Heart block is an abnormal heart rhythm in which the heart beats too slowly. Why is this happening and what to do? Let's find out together with the experts. Each heartbeat occurs in the heart's upper right chamber (atrium) in the sinus node, a bundle of specialized cells that act as the heart's natural pacemaker. When it beats, an electrical signal from the upper chambers goes to the lower chambers, which causes the heart to contract and pump blood. Heart block disrupts this normal rhythm.
Degrees of heart block in adults
Heart block can be first, second, or third degree, depending on the electrical signal abnormality.
First degree heart block. In this case, the electrical impulse still reaches the ventricles, but travels through the AV node more slowly than usual.
Second degree heart block. It is divided into two categories:
- Type I, also called Mobitz block I or Wenckebach AV block, is a less severe form of second-degree heart block in which the electrical signal on its way to the ventricles becomes slower and slower;
- type II, also known as Mobitz block II - in this case, some electrical signals do not reach the ventricles at all, and the heartbeat may be slower than usual.
Third degree heart block. In this embodiment, the electrical signal from the atria to the ventricles is completely blocked. To compensate, part of the ventricles acts as a pacemaker, creating electrical signals. These signals cause the heart to pump blood, but much more slowly than normal.
Classification
There are several types of heart block. They are divided based on the location of the area where the conduction function of the heart is difficult or completely blocked. Due to the development of the disease in different parts of the heart, each blockade has its own characteristic features.
Photo: psodaz / freepik.com
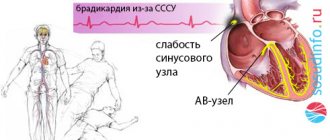
Sinoatrial blockade
Sinoatrial block or sick sinus syndrome (SSNS) develops as a result of complete or partial dysfunction of the sinus node. This can occur both as a result of physiological disorders and due to other factors not related to the state of the body (extracardiac factors).
The main cause of SSSS can be considered fibrosis (development of connective tissue and its scarring) of the sinus node tissue. This pathology can be caused by inflammatory processes, increased tone of the vagal nerve, or taking medications.
SSSU can manifest itself:
- shortness of breath;
- general weakness of the body;
- pain in the heart;
- dizziness and loss of consciousness;
- low blood pressure;
- arrhythmia.
Interatrial block
Interatrial block develops when the propagation of electrical impulses is disrupted, both within and between the atria. The propagation of excitation occurs along special conduction pathways, which are circular and longitudinal muscle bundles, usually not described as part of the specialized conduction system of the heart.
One of the mechanisms of changes in the electrophysiological properties of the atrial myocardium, leading to a slowdown in conduction, is the development of fibrosis. There is a violation of the integrity of myocardial cells with the deposition of collagen in the intercellular space, which prevents the movement of impulses throughout the heart.
Accompanied by general weakness, pain in the chest and abnormal heart rate.
Atrioventricular block
Atrioventricular (AV) block is a partial or complete interruption of the transmission of impulses from the atria to the ventricles, leading to disturbances in heart rate and blood flow rate.
There are 3 types of atrioventricular block:
- 1st degree - due to a slow transition of impulses from the atria to the ventricles;
- 2nd degree - characterized by blocking of some impulses;
- 3rd degree - (complete atrioventricular block), associated with blocking of all impulses coming from the atria to the ventricles.
It occurs due to damage to the most sensitive area of the conduction system of the heart - the atrioventricular junction.
Intraventricular block
Intraventricular block occurs when the His bundle, the conducting region of the heart located in the region of the ventricles, is disrupted. The bundle of His consists of 3 branches: the left and right anterior branches and the posterior branch. The posterior branch is also divided into right and left.
Figure 1. Differences in ECG readings with normal rhythm and with blockades.
Intraventricular block is classified based on damage to 1 of 3 branches:
- Blocking of the anterior right branch - the innervation of the right ventricle is disrupted;
- Blocking of the anterior left branch - in case of disruption of the innervation of the left ventricle;
- Blocking of the posterior branch - the work of the His bundle is disrupted to the greatest extent, since along this branch impulses go from the atria to the ventricles, and are subsequently divided into right and left;
- Three-bundle block is associated with disruption of the conduction of the entire His bundle.
Causes of heart block in adults
The most common cause of heart block is a heart attack.
Other causes include heart disease, problems with the structure of the heart (due to defects) and rheumatism. The blockage can also be caused by damage during open heart surgery, as a side effect of certain medications or exposure to toxins. Heart block can be congenital, but it is a rare pathology. The risk of heart block increases with age and the presence of heart disease.
First-degree heart block is common in well-trained athletes, teenagers, young adults, and people with a highly active vagus nerve.
Treatment
When diagnosing first-degree heart block and first-degree Mobitz block, treatment as such is not necessary. These types of blockades do not pose any serious danger. The doctor may advise you to lead a healthy and active lifestyle, with moderate physical activity, and give up bad habits such as smoking and drinking alcohol.
When diagnosing Mobitz block of the second type and block of the 3rd degree, the patient needs medical attention, since the lack of treatment can lead to death.
The main treatment method for these types of blockades is the installation of a pacemaker. This device is surgically placed near the heart and monitors the correct frequency and rate of generation of electrical impulses.
Pacemaker. Photo: PantherMediaSeller / Depositphotos
Diagnostics
First, the cardiologist will review the patient's medical history and ask questions about your general health, diet and activity level, and family medical history.
In addition, he will ask about the medications the patient is taking, as well as about bad habits. The doctor will then listen to your heart and check your pulse for signs of heart failure, such as fluid retention in your legs and feet.
In addition, to diagnose heart block, use:
- ECG – this will show the heart rate and rhythm, as well as the timing of electrical signals as they pass through the heart;
- A Holter monitor is a portable ECG that is attached to the patient’s body and records heart activity from 24 to 48 hours;
- An event monitor is another type of portable ECG that is worn over an extended period, where the device records heart activity at specific times rather than continuously;
- Electrophysiology test - This test uses thin flexible wires (catheters) that are placed on the surface of the heart to record its electrical activity.
Main symptoms of bradycardia
The clinical picture of bradycardia disease corresponds to the changes in central hemodynamics that develop in this case. Characteristic signs for this pathology are revealed during the initial examination, i.e. during a patient interview. Already on the basis of the most characteristic complaints, a preliminary diagnosis can be made.
The frequency of certain symptoms and the most characteristic complaints depends on the severity of the disease, the severity of hemodynamic changes and the duration of the disease at the time of visiting a doctor.
The patient's age suggests a high probability of developing cardiac arrhythmias. The etiology of the disease may be an important factor in deciding whether pacemaker implantation is necessary.
Popular questions and answers
Cardiologist Stanislav Snikhovsky answered our questions about heart block.
What complications can occur with heart block?
Clinically, all heart blocks are manifested by slowing of the pulse.
When the pulse rate decreases, fainting conditions associated with a lack of blood circulation to the brain may develop. Patients may complain of irregular heartbeat, headache and shortness of breath. With complete heart block (pulse about 40 beats per minute or less), Morgagni-Edams-Stokes syndrome develops, which is manifested by convulsions and loss of consciousness. Complete heart block causes rapid development of heart failure and can be fatal.
When to call a doctor at home if you have a heart block?
If there is sudden general weakness or fainting, a rare (less than 50 beats per minute) or very weak pulse, a feeling of irregular heartbeat, sudden shortness of breath and a feeling of lack of air, you should immediately call an ambulance.
Differential diagnosis
Differential forecast:
- Atrioventricular dissociation. The rhythm of contraction of the ventricles in comparison with the frequency of contraction of the atria increases.
- Atrial blocked extrasystole. In contrast to 2nd degree blockade, there is no pattern between the loss of the QRS complex and the shortening of the P-P interval. The P waves change shape. Subsequently, prolapse of the ventricular complex is observed.
- Slipping rhythm. There are waves on the ECG, their frequency is increased. Complete blockade differs from the escape rhythm by the higher frequency of the QRS complexes.
Second degree blockade is also characterized by loss of the QRS complex.
Diagnostic capabilities
- ECG - allows you to detect bradycardia or transient SA and AV blockades at the time of treatment.
- 24-hour Holter monitoring is the most reliable method for diagnosing incoming heart rhythm disturbances per day of observation (continuous ECG recording).
- EchoCG - a decrease in the ejection fraction below 45%, an increase in the size and volume of the heart that arose against the background of bradycardia, indicates severe myocardial pathology.
- An X-ray examination of the chest allows one to assess the size of the heart shadow and identify signs of venous congestion in the lungs.
- Bicycle ergometry allows you to identify coronary artery disease and assess the adequate increase in heart rate contractions during physical activity.
- Transesophageal examination of the cardiac conduction system is carried out to confirm the diagnosis in cases where transient blockades cannot be detected by conventional methods (ECG, Holter monitoring), in the presence of clinical manifestations. In some cases, it allows one to verify the organic or functional etiology of cardiac arrhythmias.
to the top of the page
Diet food
After diagnosing a patient with a transient 1st degree blockade, cardiologists recommend changing the diet.
To improve conductivity in the AV node, it is necessary that the foods consumed have enough potassium, magnesium and calcium.
Products that improve AV node conduction:
- seeds;
- honey;
- dried fruits;
- bananas;
- baked potatoes with skins;
- dairy products;
- seafood;
- cottage cheese, sour cream, cheese;
- fresh fruits;
- vegetables;
- sea fish.
Salted and smoked foods, confectionery sweets, and artificial fats are excluded from the diet. If you are obese, you need to lose those extra pounds that put a strain on the heart.
Transient AV block: what not to eat:
- lard, meat with fat;
- animal fats, butter;
- strong broths;
- canned food and marinades;
- sour cabbage;
- seasonings and sauces with hot pepper;
- chocolate;
- coffee;
- cocoa;
- Black tea;
- alcoholic drinks;
- sparkling waters.
On the table of a patient with cardiac disease there should be vegetables, preferably fresh or stewed in olive oil, porridge, boiled, lean meat, and dairy products.
If you have high cholesterol, the number of eggs is limited; it is advisable not to serve them whole, but to add them to dishes according to the recipe. Fresh bread made from white flour is replaced by bread made from wholemeal flour, baked yesterday.