Cardiac glycosides are a group of herbal drugs that are used to treat heart failure.
The main function of the myocardium - the heart muscle - is contractility, thanks to which the heart, working like a pump, delivers a sufficient volume of blood to the tissues and cells of the body for their normal functioning.
Heart failure is a disease manifested by a significant decrease in the pumping function of the myocardium, in which the heart actually cannot cope with the loads placed on it. In this case, there is a decrease in the supply of fresh arterial blood rich in oxygen to peripheral organs and tissues, as well as a delay in the return of venous blood that has released oxygen to the heart.
Stagnation of blood in the veins leads to the development of edema - most often the legs swell in the ankles and feet. In addition, stagnation of venous blood in the lungs leads to the accumulation of fluid and increased pressure in the lungs, which is accompanied by shortness of breath and coughing (especially when lying down).
As the severity of heart failure increases, the skin acquires a bluish color (cyanosis), which is especially pronounced in the area of the lips, ears, tip of the nose, and fingers.
Heart failure significantly limits a person's life activity. The slightest physical exertion can lead to weakness, shortness of breath, heart pain or palpitations. Sometimes a patient with heart failure cannot climb several steps without taking a moment's rest.
To treat heart failure, cardiac glycosides are used - special preparations that are obtained from certain plants: digitalis (digitalis), lily of the valley, strophanthus, adonis. Cardiac glycosides increase the strength of heart contractions and alleviate all symptoms of heart failure.
Definition of digitalis intoxication
· Poisoning with cardiac glycosides (digitalis intoxication) is an overdose of drugs from the foxglove plant, for example, digoxin.
· Cardiac glycosides were originally developed from the leaves of various plants (digitalis, lily of the valley) and have been in clinical use for centuries.
· This class of medications is used primarily in the treatment of heart failure and supraventricular arrhythmias.
· Digitalis poisoning is a potentially life-threatening condition.
· Characteristic symptoms appear when the dose of the drug is 1.5–2 times higher than the norm, and if its amount is 5–10 times higher than the permissible daily dose, there is a high probability of death.
· Cardiac glycosides bind to plasma proteins and have a cumulative effect, so digitalis intoxication is not only acute (with a single dose of an excessive dose of the drug), but also chronic (non-critical, but repeated use of a dose of the drug exceeding the daily norm).
Indications for use
Cardiac glycosides are indicated for acute and chronic heart failure.
In addition, certain cardiac glycosides (for example, digoxin) are used for a special form of heart rhythm disorder - atrial fibrillation. Flickering (fluttering) is a phenomenon in which certain parts of the heart (atria or ventricles) contract quickly and randomly or, figuratively speaking, “flutter” like the wings of a butterfly. The heart rate can reach 150-300 per minute with a normal rate of 60-90 heart beats.
Etiology and pathogenesis
At the moment, cardiac glycoside poisoning is less common in medical practice than before, as fewer patients receive digoxin.
General effects:
· Digitalis paralyzes Na + -K + AT and has a strong vagotonic effect.
· Poisoning can be due to intentional acute or accidental chronic overdose.
· The toxic effects of digitalis are enhanced by electrolyte disturbances, especially hypokalemia, as well as cardiovascular and pulmonary disturbances.
· The plasma half-life of digoxin is approximately 36 hours but may be prolonged in renal failure due to delayed urinary excretion.
pharmachologic effect
Cardiac glycoside preparations increase the force of heart contractions, helping to increase the amount of calcium ions in the heart muscle cells. Calcium is critically necessary for any muscle cells (including the myocardium) for full contractile activity.
In addition, cardiac glycosides reduce the frequency (number) of heart contractions, thereby giving the heart the opportunity to rest longer and restore its strength as much as possible in the interval between contractions.
Cardiac glycosides reduce impulse conduction in the conduction system of the heart and normalize pathological heart rhythm.
Additionally, cardiac glycoside preparations, improving blood flow in the kidneys, have a diuretic (diuretic) effect.
Diagnosis of digitalis intoxication
Diagnostic criteria
Clinical suspicion is confirmed by evidence of:
Increased levels of serum digoxin;
· heart failure;
· diseases of the gastrointestinal tract;
· neurological diseases.
The condition can occur due to intentional (acute) or accidental (chronic) overdose.
Acute overdose is characterized by the following symptoms:
- The patient develops nausea, vomiting, and diarrhea.
- Severe abdominal pain occurs.
- Bradycardia.
- Hyperkalemia.
- Atrioventricular block.
Chronic overdose:
- Gradual development of hypokalemia and hypomagnesemia due to concomitant diuretic therapy.
- Development of ventricular arrhythmias - stroke, ventricular tachycardia, ventricular fibrillation.
- Decreased appetite, nausea, vomiting, diarrhea, sometimes severe abdominal pain.
- Neurological symptoms such as lethargy, headache, confusion, hallucinations, color vision disturbances (yellow-green vision).
- Nightmares, psychotic reactions.
- Impaired consciousness, confused speech, drowsiness, loss of strength, convulsions.
Interactions with drugs
Convincing evidence has been provided for changes in plasma concentrations of digoxin when used in combination with other drugs [26, 27, 29]. A decrease in the absorption of digoxin occurs when taken simultaneously with antacids, cholestyramine, sorbents, metoclopramide, sulfasalazine, and cytotoxic drugs.
An increase in the concentration of digoxin in plasma occurs when antiarrhythmic drugs are prescribed (quinidine, amiodarone, propafenone, procainamide, verapamil), drugs with cholinergic properties (atropine, metacin), and angiotensin-converting enzyme inhibitors. The use of non-steroidal anti-inflammatory drugs is associated with the risk of a decrease in GFR, which leads to a decrease in renal excretion of digoxin by 20–30%, and consequently to an increase in its plasma level [26, 29, 31].
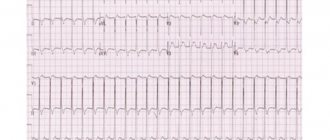
The combined use of digoxin with diuretics increases the risk of developing DTI due to their inherent side effects: hypokalemia, hypomagnesemia (loop and thiazide diuretics), hyperkalemia (potassium-sparing diuretics), hypercalcemia (thiazide diuretics), metabolic alkalosis (loop and thiazide diuretics). In this regard, in patients receiving digoxin and diuretic therapy, it is necessary to monitor plasma levels of electrolytes and electrocardiographic parameters [25–27].
Clinical data
What you should pay attention to when poisoning with digitalis drugs:
- Consider your mental and conscious state.
- Carefully examine the condition of the heart.
- Look for signs of neurological disease.
- Measure serum digoxin levels, potassium, and other electrolytes.
- Electrocardiogram.
- Bradycardia.
- Multiple ventricular extrasystoles.
- Ventricular bigeminy.
- Paroxysmal atrial tachycardia.
- Ventricular tachycardia.
- Ventricular fibrillation.
Non-cardiac symptoms
Noncardiac symptoms of DTI are varied and nonspecific, poorly correlate with serum digoxin levels, and are usually not life-threatening. Among them, symptoms from the gastrointestinal tract, central nervous system and visual apparatus prevail [19, 26–28]. Allergic reactions (skin rash, eosinophilia, fever) are rare when taking SG.
Frequent and often early manifestations of DTI (up to 80% of cases) are anorexia, nausea and vomiting, which have a central origin. Abdominal pain and diarrhea are quite common. Almost all patients with DTI develop weakness, malaise, decreased exercise tolerance, and headache. In 2/3 of cases, various mental disorders are observed, including irritability, nervousness, confusion, and less commonly, disorientation, hallucinations and psychosis [17, 29, 31]. Visual impairments include altered color vision, retrobulbar neuritis, and ocular palsy [37].
Treatment of intoxication with cardiac glycosides
Treatment goals: adjustment of digitalis levels, correction of arrhythmia, prevention of complications.
The treatment regimen depends on the degree of poisoning.
1. Mild poisoning is treated with a temporary pause in taking the drug or reducing the dose.
2. Acute poisoning and stable conditions, e.g. S-digoxin <5 ng/ml requires gastric aspiration, use of activated charcoal, monitoring of S-potassium, correction of hypokalemia.
3. For severe poisoning, provide adequate ventilation and monitor serum potassium and heart rate. Provide symptomatic and antidote drug treatment.
Effect of heroin on the body
Taking this opioid induces a euphoric state. The addict feels a pleasant warmth throughout the body, relaxation and pleasure. When the drug is administered intravenously, the onset of the so-called “arrival” occurs within a few seconds. When applied to mucous membranes - after 3-5 minutes. During the smoking process - literally with the first puff.
Signs of heroin intoxication:
- constriction of the pupils to a point;
- severe drowsiness;
- smooth, good mood;
- slow movements;
- “glassy” look;
- incoherent speech;
- decrease in blood pressure.
Depending on the dose taken, a person under the influence of this substance becomes indifferent to everything that happens around him or, conversely, energetically and enthusiastically begins to engage in routine, everyday activities.
Antidote treatment
1. Ventricular rhythm disturbances are initially treated with lidocaine, 2-3 mg/kg IV.
or phenytoin 10-15 mg/kg slowly i.v. more than 30 minutes.
2. Bradycardia. Initially atropine 0.5-2 mg IV, isoproterenol treated 1-5 mcg/min.
3. Life-threatening digitalis poisoning occurs in arrhythmias with heart failure in which symptomatic treatment is insufficient,
severe bradycardia or AV block that does not respond to atropine, ventricular arrhythmia that does not respond to lidocaine or phenytoin.
4. The development of hyperkalemia (in acute poisoning) causes progressive symptoms of the central nervous system. In these cases, antidigoxin, monovalent antigen-binding fragments, is used. Dosage is based on the estimated amount of glycoside absorbed (see Instructions for Use), so approximately 76 mg of antibody per mg of glycoside absorbed is required. The average dose in adults is 400-800 mg IV. If the dose taken is unknown, it is recommended that 6 mg/kg body weight IV given over 15-30 minutes. If there is no effectiveness, the dose can be repeated after 30 minutes. Hypersensitivity reactions are very rare. An allergy test is carried out before using the drug (see Instructions).
NOTE : Determination of S-digoxin after administration of the antidote gives an incorrect picture of the degree of poisoning because it measures both free and Fab-bound glycoside. Therefore, any repetition of treatment with DigiFab depends on clinical observations.
Electrolyte disturbances
Imbalances in the balance of K+, Na+, Mg2+ and Ca2+ ions are associated with both changes in the effectiveness of SG and the development of DtI. Among these disorders, disturbances of K+ homeostasis occupy an important place. Experimental and clinical studies have shown an increased risk of developing DTI with hypokalemia. This phenomenon is due to a number of factors, including a decrease in the binding of SG to the Na+-K+-ATPase of the sarcolemma, a decrease in the content of Na+-K+-ATPase units in skeletal muscle, the direct effect of hypokalemia on the formation of ectopic foci in the myocardium and conduction disturbances. Electrophysiological mechanisms caused by hypokalemia contribute to an increase in the toxic effects of SG and significantly increase the risk of developing arrhythmias [16].
Unlike hypokalemia, hyperkalemia is not associated with an increased risk of developing DTI. An increase in the concentration of extracellular K+ leads to structural changes in Na+-K+-ATPase, disrupting the connection of SG with it. In addition, with hyperkalemia, stimulation of Na+-K+-ATPase activity is observed. An increase in plasma K+ levels (more than 5.5 mEq/L) stimulates depolarization of the conductive tissue of the heart (especially atrioventricular connections), which may result in a decrease in conductivity and the development of atrioventricular block [26–28].
Ca2+ ions play an important role in the development of DtI. One of the risk factors for DTI is an increase in intracellular Na+, which modifies the Na+-Ca2+ exchange, resulting in an increase in the intracellular Ca2+ content, leading to a slowdown in conduction processes [12]. The above argues for the need to determine plasma levels of electrolytes when using digoxin [32].
Signs of use
It is possible to recognize a heroin addict and prevent the negative consequences of addiction by encouraging treatment. The first thing that catches your eye are the injection marks.
. They are usually located on the bends of the elbows or in the groin.
Strong cravings for sweets, thirst quenched by small sips, saliva dried in the corners of the mouth, sudden changes in lifestyle, frequent colds and other infectious diseases. The above signs should make the patient’s relatives and friends wary.
Drug addicts rarely realize the severity of their situation on their own
. Most of them need confidential, frank conversations, which will result in consent to treatment. After all, the longer a person uses, the greater the chance that sooner or later he will have an overdose.