Symptoms
Hepatic encephalopathy occurs in several stages, during which the severity of clinical manifestations varies. In general, the disease is accompanied by a wide range of mental and neurological disorders. The main ones are described below.
Sleep disorders
. Patients with hepatic encephalopathy initially experience drowsiness. Subsequently, an inversion (radical change) of the normal rhythm of wakefulness and sleep occurs.
Impaired consciousness
. With this disease, there is usually a decrease in the number of spontaneous actions. The patient rarely fixes his gaze, he exhibits apathy and lethargy, and answers questions briefly. As the condition worsens further, a person suffering from hepatic encephalopathy responds only to intense stimuli.
Personality changes
. Patients may experience a loss of interest in the family and childishness. Moreover, these changes often persist even during the period of remission, which indicates the involvement of the frontal lobes of the brain in the pathological process. With hepatic encephalopathy, patients may be in a state of euphoria or a playful mood.
Intellectual disorders
. Impairments in cognitive functions (memory, attention, etc.) can be mild or severe. In severe cases, confusion occurs.
Speech disorders
. In patients with hepatic encephalopathy, the voice becomes monotonous, and speech becomes slurred and slow. In the future, speech impairment may become even more severe (dysphasia).
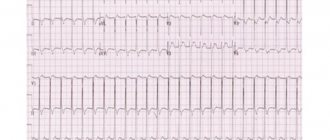
Flapping tremor
. With this disease, a characteristic flapping (flexion-extension) movement of the hand is observed with outstretched arms and widely spaced fingers.
Coma
. At first it may resemble a normal dream, but later the patient stops responding to external stimuli completely.
Latent hepatic encephalopathy
A separate issue that is constantly discussed by experts in the field of management of patients with cirrhosis is latent HE. This topic received a lot of attention from the ISHEN consensus. Hidden PE or mild PE (this form includes minimal and 1st degree PE according to the West-Haven criteria) is very common in clinical practice. As a rule, patients with latent PE are in an outpatient setting and do their usual activities. However, hidden PE negatively affects the quality of life, social and family relationships, the ability to learn and work effectively, and the ability to drive. In addition, it is associated with a higher likelihood of developing overt PE. Therefore, according to the clinical guidelines of the American and European Associations for the Study of the Liver for the management of patients with PE, it is advisable to screen each patient at risk for developing this condition for hidden PE. In our country, psychometric tests such as the “number connection test” and the “line test” are most often used to diagnose latent PE. They require pen and paper and some skill. Screening for mild HE has become easier in recent years with the availability of tools that can be used at the bedside. An example is the animal name test; it is universal and quick to use (does not require equipment and takes only 60 seconds). This test can be performed by physicians, nurses and caregivers and has limited spontaneous variability, making it useful for follow-up/monitoring. The essence of this test is that for 60 seconds the patient is asked to name the names of pets absolutely randomly. A simplified test for animal names is assessed as follows: if within 60 seconds the patient names more than 15 animal names, then there is no encephalopathy (value 0 is assigned), if during this period of time he names from 10 to 15 animal names, then there is a mild degree of PE ( a value of 1 is assigned) if the patient is able to name less than 10 names of animals, that is, a more significant PE and a value of 2 is assigned. This assessment correlated with both the results of psychometric tests (p
Treatment
Specific drug therapy
. Treatment may use drugs that reduce the flow of ammonia or neutralize it in the liver. An important role is played by the use of drugs that reduce inhibitory processes in the central nervous system.
Medical nutrition
. Frequent split meals may be indicated for patients with hepatic encephalopathy. It is recommended to take small meals several times during the day, as well as before bed. Feelings of hunger are not allowed. A low protein diet may be preferable for this condition. Daily protein intake can be 1.2–1.5 g per kilogram of body weight.
Liver transplantation
. This may be the only way to treat severe forms of hepatic encephalopathy that cannot be treated conservatively. This syndrome in itself is not an indication for transplantation. However, it may be recommended in cases where hepatic encephalopathy significantly reduces the patient's quality of life and does not respond to other types of therapy. Then transplantation is possible even if the liver is in satisfactory condition.
Pathogenesis of hepatic encephalopathy: basic principles
Traditionally, PE is divided into overt (with neurological and/or psychiatric abnormalities that can be detected clinically) and latent (with abnormalities that are detected using neuropsychological or neurophysiological tests).
It is believed that the following main factors underlie the pathogenesis of PE: 1) increased ammonia levels in the blood (hyperammonemia) due to the excessive entry into the blood of nitrogen-containing substances synthesized by intestinal bacteria and insufficient neutralizing function of hepatocytes, 2) portosystemic shunting of the blood. A serious role in the pathogenesis of PE is played by the severity of liver damage, the severity of inflammation and/or oxidative stress, age, associated diseases (diabetes mellitus, renal failure), the severity and nature of the factor provoking PE.
Astrocytes absorb ammonia, which is involved in the reaction of converting glutamate into glutamine; an excess of the latter in hyperammonemia leads to swelling of astrocytes and tissue edema. A decrease in glutamate content in astrocytes is accompanied by a disruption of its neurotransmission with the participation of NMDA receptors, as well as an increase in the activity of GABAergic processes. Most likely, these events underlie cognitive deficits, convulsive paroxysms and other clinical manifestations of PE [5, 6].
Despite the long period of studying PE, there are still issues that require clarification: correct diagnosis of both clinically pronounced and latent PE; the role of certain factors in its pathogenesis and, accordingly, diagnostic tools, the choice of optimal therapeutic measures. Separate issues: tactics for managing patients with minimal PE and outpatient treatment, namely monitoring the level of consciousness, the effectiveness of treatment for PE at home.
Causes of hepatoencephalopathy in alcohol dependence
The basis of brain disorders in this disease is liver failure against the background of hepatitis caused by alcohol. Ethanol has a direct damaging effect on liver cells. Hepatocytes are destroyed and cease to perform a number of their basic functions. The acute process is especially dangerous when drinking large quantities of alcoholic beverages.
Malfunction of the liver leads to:
- accumulation of toxins selectively acting on neurons;
- changes in the acid-base properties of blood, hemostasis;
- deviations in the values of oncotic (created by plasma proteins) and hydrostatic pressure;
- disturbance of the electrolyte and water balance of the body.
These pathological processes cause inhibition of the function of astrocytes - cells that act as a natural defense between the tissues of the nervous system and blood.
As a result of the destruction of hepatocytes and astrocytes in the central and peripheral nervous system:
- Unneutralized poisons accumulate;
- electrolyte imbalance occurs;
- a malfunction of neurotransmitters—impulse transmitters—is formed;
- the production of cerebrospinal fluid (CSF) increases sharply, leading to a pronounced increase in intracranial pressure;
- There are increasing signs of cerebral edema.
The following has a particularly destructive effect on nervous tissue:
- ammonia;
- the appearance of false neurotransmitters - substances that replace the main mediators of the nervous system, which leads to insufficient functions of the latter;
- some types of fatty acids and amino acids.
Diagnosis of hepatoencephalopathy
If the damage to the liver and brain is alcoholic, the doctor is interested in:
- symptomatic picture;
- establishing the severity of the disease;
- stage of the process.
Based on the data obtained, during a survey and examination, the doctor prescribes additional types of diagnosis of hepatic ecephalopathy.
These include:
- A detailed clinical blood test with determination of the content of erythrocytes, leukocytes, hemoglobin, platelets.
- Biochemistry data with liver tests, bilirubin, alkaline phosphatase, gamma globulin transferase.
- Ultrasound of the parenchymal organs of the abdominal cavity. The specialist is especially interested in the condition of the liver, pancreas, and kidneys.
- Computed tomography is the most informative method of x-ray diagnostics.
- MRI in doubtful cases, as an additional diagnostic method.
- Needle biopsy as the most accurate option for differential diagnosis.
Our specialists
Tarasova Svetlana Vitalievna
Expert No. 1 in the treatment of headaches and migraines. Head of the Center for the Treatment of Pain and Multiple Sclerosis.
Somnologist.
Epileptologist. Botulinum therapist. The doctor is a neurologist of the highest category. Physiotherapist. Doctor of Medical Sciences.
Experience: 23 years.Derevianko Leonid Sergeevich
Head of the Center for Diagnostics and Treatment of Sleep Disorders.
The doctor is a neurologist of the highest category. Vertebrologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 23 years.
Bezgina Elena Vladimirovna
The doctor is a neurologist of the highest category. Botulinum therapist. Physiotherapist. Experience: 24 years.
Dyachenko Ksenia Vasilievna
Head of the center for the treatment of dizziness and balance disorders.
The doctor is a neurologist of the highest category.
Angioneurologist. Neurorehabilitation specialist. Physiotherapist. Candidate of Medical Sciences.
Experience: 19 years.Drozdova Lyubov Vladimirovna
The doctor is a neurologist. Vertebroneurologist. Ozone therapist. Physiotherapist. Experience: 17 years.
Zhuravleva Nadezhda Vladimirovna
Head of the center for diagnosis and treatment of myasthenia gravis.
The doctor is a neurologist of the highest category. Physiotherapist. Experience: 16 years.
Palagin Maxim Anatolievich
The doctor is a neurologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 6 years.
Forecast and prevention of the disease
The prognosis for the development of the disease, although it depends on a whole range of factors, is almost always negative. The survival rate of patients is higher if the disease develops against the background of chronic liver pathologies. In cirrhosis, the prognosis is seriously worsened in the presence of jaundice and ascites.
In acute liver failure, the prognosis for the development of the disease worsens in children under 10 years of age and adults after 40 years of age due to viral infection. The mortality rate in the first two stages reaches 30%, and in the last stages it exceeds 80%.
Prevention comes down to normalizing lifestyle, avoiding excessive use of medications and timely treatment of diseases that provoke the development of encephalopathy.
Due to the fact that the lethality of the disease directly depends on the stage of its development, timely detection of the disease is of great importance. To do this, it is important, at the slightest suspicion of the presence of the disease, to seek advice from a specialist, as well as to do a CT and MRI. You can undergo diagnostics at one of the clinics located in the service database. The site has collected information about hundreds of diagnostic clinics. A consultant is ready to help you choose a clinic over the phone and make an appointment for a convenient date.
Therapy
Therapy for this disease is a complex process that requires as quickly as possible clarification of the causes of its occurrence. The course of treatment includes: diet therapy, bowel cleansing, lowering nitrogen levels and symptomatic therapy.
It is necessary to reduce the amount of protein coming from food. It is necessary to adhere to this diet for a long time, since an increase in the amount of protein in the diet of a cured patient can provoke a relapse of the disease.
To speed up the excretion of ammonia in feces, it is necessary to achieve at least two bowel movements per day. For this purpose, cleansing enemas are used.
Antibacterial therapy involves taking antimicrobial drugs, the action of which is especially effective in the intestinal lumen (vancomycin, metronidazole, neomycin).
To achieve a sedative effect, benzodiazepine drugs are used, with preference given to haloperidol.