Defects of the cardiovascular system are mostly invisible to the patient. But up to a certain point. Many diagnoses are made after the fact, after an autopsy. Some diseases do not produce any symptoms at all and do not affect the anatomical state of the muscle organ.
Sinoatrial block is a disruption of the movement of electrical impulses from the natural pacemaker (sinus node) to the underlying chambers of the heart (atria and ventricles). Several structures of the heart are involved at once, hence the generalized disruption of its functioning.
The signal does not reach the ventricles, so they contract incorrectly (beats are skipped).
With prolonged damage, ventricular fibrillation develops: chambers that do not receive an external impulse begin to generate it independently. This can be fatal in the short term.
Treatment is carried out under the supervision of a cardiologist, preferably in a hospital until all the nuances are identified. Full recovery presents some difficulties: more often, sinoatrial blockade acts as a secondary pathology, occurring against the background of other diseases.
The correct treatment regimen is a simultaneous impact on the cause and symptomatic component.
The essence of the violation
In the normal state of affairs, the muscular organ works autonomously and does not need external stimulation. Uninterrupted functioning is ensured by the presence of a special accumulation of active cardiomyocyte cells - the sinus node. It is located in the right atrium.
The job of this anatomical structure is to generate an electrical impulse that causes the other chambers to contract.
With sinoatrial (SA) blockade, the generation or propagation of an impulse into the underlying chambers of the heart is disrupted. The result is the impossibility of proper stimulation of the ventricles.
Since they do not receive the necessary command, a full reduction does not occur either. The body strives to compensate for this situation. The cameras begin to produce a signal themselves and become spontaneously excited.
But on the one hand, the intensity is not enough for a high-quality release of blood, on the other, the ventricles stop coordinating actions.
The contractions turn out to be chaotic and disorderly. Fibrillation develops, which most likely leads to cardiac arrest.
Another point is the excessive activity of the sinus node itself. This is another compensatory mechanism. The organ begins to produce impulses more often in order to somehow reach the ventricles.
As a result, a patient with advanced sinoatrial block has a history of two dangerous processes: tachycardia as a result of excessive work of the natural pacemaker and fibrillation.
It is difficult not to notice these signs, so diagnosis is prescribed in relatively early stages. Although the situation described is not always so critical. A patient can live with the pathology for years without even suspecting any problems.
Introductory part
Bradycardia is a decrease in heart rate less than 55 beats per minute.
Sometimes bradycardia is a variant of the norm, for example, for a trained cardiovascular system of athletes. But still, bradycardia is more often a consequence of cardiac dysfunction. Bradycardia can also be observed in healthy people, but in any case, pathological causes of its occurrence should be excluded, since, becoming constant, the reduced heart rate leads to the fact that the internal organs begin to suffer from insufficient blood circulation.
Classification and degrees
Typing is carried out according to the severity of the condition.
- SA blockade 1st degree. Represents the initial phase of the disease. There are no symptoms as such, there are no changes in well-being. The patient is active and goes about his daily activities.
It is possible to detect problems during sports, especially at a professional level. Excessive load leads to increased heart rate, impaired myocardial contractility, and chest discomfort.
Additionally, intense shortness of breath and loss of consciousness similar to superficial fainting are detected. After rest, everything falls into place. The objective picture consists of a slight drop in blood pressure and heart rate.
- 2nd degree SA block is an incomplete disruption of impulse conduction. Contractility is still normal, the activity of the sinus node is normal or slightly reduced.
At this stage, severe tachycardia occurs, but the reverse process is also possible. Shortness of breath, sleep disturbances, poor exercise tolerance. All these are moments inherent in pathology.
Depending on the ECG pattern, two types of the described condition are distinguished:
SA blockade 2nd degree, type 1 - the graph reveals chaotic transmission of contractions, usually two or more in a row, possibly with an increase in the impulse conduction time (Samoilov-Wenckebach periods). Clinically, this form is especially dangerous, since it more often causes spontaneous cardiac arrest without the possibility of urgent resuscitation using routine methods.
SA blockade 2nd degree, type 2 - there are no beats symmetrically: there is an alternation of normal contraction and its omission.
- Sinoauricular block of the 3rd degree is considered terminal stage. It takes from several months to years to develop, depending on the aggressiveness of the condition and its underlying cause.
Electrocardiography shows weak contractions. In severe cases, the indicator degenerates almost into a straight line. There is a high risk of asystole or cardiac arrest. This can happen at any time.
The patient needs to be hospitalized urgently. Third degree sinoatrial block is extremely difficult to treat. Radical measures are required. If you are lucky and there are no abnormalities in other organs yet, transplantation will help, which in itself is difficult to implement due to the lack of donors.
At its core, sinoatrial block is a type of sick sinus syndrome. It is similar to bundle branch lesions in both manifestations and prognosis.
But it flows much more aggressively, gives more complications and carries great danger, since the disorder affects both ventricles at once, and at stages 2-3 the atria also suffer.
AV block (atrioventricular block) - symptoms and treatment
Treatment of AV block depends on its degree and the presence of concomitant diseases.
In the case of 1st degree AV block, treatment of the underlying pathology that provoked the development of the block is indicated. All patients with this degree of conduction impairment should be monitored to ensure its progression. If intoxication with digitalis preparations (digoxin, strophanthin, corglycon) is detected, they should be discontinued. With increased tone of the parasympathetic nervous system, atropine must be prescribed. Ajmaline, quinidine, procainamide, beta-blockers and potassium should be avoided due to the risk of increasing the degree of AV block [2].
Second degree AV block (primarily type I) in the absence of symptoms and signs of acute cardiac pathology usually does not require active treatment, since there are no objective signs of circulatory disorders.
Special drug treatment is necessary for second degree AV block with slow heart function, causing circulatory disorders and various symptoms. Pharmacotherapy is also indicated in all cases of acute myocardial infarction. Treatment begins with the administration of atropine and isoprenaline, which increase the conduction of impulses in the His bundle. The exception is cases when, due to a very rare rhythm and impaired blood supply, urgent placement of an artificial pacemaker is necessary. Treatment with these drugs is carried out only by a doctor.
To determine treatment tactics, complete AV block can be divided into three groups:
1. Complete AV block without symptoms . No treatment required. This form occurs in a small group of people with congenital or acquired at a young age AV block with a ventricular contraction rate of 50-60 beats per minute. These patients should be monitored, visit a cardiologist and have an ECG done once every 6 months. If your condition worsens and complaints appear, you should definitely consult a doctor. If the ventricles contract less than 40 times per minute and the QRS complexes become wider, a permanent pacemaker should be installed, even in the absence of symptoms. This will help prevent sudden cardiac death.
2. Complete AV block with impaired circulation in the brain or heart . When cerebral circulation is impaired, fainting occurs. The main method of treatment is the installation of a pacemaker. Most doctors consider even a single faint to be an indication for its installation, since each attack may be the last and lead to the death of the patient. Drug therapy is carried out if the pacemaker is ineffective or during preparation for its use. The most suitable drugs are sympathomimetics - orciprenaline (alupent), isoprenaline (isoproterenol, proternol, saventrin). They cannot eliminate complete AV block, but they can increase the automaticity of the replacement ventricular center and maintain the ventricular contraction rate within 50-60 beats per minute. The dosage of the drug is selected individually for different periods of treatment.
Impaired cardiac circulation is associated with heart failure. If fainting is not observed, complete AV block is treated with digitalis and saluretics. To increase the frequency of ventricular contractions and minute volume, long-term therapy with isoprenaline, orciprenaline or ephedrine is indicated. If drug treatment does not improve heart failure, a pacemaker may be necessary.
3. Complete AV block of acute, transient form in case of fresh myocardial infarction, intoxication with cardiac glycosides, myocarditis, after heart surgery. Corticosteroids are an effective treatment for such blockade. They accelerate the resorption of edema and stop the process of inflammation in the area of the AV system. Hydrocortisone is administered intravenously, or prednisolone in tablet form is used.
The role of saluretics in the treatment of complete AV block is still being clarified. By influencing the excretion of salt from the body, they reduce the level of potassium in the serum by 1 mEq/L. This may improve AV conduction, increase the number of ventricular contractions, and stop or reduce the frequency of syncope. It is necessary to take saluretics for a long time, be sure to monitor the level of potassium in the blood.
Causes
Development factors are always cardiac. On the one hand, this makes diagnosis easier. On the other hand, it initially worsens the prognosis.
- Poisoning with phosphorus compounds. Usually these are mineral fertilizers. Patients working in hazardous chemical plants are especially at risk. Once the dangerous factor is eliminated, the likelihood of restoring normal health is almost maximum.
Patients with acute intoxication should be immediately hospitalized for specific treatment measures. The prognosis in this case is relatively favorable.
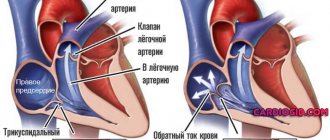
- Congenital and acquired heart defects. What kind doesn't play a big role. This may be stenosis, prolapse of the mitral, aortic valves, disturbances in the anatomical development of the septum and other conditions.
The problem is that it is extremely difficult to detect them if you do not contact a cardiologist every six months or a year for a routine examination.
Findings are mostly accidental, because pathological processes are detected already at irreversible stages. Some cases are even dealt with after the fact, when the person has died.
Sinoatrial blockade of this type is relieved as part of the main surgical treatment.
- Drug overdose. It’s ironic, but drugs designed to lower blood pressure and eliminate arrhythmia, that is, medications aimed at improving the heart, can kill the patient in a matter of hours.
Amiodarone, Quinidine, Digoxin, glycosides in general, and beta blockers are especially dangerous. Third-party drugs include psychotropic drugs, including antipsychotics, antidepressants, and tranquilizers.
It is possible to provoke a similar effect due to the use of oral contraceptives. All drugs should be prescribed only by a specialist after a thorough diagnosis.
- Myocarditis. Inflammation of the heart muscle. It is an infectious, less often autoimmune disease. Requires urgent medical care in a hospital.
Such a dangerous condition cannot be treated on an outpatient basis, since complications are possible, including a heart attack or cardiac arrest. Antibiotics are used in loading doses or immunosuppressants.
As a rule, the condition is secondary. Develops as a complication of colds, rheumatism and others. Sinoatrial blockade after severe myocarditis does not go away on its own.
- Vegetovascular dystonia. Strictly speaking, it does not apply to cardiac problems. However, the normal innervation of the cardiovascular system is disrupted. Hence the deviations in the conductivity of the electrical impulse.
It is a complex symptomatic complex. It manifests itself in many ways: from tachycardia, to dizziness, fainting, shortness of breath and others.
It is not considered an independent diagnosis; you need to look for the cause of this condition. Usually we are talking about hormonal imbalance or pathologies of the cerebral structures themselves.
- Rheumatism. Autoimmune damage to cardiomyocyte cells. The body's protective forces, designed to cover the body, destroy its own tissues. The reasons for this deviation are not fully known. However, rheumatism quite quickly destructs cardiac cells, causing severe scarring and severe heart failure with sinoatrial block.
- Myopathy. Proliferation of the muscle layer, as well as dilatation (expansion) of the chambers of the heart. Restoration is not possible due to the anatomical nature of the deviation. Maintenance therapy under the supervision of a specialist is required. Read more about cardiomyopathy and its types in this article.
- Heart attack and, as a consequence, scarring of the affected areas (cardiosclerosis). It ends with a significant decrease in the conductivity of the natural pathways of electrical impulses. Treatment is required urgently. There is always a risk of death.
In completely healthy people, sinoatrial blockade is also possible. Spontaneous, transient, and transient SA blockades are a consequence of increased activity of the vagus nerve.
Such conditions can be dangerous, but they last only a few minutes, half an hour at most. Patients with no cardiac history and no organic abnormalities in the objective picture are observed by neurologists.
Attention:
There is a chance that the first attack will be the only one, but it is not great. Most likely, we are talking about a disruption of the brain or endocrine system.
In the absence of data for pathologies and functional disorders, they generally speak of an idiopathic form of sinoatrial block. This is a relatively rare option. Typically, diagnostic problems do not arise due to the obviousness of the underlying process.
"Failure" of the SA node. Reasons for the blockade
Sinoatrial blockade
Conditions in which there is difficulty in conducting the impulse and a decrease in its production at the level of the SA node are called sinoatrial block. Blockade of impulses at the very beginning of the path can develop with:
- insufficient production, low frequency of impulse production directly in node No. 1 - sinus;
- low impulse strength, which is not enough to cover the atria with excitation and subsequent spread to the underlying nodes;
- blocking the normal impulse by the sinus node and the right atrium.
Cardiac ischemia
- What is heart block, what are its degrees, treatment methods
All causes of damage to the sinoatrial node can be divided into three main groups:
- Primary. “Breakage” of the node that occurs against the background of its organic lesions, the consequence of ischemic disease, a previous heart attack, the influence of drugs (cardiac glycosides, quinidine, tricyclic antidepressants, Li salts, AK, clonidine) or toxic factors, inflammatory processes in the heart muscle. Primary damage to the sinus node is caused by systemic lesions of the connective tissue, myocardial fibrosis, systemic vasculitis, ankylosing spondylitis, muscular dystrophy, surgical interventions on the lungs and chest, thyrotoxicosis, diabetes mellitus.
- Secondary. Associated with dysfunction of the autonomic nervous system with an excessive increase in n.vagi activity. A physiological increase in the vagus can be observed during sleep, coughing, vomiting, and straining. Physiological changes do not lead to the occurrence of sinoatrial block. This condition can be caused by pathological activity of the vagus nerve with a hiatal hernia, esophageal diverticulum, stroke, brain tumors, disturbances in the electrolyte composition of the blood with an increased concentration of K, sepsis, hypothyroidism, hypothermia.
- Idiopathic. Cases of sinoatrial blockades are characterized when it is impossible to find out the exact cause of their occurrence, in which case they are called idiopathic. Signs of diseases of the heart and other conduction systems cannot be detected with such damage to the SA node.
Stage 1 symptoms
At an early stage, there are no manifestations at all or they are scanty. The clinical picture consists of two signs:
- Severe shortness of breath. But only after intense physical activity. The average person is not active enough to notice a deviation from the norm. In part, problems can be suspected based on the results of specialized tests (bicycle ergometry), but such a test is prescribed only when indicated.
- Tachycardia. Acceleration of the heart rate due to excessive generation of an electrical impulse, against the background of incomplete conduction of the signal to the ventricles. The compensatory mechanism is activated. But he is initially flawed, unable to influence the state of things. Both signs are revealed only after intense physical exertion. An ordinary person does not notice the problem, so diagnosis at stage 1 is almost impossible.
Main manifestations
- Attacks of loss of consciousness or dizziness during a decrease in pulse (Morgagni-Edams-Stokes attacks or MES prodromes).
- Arterial hypertension or unstable blood pressure, poorly corrected by antihypertensive therapy against the background of bradycardia or periodic decreases in heart rate.
- Decreased tolerance to physical activity, increased fatigue, accompanied by bradycardia.
- Chronic circulatory failure in the large and small circles, not amenable to conservative therapy, with constant or intermittent bradycardia.
- Angina pectoris of exertion and rest in combination with a decrease in heart rate, especially in the absence of evidence of stenotic lesions of the coronary arteries.
- Persistent disability of the patient due to decreased heart rate, disease refractoriness to conservative therapy.
to the top of the page
Symptoms at stages 2-3
Phases 2-3 are accompanied by a number of gross changes in condition:
- Chest pain. Pressing or burning. Unlike angina, the episodes are so small that the patient does not have time to pay attention to them. Discomfort is described as a momentary unpleasant sensation that immediately disappears. Duration - from a couple of seconds to several minutes.
- Dyspnea. Against the background of minimal physical activity or at rest. It is extremely difficult to tolerate, the patient is unable to work or perform daily duties. Even going to the store becomes akin to achievement. It is difficult to correct the condition. Usually such patients are given a disability group.
- Heaviness in the chest. It feels like a huge stone has been sewn up.
- Tachycardia and the reverse process. Increase and decrease in heart rate. One may be replaced by another. In parallel, other arrhythmias occur. Ventricular fibrillation. The number of movements reaches 300-400, but they are visible only on electrocardiography.
- Cyanosis of the nasolabial triangle.
- Increased sweating, especially at night.
- Paleness of the skin.
- Fainting may occur more than once during the same day.
- Headache.
- Vertigo, inability to navigate in space.
- Weakness, drowsiness. Long-term decline in labor activity.
- Apathy, unwillingness to do anything.
Sinoatrial blockade of the 2nd degree is accompanied by all the described manifestations, but treatment still has promise.
What is sinoatrial block?
In order to explain the essence of the pathology, you first need to pay attention to the anatomical and physiological features of the human myocardium. As you know, the heart is a partially autonomous organ
Its reduction is ensured by the work of special nerve nodes that conduct nerve impulses.
An important part of the heart rate drivers is the sinus node. It is located between the right atrial appendage and the opening of the superior vena cava, in the wall of the right atrium
The sinoatrial junction has several branches, including the bundle of Thorel, Bachmann, Wenckebach - they conduct impulses to the walls of both atria. Disruption of the normal conduction of nerve impulses in this area is called sinoatrial node block.
Thus, against the background of pathology, disruptions in the heart rhythm occur, which leads to asystole, which, of course, is extremely dangerous. It is worth saying that this is a rather rare pathology - it is diagnosed in 0.16% of patients in the cardiology department. And according to statistical studies, men over fifty years of age most often suffer from the disorder. In female representatives, such a deviation is observed less frequently.
It is possible for the blockade to develop in childhood, but this usually occurs against the background of congenital organic lesions of the myocardium.
Diagnostics
It is carried out under the supervision of a cardiologist. A group of techniques is assigned:
- Oral questioning of the patient and collection of anamnesis. A way to objectify complaints, formalize symptoms and create a clinical picture.
- Measurement of blood pressure, heart rate.
- Daily monitoring using a special tonometer. Allows you to evaluate both heart rate and blood pressure over 24 hours in natural conditions for the patient.
- Electrocardiography. Study of functional indicators. Used as a basic measure.
- Echocardiography. Ultrasound method of tissue visualization. Defects are diagnosed in this way.
- General blood test, hormones and biochemical.
- MRI as indicated.
As part of an extended examination, a neurologist is involved. It is also possible to schedule a consultation with a specialist who works with hormonal imbalances.
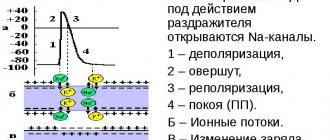
Signs on ECG
At the first stage there are no changes. Problems cannot be detected. Or the features are so nonspecific that they do not give an idea of the nature of the process.
Grade 2 reveals the most pronounced changes on the ECG:
- Passing several pulses in a row at once. Objectively manifested by the complete absence of PQRST complexes on the graph. This is type 1.
For the 2nd, alternating loss of contractions is typical. Yes, no, and so on. Inadequate movements may occur and appear as minor waves.
- PP extension.
- Acceleration or deceleration of the intensity of work of a muscle organ.
SA blockade on the ECG has features of tachycardia or bradycardia and uneven contractile activity.
The third stage is accompanied by impaired functional activity. The graph degenerates almost into a straight line.
Treatment options
The main method of correcting the condition is surgical. Implantation of a pacemaker is indicated, which will artificially control the rhythm.
Medication is a temporary measure and its effect is incomplete.
During acute attacks against the background of autonomic, nervous dysfunction, the following are prescribed:
- Nitroglycerine.
- Atropine or Amizil.
The drugs cannot be abused; they provoke dangerous forms of arrhythmias when used in excess.
In the long term, vitamin and mineral complexes with sufficient amounts of magnesium and potassium, and cardioprotectors (Mildronate) are prescribed.
Attention:
The use of antiarrhythmic drugs is strictly not recommended, as the condition is likely to worsen.
Forecast
Relatively favorable against the background of systematic drug treatment.
If a pacemaker is implanted and the operation is successful, survival rate increases dramatically to 90-95% over a period of 10 years or more.
Lack of therapy is associated with an almost 100% chance of death within a short period of time.
The pathological process cannot always be cured surgically. For some patients, with severe heart defects, severe concomitant conditions, or old age, surgery may be contraindicated.
However, the chance cannot be neglected. First they try to stabilize the patient, then they still consider radical intervention. Otherwise there is no chance of recovery.