially blocked, the ECG shows that the electrical impulse travels at a slow pace. A wave is recorded demonstrating atrial contraction, but a wave of ventricular contraction is absent. When an incomplete block of PNPG is detected, the ECG shows small notches on the S wave, and changes are noticeable on the right side.
The duration of the QRS complex in patients with partial obstruction of nerve impulses may remain within normal limits, but in most cases it is 0.9–1.1 seconds.
To identify the presence of diseases that can cause partial obstruction of electrical impulses, the cardiologist additionally prescribes these research methods:
- general blood and urine tests;
- biochemical blood test;
- Ultrasound of the heart;
- in severe diagnostic cases, computed tomography or magnetic resonance imaging is used;
- transesophageal electrocardiography;
- 24-hour ECG monitoring is used to identify transient disorders.
Based on the results of tests and consultations with a cardiac surgeon, an accurate diagnosis is made, allowing competent therapy to be prescribed.
The doctor receives the bulk of information about the degree of conduction disturbance along the His bundle and its branches from the ECG described above, because it is impossible to listen to it or determine it based on symptoms. To clarify the diagnosis, 24-hour monitoring or transesophageal ECG recording can be performed.
If the blockade has developed against the background of organic changes in the heart, then the patient is shown an ultrasound examination; if necessary, MRI and scintigraphy can be performed.
Complications
The prognosis is favorable for young people who do not have organic heart disease. Often, blockage of the right leg of the heart does not pose such a threat as blockage of the left. But still, the pathological condition can have consequences.
A complication develops in the form of ventricular tachycardia. The pathology manifests itself as an accelerated heartbeat. It often causes severe consequences. There is a risk of ventricular fibrillation; if it is not properly treated, the patient may die.
To avoid serious consequences, you should undergo periodic examination by a cardiologist. Self-medication is strictly prohibited.
serdechka.ru
Sinus arrhythmia: types and symptoms
With incomplete blockade of the right UA, patients often experience sinus arrhythmia, which is a failure of normal heart contractions. Normally, the heart is characterized by sinus rhythm. At the same time, it contracts at rest in an adult 60-90 times per minute. If the rhythm deviates from the norm, they speak of cardiac arrhythmia. The following types of sinus arrhythmia can be distinguished:
- tachycardia - rapid heartbeat;
- bradycardia – slow heartbeat;
- Irregular heartbeat.
In relation to the site of damage, blockades are distinguished:
- sinoauricular,
- atrial,
- atrioventricular (AV),
- intraventricular.
The most common occurrence is atrioventricular block and conduction disturbances in individual bundle branches (two bundles of fibers into which the conduction system splits inside the ventricles).