The cause of acute coronary syndrome (ACS) is almost always a sharp decrease in coronary blood flow caused by occlusion or thrombosis of a coronary artery. Clinical manifestations and consequences of ACS depend on the location of the obstruction, severity and duration of myocardial ischemia.
Of great importance in the treatment of ACS is the identification of individuals at high risk of developing cardiac complications, such as recurrent or repeated acute myocardial infarction (AMI) or death.
Stratification models (scales) make it possible to identify risk groups and, based on the degree of risk, to plan a particular treatment method, which help to more accurately determine the risk in patients with ACS, compared with the expert assessment of experienced doctors.
Risk stratification is considered one of the indicators of the quality of care for patients with ACS, and for its implementation (risk calculation) in patients with ACS, stratification models (scales) TIMI , GRACE, PURSUIT (for patients with ACS without ST-segment elevation), TIMI II (for patients with ACS and ST segment elevation); CADILLAC (when referring patients for percutaneous coronary interventions) and others.
Differentiated use of risk stratification models (scales) for the development of adverse outcomes helps in choosing a treatment strategy for patients with ACS (early invasive or initially conservative), thereby reducing mortality and the frequency of re-hospitalization for myocardial infarction or unstable angina.
What is the GRACE scale for ACS?
The GRACE scale for ACS is a relatively new diagnostic method that allows you to assess all sorts of risks characteristic of acute coronary syndrome. This pathological process is a chronic exacerbation of coronary heart disease, which significantly increases the chances of developing myocardial infarction or unstable angina.
Using such an assessment model, one can effectively estimate the risk of mortality within a hospital department, as well as the overall mortality rate or the development of dangerous complications over a 6-month period.
The scale also allows you to determine the most effective treatment method, which makes it possible to save the patient’s life. In this case, a complex indicator is assessed that correlates with a particular therapy method.
The GRACE scale for ACS includes the following 8 assessment criteria:
- patient's age;
- type of acute heart failure based on the Killip index;
- systolic blood pressure level;
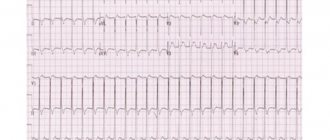
- changes in ST segmentation;
- cardiac arrest, including its quality and frequency;
- level of concentration of creatinine molecules in serum;
- presence of cardiac biological markers;
- tachycardia.
Quantitative assessment of points based on the GRACE scale is characterized by its accurate calculation, both using automatic methods using a calculator that can be installed on a phone or computer, or manually.
The assessed risks of the scale are interpreted as follows:
| Risk | Interpretation |
| Short | In this case, the possibility of death is less than 1% in the case of electronic counting and no more than 109 using manual counting. Here the initial stage is diagnosed, which has the most favorable prognosis for the patient. |
| Average | Considers a mortality risk of 1-3% using the calculator, and 109 to 141 when counting using the manual method. This assessment is an intermediate stage, therefore it is diagnosed most often, in contrast to low or high judgment. In this case, the patient may be prescribed additional therapy and diagnostic tests that can confirm the diagnosis. |
| High | It is characterized by a risk of death of 3% or more in the case of automatic counting, as well as from 140 points in case of manual counting. It is the most dangerous estimate, in which the minimum value of 3% is especially rare. The average mortality rate is from 30 to 60%. |
GRACE scale for ACS
Based on the above interpretation, the doctor determines further treatment of the underlying disease. A particularly high value of 80% is effectively defined as the patient having already died. In this case, many countries resort to the method of euthanasia to eliminate unnecessary suffering for a person.
TIMI scale
The TIMI (Thrombolisis In Myocardial Infarction) scale proposed by Antman et al. in 2000, based on data from two well-known large-scale studies, TIMI-11B and ESSENCE, comparing unfractionated heparin and enoxaparin in PD-ACS.
ESSENCE study followed 3171 patients from 176 centers in the United States, Canada, South America and Europe, randomized within 24 hours of the onset of acute myocardial ischemia without ST-segment elevation on the ECG that occurred at rest. The end point was the sum of deaths, AMI and recurrent angina.
The TIMI 11B study is the largest comparative clinical trial of low molecular weight heparins conducted. The study involved 3910 patients with unstable angina or myocardial infarction; randomization was performed within the first 24 hours of the onset of the disease. Moreover, the majority of patients (81%) also had ischemic changes on the ECG and/or elevated levels of markers of myocardial necrosis in the blood. The end point was the sum of cases of death, MI (including repeated ones) and emergency myocardial revascularization performed due to resumption of angina.
The result of the TIMI 11B study was similar to the ESSENCE study - the reduction in the risk of the sum of adverse outcomes in those receiving enoxaparin was about 15% and persisted until at least 43 days after the start of treatment. At the same time, a significant advantage of enoxaparin was noted already 48 hours after the start of treatment and during this period was maximum during the entire observation period.
E. M. Antman et al. performed a meta-analysis of the effectiveness of enoxaparin in comparison with conventional heparin according to the ESSENCE and TIMI 11B studies, on the basis of which a comprehensive approach was developed to determine the risk of death, MI, recurrent angina and/or the need for urgent revascularization in patients with ACS without ST-segment elevation.
TIMI scale for ACS without ST elevation
The TIMI scale for PD ACS allows you to determine the risk of adverse events within 14 days after their occurrence.
The scale takes into account seven main risk factors:
- age over 65 years;
- the presence of at least three risk factors for IHD (hypercholesterolemia, family history of IHD, diabetes, hypertension);
- previously identified 50% or more stenosis of the coronary artery;
- ST segment deviation;
- two or more attacks of angina in the previous 24 hours;
- taking aspirin within the last seven days;
- elevated serum levels of cardiac biomarkers.
The basic level of risk in the absence of these factors is 4.7%. Each risk factor adds one point, to a maximum of 7 points, which increases the risk level to 40.9%, that is, almost 10 times.
A high TIMI score in PD ST ACS indicates a high risk of death, MI, and recurrent ischemia requiring revascularization. The high-risk group includes patients whose score exceeds 4.
TIMI scale for ST-elevation ACS
The TIMI scale for P ST ACS is based on the EARLY II and allows you to determine the risk of death of a patient within 30 days after the onset of the disease.
It must be remembered that the scale was created on the basis of clinical studies that included patients admitted in the first 6 hours of acute MI with ST segment elevation and treated with thrombolytic drugs - tissue plasminogen activators (alteplase, lanoteplase).
The scale takes into account the following risk factors:
- age over 65 years;
- the presence of diabetes mellitus, hypertension or angina pectoris;
- systolic blood pressure <100 mm Hg. Art.;
- heart rate >100 per minute;
- symptoms of acute heart failure (T. Killip II-IV class);
- body weight <67 kg;
- anterior localization of MI or blockade of the left branch of the His bundle;
- initiation of reperfusion therapy >4 hours.
The basic level of risk in the absence of these factors is 0.8%. Each factor adds points, from a maximum of 9 to 14, which increases the risk level to 36%, i.e. almost 40 times. In addition, the possibility of long-term (3 years) prediction of an increased risk of death, the development of chronic heart failure, and their combination has been shown.
What is it based on?
The GRACE scale is based on the results of numerous studies that have verified the assessment methodology as the most effective diagnostic method.
Registration data from the study were characterized by more than 40,000 subjects who were diagnosed with ACS, while ST elevation or depression was not taken into account. Patients were located in various countries, including South and North America, Europe, as well as New Zealand and Australia.
The analysis on which the methodology is based was carried out from the beginning of 1999 to mid-2005, which made it possible to collect the most reliable and voluminous data from patients from different parts of the Earth. The endpoints that indicated the assessment of mortality were those subjects whose mortality was due to coronary heart disease within six months after discharge from the hospital.
In addition to numerous studies that were carried out with all the standards of scientific specification, the scale is based on the main classification of chronic or acute heart rhythm failure, which is detected in the presence of a previous myocardial infarction.
- I class. There are no symptoms of heart failure, including changes in the overall heart rhythm. Tachycardia is not detected. Analysis of the general hemodynamic indicator is not performed.
- II class. The patient exhibits moderately severe heart failure, the main symptoms of congestion in the pulmonary tissue are present, and there are small wet rales. A hemodynamic analysis is performed.
- III class. There is severe swelling of the lung tissue, disturbances in some heart rhythm functions, tachycardia and a decrease in total oxygen in the blood may develop. In this case, monitoring is a mandatory procedure.
- IV class. The patient develops a cardiogenic shock state. Various complications, differing in severe course, are possible. Hemodynamic monitoring can be repeated to identify underlying pathological processes, as well as to assess the risk of death.
Based on the above classification, treatment is prescribed, which most often involves taking heparin or aspirin, as well as statins and B-blockers. If necessary, the patient may be administered calcium antagonists, as well as angiotensin-converting enzyme inhibitors.
If the patient was admitted to the hospital more than 12 hours ago and if there is a low risk of complications or death, the use of heparins is discontinued. Based on the absence of pathological changes on the ECG, as well as a decreased level of troponins, a repeat biochemical blood test is taken, after which the patient can be discharged.
PURSUIT
The PURSUIT risk assessment model is known, which is based on the design and results of the corresponding study (Platelet Glycoprotein Ilb-IIIa in Unstable Angina: Receptor Suppression Using Integrilin Therapy, 2000).
The protocol for this study was designed to examine the effectiveness of eptifibatide (Integrilin) given in addition to required standard therapy in patients with ACS.
A total of 10,948 patients participated in the study and were randomized within 24 hours of the onset of symptoms of unstable angina or non-Q wave myocardial infarction. Inclusion criteria also included ischemic changes in the terminal portion of the ventricular ECG complex without persistent ST segment elevation.
Changes in the level of serum MB fraction of creatine kinase were taken into account. The end points of the study were death and MI within 30 days of follow-up. The number of end points was also analyzed after 96 hours from the start of treatment.
The scale takes into account criteria such as age, increased heart rate, increased systolic blood pressure, ST segment depression, signs of heart failure, and increased cardiac enzymes in the blood serum. These criteria are associated with an increased mortality and risk of MI (including recurrent MI) within a 30-day period.
When to use
The GRACE scale is primarily used when a patient is suspected of having ACS, as well as in assessing the overall dynamics of the pathological process. This indicator can identify the possibility of developing certain complications, which often lead to death.
The use of the scale is possible in the presence of the following clinical manifestations:
- long-term painful attack of an angiotic nature;
- various pathological changes in the cardiovascular system, which leads to rhythm disturbances;
- manifestations of renal failure.
In addition to the main symptoms that lead to the GRACE score, medical practice takes into account various risk factors that influence the development of certain complications:
- genetically determined predisposition;
- age and gender of the patient;
- abuse of nicotine or alcohol;
- any stage of obesity, diabetes mellitus;
- the presence of physical inactivity and arterial hypertension.
The above symptoms lead to the development of coronary heart disease, which significantly increases the risk of death. In case of suspicion, so-called serum markers can be used, which makes it possible to better see the dynamics of the disease.
When assessing risk, pathological processes such as metabolic syndrome, various congestions in the lung tissue and heart, as well as the presence of repeated ischemia can also be taken into account.
If any of the above characteristics are absent, no points are awarded according to the GRACE table value. In this case, additional diagnostics can be carried out to determine the nature of the disease or identify missing pathological markers.
In case of ACS, coronorography is most often prescribed, which can reduce or completely eliminate negative symptoms in patients with absent ST segment elevation. In addition, revascularization can be used, which makes it possible to improve the long-term or short-term prognosis of the disease.
RECORD
Based on data obtained in the ACS RECORD registry, which was carried out in domestic hospitals, a prognostic scale of the same name was proposed. This suggests its significance specifically for Russia, although it does not exclude the possibility of use in other countries.
RECORD register was conducted from November 2007 to February 2008. 18 hospitals from 13 cities participated in it. A total of 796 patients were included in the register. The condition of 550 of them at admission was regarded as PD ST ACS. Condition 246 was assessed as ACS P ST.
According to the registry, factors independently associated with death were identified (Killip class >11, ST segment elevation on the initial electrocardiogram >1 mm, systolic blood pressure on admission <100 mm Hg, hemoglobin level on admission <110 g/l, age 65 years and older, history of diabetes mellitus), as well as death or development of myocardial infarction during hospital stay.
These factors are combined as equivalent (1 point) into a system (scale) for assessing the risk of developing relevant events. The separation point between high and low risk of death in hospital during ACS was determined (2 points).
According to the results obtained, the proposed scale for assessing the risk of adverse events in patients with ACS has a fairly high prognostic power in relation to both fatal outcome and death or MI during the patients’ hospital stay.
In terms of prognostic value, the RECORD scale was not inferior to the GRACE scale, the use of which is recommended by modern guidelines and which, in patients with PD ACS, in this regard is superior to the TIMI and PURSUIT scales.
However, this result was obtained on a cohort of patients in whom independent prognostic factors for adverse outcomes were identified and included in the RECORD scale. Convincing data can only be obtained by comparing prognosis estimates using different scales on large independent samples of patients with ACS.
The main disadvantage of the RECORD register can be considered its limitations, i.e. small number of participating institutions. Among the advantages of the RECORD scale, one should note its simplicity (even in comparison with the rather simple TIMI scale), as well as the ability to quickly determine its components. To definitively determine the clinical significance of the scale obtained from the RECORD registry, its verification in large independent groups of patients with ACS is required.
Thus, the presented scales demonstrate high predictive accuracy when assessing the risk of death and development (new or recurrent) MI at different times from the moment of hospitalization of patients with ACS.
What is the test for?
The GRACE scale for ACS allows you to assess the overall risk of developing certain complications or pathological conditions that lead to the death of the patient. This indicator takes into account many factors and, based on them, a variation model is built, measured as a percentage ratio.
Thanks to advances in technology, anyone can perform a GRACE analysis using their home computer or phone. Despite the fact that the indicator in automatic research is measured as a percentage, an incorrect conclusion is practically excluded.
Due to the fact that the automatic calculation of the indicator using a calculator eliminates the human factor, this GRACE calculation makes it possible to quickly and effectively assess the main risk of death.
Differentiated use of the scale allows you to choose the best treatment method in case of acute development of ACS. Most therapeutic courses show high effectiveness in early or conservative stages of the disease. Using the scale when making a diagnosis significantly reduces mortality, based on numerous studies, by 50-70%.
Features of the prognostic risk assessment scale
Calculation of the percentage risk ratio is one of the most effective indicators, which allows you to determine the possibility of death in a patient with ACS. In addition to the main GRACE model, other scales are also used in medical practice: TIMI, PURSUIT, CADILLAC. They all differ based on the method of application and the specific disease.
In addition to obvious advantages, the use of prognostic scales includes a number of limitations, due to which such models are used much less frequently, especially in inpatient departments in Russia. Thus, the GRACE register is not carried out in hospitals, instead the RECORD scale is used.
Among other things, to effectively calculate risk using GRACE, it is necessary to obtain data on the amount of creatinine in the blood and its dividing ability, which takes some time. Diagnosis using the TIMI scale is not possible for patients over 60 years of age.
The GRACE prognostic scale shows higher efficiency and accuracy of measurements when compared with the TIMI technique, which does not take into account many minor factors of ACS. This allows us to develop and implement better treatment methods.
Many experts believe that the main predictive value of the GRACE score lies in conducting studies that target general patient populations across multiple countries. This allows for a more accurate analysis of the methodology.
Based on the nuances described above, medical practice is still searching for and developing the most effective scale that would suit all patients without exception. In addition to calculating risk, various biochemical markers have recently become very popular, which makes it possible to determine the pathophysiological basis of the disease, as well as to quickly identify the underlying pathological process.
Modern serum markers are particularly effective for determining myocardial infarction, the most popular of which are the protein structures of type I and II troponins. Their serum concentration increases 3-4 hours after painful attacks, with a decrease occurring within 6-15 days. This biomarker is often used in conjunction with the GRACE score.
In order to more effectively assess risks in the presence of ACS in a patient, a specialized GRACE scale can be used. In addition to manual calculation by a doctor, anyone can calculate the indicator independently using an automatic calculator.
CADILLAC
The CADILLAC risk score was developed based on data from the CADILLAC (the Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications), which included 2082 patients with MI without cardiogenic shock. All underwent primary (but not salvage) PCI with randomization to angioplasty or stenting with or without abciximab.
The resulting criteria were then tested in another independent study, the Stent-Primary Angioplasty in Myocardial Infarction ( Stent-PAMI ), which included similar patients with MI (900 in total) and performed similar interventions, except for the less frequent use of abciximab (5% vs 53%). in CADILLAC). However, 1-month and 1-year mortality rates did not differ between the two studies.
7 predictors were selected that showed their independence in predicting both annual and monthly mortality. They turned out to be:
- left ventricular ejection fraction less than 40% (strength 4 points),
- renal failure - glomerular filtration rate less than 60 ml/min (3 points),
- MI severity class according to T. Killip 2/3 (3 points),
- post-procedural blood flow on the TIMI scale 0-2 (2 points),
- age over 65 years (2 points),
- anemia (2 points),
- three-vessel coronary artery disease (2 points).
To simplify risk stratification, 3 groups were identified: low risk (sum from 0 to 2 points), intermediate risk (3-5 points) and high risk of death (>6 points), which showed high predictive accuracy for both 1-month and for 1-year survival. At the same time, the developed CADILLAC scale turned out to be better than other models used for this purpose (TIMI ST-segment elevation, 2000; PAMI, 2004).
T. Palmerini et al. A comparative study of stratification scales in patients with NSTE-ACS who underwent PCI was conducted, which found that stratification scales, including clinical and angiographic variables, have the highest predictive accuracy for a wide range of endpoints - cardiac mortality, myocardial infarction, target vessel revascularization and stent thrombosis in patients with ACS undergoing PCI.
During annual follow-up, attempts were made to study the prognostic accuracy of models for assessing short- and long-term risk in patients with ACS in the Russian population.
The GRACE prognostic score was ineffective in predicting deaths and cumulative deaths/MI during hospitalization. At the 6-month follow-up period, the scale demonstrated an average level of prognostic significance. Similar performance was found for the TIMI model in predicting death/MI/refractory ischemia at 14-day and 1-year follow-up.
The PURSUIT risk model showed a very good level of predictive value at 30-day and 1-year follow-up. When comparing the GRACE and PURSUIT models for all-cause death and death/MI composites at 12-month follow-up, the PURSUIT scale had better predictive accuracy. One of the features of this study is the small sample size.
A slightly larger study showed higher predictive accuracy of the GRACE score compared with the TIMI score.
According to the Canadian ACS Registry, which is significantly larger in scale than both previous studies, the GRACE and PURSUIT models had comparable predictive power for predicting mortality during hospitalization and within a year after the onset of ACS, superior to the TIMI model. According to other data, the GRACE scale is superior in accuracy to TIMI and PURSUIT.
It is believed that the prognostic value of the GRACE score needs to be tested in patient populations from countries that did not participate in the registry.