Quick Transition Treatment of Autoimmune Hemolytic Anemia
Autoimmune hemolytic anemia (AIHA) is a group of rare acquired hematological diseases and syndromes characterized by hemolysis (destruction) of red blood cells due to the formation of autoantibodies to the antigens of these blood components.
AIHA can occur at any age; women are more likely to be affected (60%). Pathology develops gradually or suddenly.
There are two main types of AIHA: heat (autoantibodies are most active/attack red blood cells at a temperature of 37-40 ° C) and cold - with cold hemolysins (autoantibodies are most active at temperatures less than 30 ° C, red blood cells are destroyed even with local exposure to cold, for example, when a person drinks cold water or washes his hands in cold water).
The prevalence of AIHA is 1 case per 70-80 thousand people per year.
Causes
The causes of the disease are not well understood. Today it is known that approximately 50% of cases of t-AIHA are idiopathic (develop spontaneously). Whereas x-AIHA are associated with other diseases or occur simultaneously with them: autoimmune, oncological, infectious (systemic lupus erythematosus, lymphocytic leukemia, non-Hodgkin lymphoma, Epstein-Barr virus, cytomegalovirus, mycoplasma pneumonia, hepatitis, HIV). Taking certain medications, for example, penicillin drugs (drug-induced AIHA), can also play a role in the development of AIHA.
Why does anemia occur?
Causes of anemia:
- metabolic disorders involved in hematopoiesis - iron, vitamins B6 and B-12;
- weakness of the hematopoietic system;
- increasing the body's intake of iron and vitamins;
- blood loss;
- hereditary abnormalities of red blood cells;
- gastrointestinal diseases leading to impaired absorption of microelements and vitamins;
- infections;
- immune pathologies;
- breakdown of red blood cells;
- acute and chronic (occupational) poisoning;
- irradiation
There are conditions that require periodic laboratory testing for anemia:
- chronic pathologies of hematopoiesis, gastrointestinal tract of the heart, liver, kidneys;
- period of pregnancy and lactation;
- hemorrhoids, hypermenorrhea, fibroids and other ailments accompanied by bleeding;
- childhood;
- puberty;
- recent operations or injuries accompanied by significant blood loss;
- professional sports;
- systemic diseases - lupus, rheumatism, vasculitis;
- infections;
- condition after blood transfusion;
- following strict diets;
- undergone radiation and chemotherapy;
- work in hazardous industries.
Symptoms
In some people, the disease may be asymptomatic, especially if AIHA develops gradually (the destruction of red blood cells is not as extensive). Basically, the symptoms of AIHA are similar to the clinical manifestations of other types of anemia (weakness, increased fatigue, pale skin).
Symptoms of more severe disease (rapid destruction of red blood cells) include jaundice of the skin and visible mucous membranes, weakness, fatigue with tachycardia and shortness of breath on exertion, abdominal discomfort, a feeling of fullness, cold extremities and peripheral cyanosis (with cold AIHA) . Physical examination reveals splenomegaly (pathological enlargement of the spleen) of varying degrees.
If AIHA develops against the background of another pathology, symptoms of the underlying disease may predominate, for example: enlarged and painful lymph nodes, fever, severe back and leg pain, headaches, vomiting, diarrhea, dark brown urine color.
Changes in blood tests due to anemia
To diagnose anemia and determine its type, blood is taken from a finger and a vein. For some types of anemia, a urine test is performed for bile pigments, which are formed as a result of the breakdown of red blood cells and concomitant liver damage.
Determine in blood:
- Red blood cell content and hematocrit;
- Reticulocyte concentration;
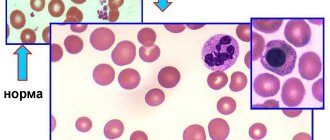
- The presence of red blood cells of irregular shape , composition and size;
- Color index (CI) , based on this criterion, anemia is divided into three types: hypochromic - CP is reduced; normochromic - CP is not changed; hyperchromic - the CPU is increased.
- Serum iron concentration . Based on this criterion, anemia is divided into three types: normosideremic - the indicator is normal; hyposideremic – iron concentration is less than normal; hypersideremic – iron content is increased.
- Saturation of blood serum with transferrin , a protein that transports iron, for the formation of red blood cells;
- Leukocyte content . With anemia, both the general indicator and the content of leukocytes of any type (lymphocytes, monocytes, eosinophils, basophils) may change;
- Concentration of bilirubin and haptoglobin;
- Mean erythrocyte diameter (EDD) . Anemia is: normocytic, red cells are normal; microcytic – the size of red blood cells is reduced; macrocytic and megaloblastic - unnaturally large red blood cells are found.
Treatment of autoimmune hemolytic anemia
The first line of treatment for warm autoimmune hemolytic anemia is glucocorticosteroids. High-dose prednisolone monotherapy can be prescribed for 3-6 weeks with a gradual dose reduction or discontinuation thereafter. However, due to the severe side effects of such treatment, short-term pulse therapy with methylprednisolone or dexamethasone is increasingly used. Approximately one third of patients achieve remission, while the rest require maintenance therapy with GCS.
If steroid therapy is ineffective, the possibility of splenectomy (surgical removal of the spleen), biological therapy (rituximab) or immunosuppressive therapy (cyclosporine, azathioprine, etc.) is considered.
The prognosis depends on the root cause of the disease, timely initiation and proper treatment. A favorable prognosis (achievement of remission, long-term remission) is entirely associated with a positive therapeutic response in the patient and the absence of complications.
Patients with cold autoimmune hemolytic anemia are advised to avoid triggers (cold, including infusions of cold solutions), and also undergo treatment for the underlying disease (for example, lymphoma), if the development of c-AIHA is associated with it. First-line therapy for x-AIHA is rituximab. GCS is not the treatment of choice due to the low therapeutic response in patients. Splenectomy is also ineffective. In severe cases, plasmapheresis is recommended.
Publications in the media
Hemolytic anemias are a large group of anemias characterized by a decrease in the average lifespan of red blood cells (normally 120 days). Hemolysis (destruction of red blood cells) can be extravascular (in the spleen, liver or bone marrow) and intravascular. General signs are severe intoxication with chills and fever, pain in the lower back and abdomen, possible shock as a result of impaired microcirculation, jaundice, splenomegaly, hemoglobinuria.
Etiology. Hemolytic anemia occurs due to defects in red blood cells (intracellular factors) or under the influence of causes external to the red blood cells (extracellular factors). Typically, intracellular factors are inherited, and extracellular factors are acquired.
• Extracellular factors. The microenvironment of erythrocytes is represented by plasma and vascular endothelium. The presence of toxic substances or infectious agents in the plasma causes changes in the erythrocyte wall, which leads to: (1) the production of autoantibodies to the altered erythrocyte (a classic example is autoimmune hemolytic anemia), (2) direct destruction of the erythrocyte •• Isoimmune hemolytic anemias are observed in erythroblastosis fetalis; this also includes hemolytic transfusion reactions •• Defects in the vascular endothelium (microangiopathy) can also damage red blood cells - hemolytic microangiopathic anemia. In children, it can occur acutely in the form of hemolytic-uremic syndrome •• Paroxysmal cold hemoglobinuria •• Prescription of certain drugs (for example, sulfonamides, antimalarial drugs) leads to a hemolytic crisis.
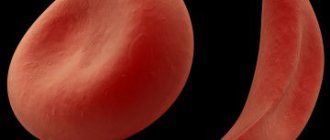
• Intracellular factors. Intracellular defects include abnormalities of red blood cell membranes, Hb, or enzymes. These defects are inherited (excluding paroxysmal nocturnal hemoglobinuria) •• Membrane defects ••• Inherited spherocytosis ••• Inherited elliptocytosis ••• Paroxysmal nocturnal hemoglobinuria •• Hemoglobinopathies (eg, sickle cell anemia). More than 300 diseases are known to be caused by point mutations in globin genes. A defect in the globin molecule contributes to the disruption of its polymerization. The membrane and shape of the red blood cell change, susceptibility to hemolysis increases •• Enzymopathies.
Some hemolytic anemias caused by enzyme deficiency
• Anemia due to deficiency of glucose-6-phosphate dehydrogenase (G-6-PD, see also appendix to this article). Clinical picture: acute episodes of hemolytic anemia, usually provoked by drugs, infections (also with neonatal jaundice and favism). Treatment • Replacement therapy (blood transfusions) • Splenectomy for G-6-PD deficiency is useless • Patients with variants of G-6-PD deficiency associated with acute hemolytic crises should avoid taking drugs that cause hemolysis. ICD-10 D55.0 Anemia due to G-6-PD deficiency.
• Anemia due to pyruvate kinase deficiency. Pyruvate kinase deficiency is the second most common (after G6PD deficiency) inherited erythrocyte enzymopathy. Pyruvate kinase catalyzes the final step of glycolysis; the consequence of its deficiency is inadequate production of adenosine triphosphoric acid (ATP), which negatively affects the functions of red blood cells, incl. at the work of Na+-K+-ATPase - defective cells lose K+. Reticulocytes (mainly in the spleen) undergo especially intensive destruction. Clinical picture • Possible manifestations of hemolysis of varying severity; in newborns - jaundice, chronic hemolysis, splenomegaly • Symptoms of pyruvate kinase deficiency are identical to those in other chronic hemolytic anemias • Due to the selective destruction of reticulocytes, their number in the peripheral blood may not reflect the severity of anemia. Treatment: splenectomy is effective. ICD-10 D55.2 Anemia due to disorders of glycolytic enzymes.
• Hemolytic anemia also develops with Norum's disease, as well as due to deficiency of the erythrocyte form of adenylate kinase (*103000, EC 2.7.4.3, AK1 gene, 9q34.1, r), adenosine triphosphatase (*102800, ATPase, EC 3.6.1.3, r, also B), d-aminolevulinate dehydratase (*125270, porphobilinogen synthetase, EC 4.2.1.24, 9q34, ALAD gene, at least 7 mutant alleles inherited by both r and B), hexokinase 1 (EC 2.7.1.1, *142600 , locus 10q22, gene HK1, r), g-glutamylcysteine synthetase (*230450, EC 6.3.2.2, r], glutathione peroxidase 1 (EC 1.11.1.9, *138320, GPX1, 3q11–q12, r), glutathione reductase ( *138300, EC 1.6.4.2, 8p21.1, GSR gene, r), glucose-6-phosphate isomerase (*172400, EC 5.3.1.9, 19q13.1, GPI gene, Â, r), 2,3-diphosphoglycerate mutases (222800, EC 5.4.2.4, 7q31–q34, BPGM gene, r), enolases (*172430, EC 4.2.1.11, ENO1 gene), coproporphyrinogen oxidase (*121300, EC 1.3.3.3, 3q12, CPO gene, В ), pyrimidine nucleotidase (*266120, EC 3.1.3.5, gene P5N, r), triosephosphate isomerase (*190450, EC 5.3.1.1, 12p13, TPI1 gene), ferrochelatase (*177000, EC 4.99.1.1, 18q21.3, FECH gene, Â, r), phosphoglycerate kinase (*311800, EC 2.7.2.3, À [Xq13, PGKA gene]; also  [arch. 19, PGKB gene]), 6-phosphogluconolactonase (*172150, EC 3.1.1.31), phosphofructokinase (*171860, EC 2.7.1.11, 21q22.3, PFKL gene). Treatment is individualized depending on the type of hemolytic anemia (for example, splenectomy or iron replacement therapy).
ICD-10 • D55 Anemia due to enzyme disorders • D56 Thalassemia • D57 Sickle cell disorders • D58 Other hereditary hemolytic anemias • D59 Acquired hemolytic anemia
APPLICATIONS
Glucose-6-phosphate dehydrogenase (G-6-PD, EC 1.1.1.49, *305900, Xq28) is important for maintaining the intracellular content of reduced nucleotides; inherited enzyme deficiency (A, extreme polymorphism, more than three hundred allelic variants) leads to the development of anemia, favism, and chronic granulomatous disease. There are variants of the enzyme: variant A and Mediterranean • Option A is found in African Americans (rapidly degrading isoenzyme, half-life - 13 days) • Mediterranean variant is found mainly in Greeks and Italians (extreme instability of the enzyme, half-life - several hours), in fact, the activity of the isoenzyme absent • In variant A or the Mediterranean variant of G-6-PD deficiency, taking drugs that exhibit oxidative properties (sulfonamides, salicylates, phenacetin) causes an acute hemolytic crisis after 1–3 days of the incubation period. The subsequent course of the disease is different for the two variants of the enzyme •• Option A. Hemolysis of the pre-existing erythrocyte population occurs. The hemolytic crisis resolves when new populations of red blood cells with high G-6-PD activity are formed in the bone marrow •• Mediterranean variant. Hemolysis leads to the destruction of almost all red blood cells. Transfusion is indicated until the drug is completely eliminated from the body.
Favism (primaquine anemia) is an acute condition that occurs when eating certain types of legumes (for example, fava beans Vicia fava), as a result of inhalation of pollen from their flowers, as well as after taking certain drugs (primaquine, sulfonamides, salicylates, nitrofurans, vitamin derivatives K, etc.). It is found everywhere, but more often in areas where malaria is endemic. Possible in some people with hereditary G6PD deficiency (305900, G6PD gene, Xq28). Clinical picture: high body temperature, headache, abdominal pain, hemolytic anemia, eosinophilia, jaundice, diarrhea, vomiting, loss of strength and coma. Treatment is supportive • blood transfusions • folic acid • maintaining adequate diuresis • urine alkalinization. ICD-10. D55.0 Anemia due to deficiency of glucose-6-phosphate dehydrogenase. Favism.
Paroxysmal nocturnal hemoglobinuria is a chronic disease with episodes of hemolytic anemia and hemoglobinuria (mainly at night). Characteristic features include yellowness of the skin or its bronze coloration, moderate enlargement of the spleen, and sometimes the liver, macrocytosis, and anisocytosis. Rarely observed (2/1 million population). Predisposition to developing the disease (*311770, Xq22.1, PIGA gene, À). Diagnosis: episodes of morning black urine; when table sugar is added to the patient's blood, hemolysis occurs. Treatment. GCs (eg, prednisolone 20–40 mg/day) cause stable remission in 50% of patients. Plasma transfusions are not recommended, but washed red blood cells can be transfused during crises. Heparin should be used with caution, because increased hemolysis is possible. Iron supplements orally. Synonyms: Marchiafava–Miceli syndrome, Marchiafava–Miceli disease. ICD-10. D59.5 Paroxysmal nocturnal hemoglobinuria. Cold is a rare disease characterized by the occurrence of hemolysis after cold exposure (atmospheric air, cold water). Usually occurs after a viral infection. Hemolysis is induced by Donath–Landsteiner hemolysins fixed on erythrocytes. The course can be acute, progressive or recurrent. Synonyms: Donath-Landsteiner hemolytic anemia, Dressler syndrome, Harley syndrome. ICD-10. D59.6 Hemoglobinuria due to hemolysis caused by other external causes.
Stomatocytosis • I (#185020, 9q34.1, EPB72 gene [133090], Â), mutation of the stomatin gene (internal protein of erythrocyte membranes). Clinically: hemolytic anemia, stomatocytosis. Laboratory: shortening of the circulation time of erythrocytes, their increased osmotic resistance, increase in the intracellular content of sodium ions • Stomatocytosis II (*185010, Â). Clinically: hemolytic anemia, stomatocytosis, cholelithiasis, periodic jaundice. Laboratory: decreased osmotic resistance of erythrocytes, increased intracellular sodium • Cold-sensitive stomatocytosis (185020, Â). Clinically: hemolytic anemia, stomatocytosis. Laboratory: Increased autohemolysis and increased osmotic resistance of erythrocytes at 5 °C, cold hemolysis prevented by a decrease in pH or an increase in ATP content.
Aldolase deficiency. Fructose-1,6-diphosphate aldolase (triosephosphate lyase, EC 4.1.2.13, 3 isoenzymes: aldolases 1, 2 and 3, or A, B and C) is a glycolytic enzyme that catalyzes the reversible conversion of fructose-1,6-bisphosphate to glyceraldehyde 3 -phosphate and dihydroxyacetone phosphate. Aldolase A is expressed in fetal tissues and skeletal muscles (5% of total muscle protein), aldolase B in the liver, kidneys, and intestines, and aldolase A and C in nervous tissue. Hereditary diseases are known that develop as a result of deficiency of various aldolases. Aldolase A (103850, 16q22–q24, ALDOA gene, r). With enzyme deficiency, congenital non-spherocytic hemolytic anemia develops (jaundice, splenomegaly, cholelithiasis, possible short stature, delayed mental development and puberty). Aldolase B (229600, 9q22, ALDOB gene, r). When the gene is mutated, congenital fructose intolerance (fructosemia) develops. Clinically: sluggish sucking, delayed growth and development, hypoglycemia, metabolic acidosis, vomiting, hepatomegaly, liver cirrhosis, gastrointestinal bleeding, seizures, proximal tubular acidosis. Laboratory: fructosemia, hyperbilirubinemia, hyperuricemia, glucosuria, hypophosphatemia and phosphaturia, high urine pH values. ICD-10. D55.2 Anemia due to disorders of glycolytic enzymes.
B6 and B12 - deficiency anemia
The causes of anemia caused by a lack of B vitamins are most often poor nutrition, gastrointestinal diseases, parasites and pregnancy.
Anemia of this type can be a consequence of chronic poisoning of the body when working in hazardous conditions, taking certain medications and alcoholism.
Giant red blood cells and neutrophils are found in the blood. Red cells of oval and pear shape are detected. The white blood cell count is decreased and eosinophils may be absent. The level of bile pigments in the blood is increased, and they are also present in the urine.
Hypoplastic anemia
This type of anemia is caused by infections, hereditary pathologies, industrial poisoning, bone marrow depletion, diseases of the immune and endocrine systems, and radiation.
This form of anemia is caused by weakness of hematopoiesis. Blood elements have a normal shape and size, but their quantity is less than normal. Pancytopenia occurs, a condition caused by the death of cells from which red blood cells should be formed. A poor prognostic sign is a decrease in the number of neutrophils below 0.5 • 109/l.
The number of platelets is also reduced, so the blood does not clot well. Analyzes reveal an acceleration of ESR, an increase in the concentration of serum iron and bilirubin.
There is devastation in the cellular contents of the bone marrow caused by inhibition of blood cells.
Iron refractory anemia
Iron-refractory (sideroblastnaya, sideroahristicheskaya) anemia occurs due to impaired absorption of iron, which occurs in hereditary pathologies, systemic diseases, metabolic disorders, chronic poisoning, and malignant tumors.
With this disease, the serum iron content in the blood reaches 225-260 µmol/l. The excess is deposited in sideroblasts and siderocytes - cells of the spinal cord, the number of which can reach up to 70%. Formations are formed in the organs - hemosiderosis, consisting of glandular compounds.
Improper iron metabolism interferes with the production of red blood cells, the concentration of which drops to 1.0 • 1012 / l., and hemoglobin can be less than 30 g / l. The color index also decreases
The number of reticulocytes increases. Macrocytes are found in the blood - large immature red blood cells, defective and ugly blood cells.
Sickle anemia and thalassemia
In these hereditary diseases, the developing red blood cells have an irregular shape and unusual inclusions - Jolly bodies, Cabo accumulation of hemoglobin in the center resembling a target (target-shaped red blood cells).
Hereditary disorders are often diagnosed in people who have ancestors from North Africa, Western Asia, Central Asia and Azerbaijan.
In patients from childhood, a sharp decrease in the amount of hemoglobin to 50 - 70 g/l and a decrease in the number of erythrocytes to 1 - 2 • 109/l are diagnosed. The concentration of reticulocytes increases to 30% of the total number of leukocytes. In biochemical analysis, an increase in bilirubin and serum iron is observed.
Due to the wide variety of types of anemia, the diagnosis can only be confirmed or refuted using a set of laboratory tests. Tests are taken during the diagnostic period and during treatment. You can take all types of tests for anemia at the Diana private clinic.
Make an appointment with a gynecologist by calling +7 (812) 528-88-65, request a call back or fill out the appointment form on the page!
Degrees of anemia
| Degree | Hemoglobin g/l |
| light | 90-110 |
| average | 70-100 |
| heavy | 70 g/l |
If with a mild degree all other laboratory parameters may be normal, then with moderate and severe cases other blood parameters also change. Severe anemia requires identification of its causes and type, so patients are prescribed a comprehensive examination.
Hemorrhagic anemia
This type of anemia can be acute, resulting from massive blood loss due to surgery, miscarriage, ectopic pregnancy, difficult childbirth. Anemia can be chronic, caused by minor but frequent bleeding.
The erythrocyte content drops to less than 3.5 1012 l; immediately after the loss of a large amount of blood, the indicator can be significantly reduced down to 2.1 1012 l. The hemoglobin content decreases - the lower this indicator, the more severe the anemia.
The average volume of red blood cells decreases. In the blood, the content of underdeveloped or deformed red cells increases, which cannot function properly. The number of immature red blood cells - reticulocytes - increases because red blood cells do not have time to mature.
The number of leukocytes in the blood drops, because with blood loss not only red blood cells are lost, but also white cells.
Blood parameters measured for anemia
| index | Norm |
| hemoglobin (Hb) | men - 130-170 g/l women outside pregnancy 120-150 g/l; pregnant <110 g/l |
| red blood cells | men – 3.9–5.5•1012 /l. women 3.9–4.7•1012 /l |
| SOE | men 1-10 mm/h women 2-15 mm/hour |
| mean erythrocyte volume (MCV) | 80-97 in |
| average amount of Hb in a single erythrocyte (MSN) | 27.-34 picograms |
| Average Hb in erythrocytes MSHC | 315-360 g/l |
| retikulotsitı | 5-15‰ |
| hematocrit | women outside pregnancy - 0.36 - 0.48 (36-48%) |
| color indicator | 0,8– 1,1 |
| serum iron | 9.0 – 31.3 µmol/l |
| iron content in transferrin | 15-50% |
| gaptoglobin | 0.3-2.0 g/l |
| bilirubin | 5.2-20.0 µmol/l |
| leukocytes | total quantity 4 -9×109/l, |
| segmented 47-70% | |
| rod 1-6% lymphocytes: 19-37% | |
| eosinophils: 0.5-5% | |
| monotsits: 3-11% | |
| basophils: 0-1% |
If anemia is suspected, not all of these tests may be prescribed, but only part of them. Laboratory diagnostic methods are determined by the doctor based on the patient’s complaints and existing symptoms.