Paroxysmal supraventricular tachycardia, abbreviated as PVT, is a type of arrhythmia. Accompanied by a heart rate (HR) from 140 to 220 or more beats per minute. It arises spontaneously and ends unexpectedly. The duration of PNT is at least three cardiac cycles, while maintaining a regular heart rhythm. The attack itself can last from a few seconds to several days.
PNT occurs due to disruption of the nervous regulation of cardiac activity or damage to other organs.
In the first case, excessive nerve stimulation leads to an increase in heart rate.
PNT can also occur in healthy people under the influence of certain factors:
- prolonged physical activity;
- stress;
- consumption of energy and stimulant drinks;
- bad habits.
In the case of organic damage, paroxysmal supraventricular tachycardia can be caused by:
- damage to the heart muscle due to ischemia, inflammation, intoxication;
- myocardial infarction;
- heart disease;
- pathology of the cardiac conduction system.
In addition to heart disease, other organs can affect paroxysmal supraventricular tachycardia. It is worth checking the functioning of the kidneys, lungs and gastrointestinal tract, especially if there are chronic or acute diseases.
Symptoms of paroxysmal supraventricular tachycardia
Paroxysmal tachycardia always has a sudden, distinct onset. The patient feels a push or compression, and sometimes a prick, in the area of the heart.
The attack may be accompanied by symptoms:
- dizziness;
- noise in the head;
- lightheadedness or fainting;
- sweating;
- nausea;
- trembling in the body.
To correctly diagnose tachycardia, it is important to conduct a thorough interview and examination of the patient. Highly qualified doctors of the Cardiology Center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency will be able to quickly identify the disease.
Treatment
NVT therapy has 2 goals:
- relief of paroxysms;
- prevention of paroxysms.
According to the professional standard protocol, the algorithm for stopping SVT is as follows: vagal maneuvers → electrical cardioversion → drug cardioversion.
To relieve an attack of supraventricular tachycardia, so-called vagal tests are very effective, which act on the principle of mechanical or reflex irritation of the vagus nerve, which slows down the heart rate. The following techniques are distinguished:
- Valsalva maneuver - straining the face with swelling of the cheeks for 20-30 seconds after maximum inhalation;
- massage of the carotid sinus - strong pressure and massage of the carotid artery in the area of the angle of the lower jaw;
- Aschner's test - pressing on closed eyeballs for 5 seconds;
- cold - washing your face or dipping your head in cold water;
- forcibly inducing the gag reflex - by stimulating the root of the tongue;
- rapid and severe cough.
In my practice, I prefer the Valsalva maneuver as the safest.
If, after the above manipulations, the attack continues, electric current is applied using external cardioversion or transesophageal stimulation.
If these measures are ineffective or impossible to implement due to the lack of appropriate equipment, I resort to intravenous administration of the following antiarrhythmic drugs (drugs):
- "Trifosadenine" ("ATP");
- "Verapamil", "Diltiazem";
- "Propranolol", "Esmolol", "Sotalol";
- "Amiodarone";
- "Procainamide."
To prevent attacks, the most effective surgical method is radiofrequency ablation (RFA), which involves destroying the arrhythmogenic area of the heart with high-frequency current. This method is contraindicated during pregnancy, as it involves x-ray exposure.
For drug prevention of paroxysms, the same drugs are used as for stopping an attack, only they are used in the form of tablets, not injections.
The criterion that the treatment of supraventricular tachycardia was successful is the cessation of attacks.
Are traditional methods of treatment effective?
On the Internet you can find a wide variety of traditional medicine recipes for the treatment of all types of arrhythmias, including SVT. However, it is worth knowing that to date there has been no reliable data on any effectiveness of alternative methods of therapy.
Moreover, many herbs are pharmacologically incompatible with antiarrhythmic drugs, i.e., when used together, the effectiveness may decrease or, conversely, the likelihood of side effects of the drug may increase. Therefore, the use of traditional medicine methods can be not only useless, but also harmful.
In my practice, I often meet patients who do not trust traditional treatment methods. It is difficult to encourage them to take life-saving medications. In such cases, I resort to tricks by allowing them to use the desired folk remedies (agreed with me, of course), but only in combination with the necessary pills. Traditional medicine is full of recipes using mixtures, tinctures and decoctions. You can read about how arrhythmia is treated with herbs here.
Diagnostics
Tachycardia can be sinus and paroxysmal; they differ from the location of the electrical impulse that causes the heart to contract. To make a diagnosis, the doctor of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency performs a physical examination, collects anamnesis and prescribes tests.
Physical examination includes:
- external examination of the patient;
- heart rate measurement;
- blood pressure measurement.
Instrumental research:
- ECG;
- ECG with additional load on the body;
- daily ECG monitoring;
- ECHO;
- stress echocardiography;
- MRI;
- CT cardiography.
Signs on ECG
All NVT have common signs on the cardiogram:
- increased heart rate (HR) - from 100 to 250 per minute;
Of course, each type of arrhythmia has its own individual characteristics on film. This happens because the rhythm disorder is based on inadequate electrical activity of the heart and it is different in each case. It is worth mentioning the following features of cardiograms for NVT:
- Before a paroxysm of sinoatrial reciprocal tachycardia, an atrial extrasystole is necessarily present.
- The atrial type is characterized by a change in the shape of the P wave (decreased amplitude, deformation, negativity). It is possible to develop first degree AV block, which appears on film as a prolongation of the PQ interval.
- In SVC syndrome, three specific signs are identified: the presence of a delta wave, shortening of the PQ interval, widening and deformation of the QRS complex.
- Atrial fibrillation and flutter. P waves are completely absent. Instead, there are frequent large F waves (with flutter) or small random f waves.
Sometimes it happens that supraventricular tachycardia is not visible on the ECG, this especially often happens in the paroxysmal form. Therefore, I almost always prescribe Holter (24-hour) ECG monitoring to my patients.
To identify rare SVTs that have additional impulse pathways, a special intracardiac electrophysiological study is performed. It is of great importance, since based on the results of this test the need for surgical treatment is determined.
Prevention
Prevention lies in early diagnosis. Often, success directly depends on the patient and his attitude towards his health. Basic recommendations that should be followed during prevention:
- moderate regular physical activity;
- proper nutrition;
- rejection of bad habits;
- avoidance of situations that lead to stress and cause anxiety;
- compliance with the instructions of the attending physician.
The main thing is to diagnose tachycardia in a timely manner in order to move on to prevention in time. You can get acquainted with the programs of our center by following the link.
Causes
Many reasons contributing to the occurrence of supraventricular tachycardia can be divided into 2 groups:
- Extracardiac - external factors, diseases or conditions not related to the heart that can trigger arrhythmia:
- emotional stress or physical stress;
- consumption of nicotine, alcohol, caffeine, medications (cardiac glycosides, antidepressants, diuretics);
- endocrinological diseases - for example, hyperfunction of the thyroid gland (thyrotoxicosis) or an adrenal tumor that produces adrenaline and norepinephrine (pheochromocytoma);
- fever;
- anemia;
- electrolyte disturbances - excess or, conversely, deficiency of certain minerals in the blood (potassium, sodium, magnesium, calcium);
- shift in acid-base balance (blood pH).
- Intracardiac - This includes organic heart diseases:
- coronary heart disease (CHD);
- chronic heart failure (CHF);
- congenital and acquired heart defects;
- cardiomyopathy;
- pericarditis;
- post-infarction cardiosclerosis;
- chronic cor pulmonale
How to treat paroxysmal supraventricular tachycardia
There are several treatment options at the FMBA center. Depending on the severity of the illness, the attending physician may place you in the therapeutic department. You will be under the constant supervision of professionals and receive timely medical care. This is usually drug therapy. If the symptoms of standard therapy are not enough, then you may be offered catheter ablation of the arrhythmia. At the same time, by puncture access under local anesthesia, under X-ray control using a catheter, an accurate diagnosis of the source of arrhythmia is made and, by precisely influencing it with a radiofrequency pulse or cold, the cause of paroxysmal tachycardia is eliminated.
Description
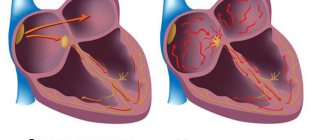
Supraventricular (or supraventricular) tachycardias (SVT) are a large group of heart rhythm disorders in which there are 3 or more consecutive heart contractions above 100 beats per minute.
As the name suggests, the source of pathological impulses that cause arrhythmia is located above the ventricles - in the atria, atrioventricular junction and sinoatrial node.
SVTs are much less life-threatening than ventricular tachycardias! The greatest danger is not the tachycardias themselves, but the diseases against which they develop.
The prevalence of rhythm disturbance is 2.25 per 1000 people. Women are predominantly affected. The distribution among age groups (children, adults, elderly) differs for each individual type of SVT. For example, sinus tachycardia (you can read more about it here) is often diagnosed in children, as is early ventricular repolarization syndrome. In the ICD, supraventricular tachyarrhythmias are coded I47.0 and I47.1.
The clinical manifestations of NVT are very diverse - from completely asymptomatic to repeated loss of consciousness.
Clinical case
A 34-year-old woman came to my clinic for an appointment with complaints of attacks of rapid heartbeat, accompanied by a feeling of lightheadedness and slight dizziness.
These symptoms began to bother the patient about 2 months ago. The woman also noted that she had recently become irritable and her sleep had worsened. General examination revealed an irregular pulse and an enlarged thyroid gland. The patient underwent an ECG, which showed no pathological changes. The patient was referred for consultation to a cardiologist and endocrinologist. The cardiologist performed Holter ECG monitoring, which revealed paroxysms of monomorphic atrial tachycardia with a heart rate of up to 160/min. Ultrasound and thyroid hormones prescribed by the endocrinologist showed signs of autoimmune thyroiditis - diffuse enlargement of the thyroid gland, decreased TSH levels, high concentrations of T4 and antibodies to TPO.
A diagnosis of Hashimoto's thyroiditis, thyrotoxic phase, paroxysmal PT was made. Beta blockers were prescribed to reduce heart rate, and further observation by an endocrinologist was indicated to monitor hormonal levels and replacement therapy.