Arrhythmia is any deviation from the normal heart rhythm, while the normal heart rate at rest for an adult is taken to be 60-90 beats per minute. Disorders that differ in the mechanisms of occurrence, manifestations and prognosis are combined under one term. In general, arrhythmia is associated with a violation of the generation and conduction of electrical cardiac impulses. These pathologies can themselves cause severe disturbances in the functioning of the heart or other organs, or be complications of other serious diseases. If you need treatment for arrhythmia in Moscow, contact our specialists.
Common Causes of Heart Rhythm Abnormalities
Arrhythmias, depending on the mechanism of formation, are conventionally divided into two groups: organic (associated with cardiac pathology) and inorganic/functional (not associated with it).
Organic arrhythmias
The development of such arrhythmias is based on damage to the heart muscle, which prevents the normal propagation of an electrical impulse through the conduction system of the heart to its various parts. Damage may be ischemic, inflammatory or morphological in nature. Thus, scar tissue formed during cardiosclerosis makes it difficult for the myocardium to perform its conductive function and, thus, contributes to the occurrence of conduction and rhythm disturbances. Often, various forms of organic arrhythmias and blockades accompany cardiac pathologies (coronary heart disease, myocarditis, heart failure, etc.), and are also complications of cardiac surgery.
Functional arrhythmias
Neurogenic sympathizers . The reason for the development of such arrhythmias is an excessive increase in the tone of the sympathetic nervous system due to stress, strong emotional experiences, neurosis, intense mental or physical activity. Smoking, drinking alcohol, strong tea and coffee, and spicy foods are also provoking factors. Symptom-dependent arrhythmias of neurogenic origin can also be associated with diseases of the thyroid gland, intoxication (viral, bacterial, industrial, etc.), febrile conditions, blood diseases, and hypoxia. Heart rhythm disturbances are observed in women suffering from premenstrual syndrome.
Neurogenic vagodependent. Such arrhythmias are associated with activation of the parasympathetic system (vagus nerve). Rhythm disturbances usually appear at night. The cause of arrhythmia can be diseases of the gastrointestinal tract.
There are also diselectrolyte arrhythmias (associated with disturbances in the electrolyte balance of the blood and myocardium), iatrogenic (arising as a result of taking arrhythmogenic drugs), mechanical (develop after various injuries), idiopathic (considered rhythm disturbances of unknown origin). In addition, when determining the cause of arrhythmia, specialists also take into account the significance of hereditary predisposition.
Types of arrhythmia
The most common types of arrhythmia are:
- sinus tachycardia . Tachycardia is an increased heart rate. The sinus is the main node of the myocardial conduction system. It is the disruption of its functioning that causes sinus tachycardia. The heart rate increases to 120-150 beats per minute. Sinus tachycardia can be physiological - caused by a reason not related to diseases (physical activity, overheating, emotional experiences). In this case, after the cessation of the cause that caused the tachycardia, the normal heartbeat should be restored. If tachycardia is not associated with such conditions, then it is most likely of a pathological nature;
- bradycardia - slow heart rate (heart rate less than 60 beats per minute);
- paroxysmal tachycardia . Paroxysmal tachycardia is characterized by a paroxysmal increase in heart rate to 140-200 beats per minute. The attack begins and ends suddenly. With the onset of an attack, you must take a horizontal position and call an ambulance;
- atrial fibrillation is a disordered contraction of the heart. With atrial fibrillation, the heart does not contract as a single whole; individual groups of atrial muscle fibers contract uncoordinated and chaotically. As a result, the heart rate can fluctuate between 40 and 500 beats per minute. An attack of atrial fibrillation may precede a stroke, therefore, if such an attack is observed for the first time, urgent hospitalization is necessary.
Types and symptoms of arrhythmias
Cardiac arrhythmia requiring treatment has different symptoms depending on the frequency and rhythm of heart contractions, their effect on intracardiac, cerebral and renal hemodynamics, as well as left ventricular myocardial function. There are the following types of disease.
Bradycardia
With this pathology, the heart rate is less than 60 beats per minute. In trained people whose bodies are accustomed to regular physical activity, bradycardia can be considered normal, but is often a sign of heart problems. The main symptoms of cardiac arrhythmia include weakness, fainting, short-term loss of consciousness, cold sweat, pain in the heart area, as well as dizziness and blood pressure instability.
Tachycardia
With tachycardia, the heart rate exceeds 90 beats per minute. Rhythm disturbances may have a physiological or pathological cause. In the first case, the increase in heart rate is not associated with the presence of diseases of the cardiovascular system. Physiological tachycardia can be considered normal if it is provoked by an increase in physical or emotional stress. Rhythm disturbances in such cases are based on anxiety, a feeling of fear, increased body temperature, sudden adoption of a vertical position and other factors. A short-term increase in heart rate may occur after taking certain medications. In turn, pathological tachycardia is always associated with disturbances in the functioning of the cardiovascular or other body systems. Symptoms of this type of arrhythmias include rapid heartbeat, palpable pulsation of the cervical artery, anxiety, dizziness, and fainting.
Atrial fibrillation
One of the most common types of rhythm disturbances. Atrial fibrillation is characterized by irregular heartbeats, atrial flutter, and irregular contraction of the ventricles. In this case, the heart rate increases to 130-150 (sometimes up to 180) beats per minute. The detection rate of this pathology is 1% of cases among people under 60 years of age and about 30% after 75 years of age. Symptoms of atrial fibrillation include a feeling of interruptions, pain in the heart area, dizziness, a sharp feeling of lack of air, shortness of breath, and fatigue.
Extrasystole
This is a fairly common type of cardiac arrhythmia. It is characterized by extraordinary contractions (extrasystoles), which can begin from the atria or ventricles. According to statistics, a single extrasystole occurs in all people at least once in their life. Even in a healthy person who never complains of heart problems, the norm is considered to be 4% of extraordinary contractions of the atria or ventricles of their total number during the day. Pathological extrasystole develops in approximately 75% of people over 50 years of age. Symptoms of this type of arrhythmia include single or paired premature heart contractions, accompanied by a feeling of a strong push in the chest, a feeling of “fading” of the heart, anxiety, or even lack of air.
It is important to know that frequent episodes of extrasystole are a cause for concern. If this happens constantly, coronary and cerebral blood flow decreases, which can provoke angina pectoris (with ischemic heart disease) and cerebrovascular accident. The presence of extrasystole greatly increases the risk of developing atrial fibrillation and sudden cardiac death.
There are also so-called “silent” cardiac arrhythmias, without symptoms, which have no clinical manifestations and are detected during a physical examination or ECG.
Heart rhythm disturbances (arrhythmias)
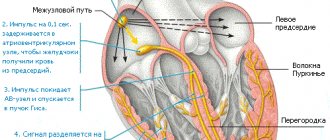
The heart is an incredibly complex organ. Its task is to collect the blood flowing to the heart through the veins and throw this blood into the arteries so that all cells of the body receive their share of nutrients and oxygen. Reacting to an increase in the nutritional needs of any organ or the whole organism, it increases the release of blood into the arteries. The heart consists of four chambers - two atria and two ventricles. In a healthy heart, the atria contract first, expelling the blood that entered them from the veins. Blood enters the ventricles of the heart. Contraction of the ventricles (systole) pushes blood into the arteries. In the right atrium, blood collects from the veins of the whole body, then it enters the right ventricle, from there it is released into the arteries of the lungs. In the lungs, the blood is enriched with oxygen, gives off carbon dioxide and is collected in the pulmonary veins. From there, the blood enters the left atrium, then into the left ventricle, and from there into the arteries of the body. The coordination of the heart is ensured by a special conduction system of the heart. These are specialized cells that produce and conduct electrical impulses that direct the coordinated contraction of the heart muscle. The impulse that triggers the contraction of the heart is produced in the right atrium, in the so-called sinus node (pacemaker). It is this node that is responsible for the fact that the heart contracts at a frequency of 60-90 beats per minute. The signal then spreads to the remaining atria, causing them to contract, and then to the ventricles. Disturbances in this system lead to heart rhythm disturbances (arrhythmias).
What are the types of arrhythmias?
Heart contractions follow each other at regular intervals. If this sequence is disrupted, the patient is said to have an arrhythmia. Depending on where the disturbances occur, all arrhythmias are divided into atrial (or supraventricular) and ventricular. Arrhythmia is not an independent disease, but a sign (symptom) of some disease. Therefore, the occurrence of arrhythmia requires mandatory examination by a cardiologist. The patient can detect the presence of arrhythmia himself. To do this, you need to learn to find and count the pulse.
Heart function (rhythms)
If the pulse rate exceeds 90 beats per minute, they speak of tachycardia. The heart rate may increase during physical or emotional stress (this is a normal reaction of a healthy heart). An increase in body temperature causes tachycardia. It is believed that an increase in body temperature by 1 degree leads to an increase in heart rate by 10 beats. Tachycardia can be a sign of many diseases, but it can also be a normal variant. Some types of tachycardia require special antiarrhythmic treatment. If the pulse rate is less than 60 beats per minute, they speak of bradycardia. Bradycardia can occur in absolutely healthy people. It is usually observed in athletes. Moderate bradycardia creates favorable conditions for the blood supply to the heart muscle. This is due to the fact that blood can only flow to it when it is in a state of relaxation (i.e. between contractions). The faster the rhythm, the more blood is needed to replenish the energy costs of the heart muscle, and the relaxation period becomes shorter. Therefore, some medications (for example, atenolol or anaprilin) that can slow down the rhythm (extend the period of relaxation) improve blood supply to the heart muscle. If bradycardia appears suddenly, if the slowdown in rhythm is accompanied by dizziness or loss of consciousness, consult a doctor immediately. You should also consult a doctor if your heart rate is less than 50 per minute and there are no other unfavorable signs. In some forms of bradycardia, it is necessary to implant a special device - a pacemaker. This device takes over control of the heart rhythm when its own pacemaker (sinus node) fails to cope with its task.
Extrasystole
If a premature contraction is woven into the correct rhythm of heart contractions, they speak of extrasystole. According to the place from which the electrical impulse emanates, leading to premature contraction, all extrasystoles are divided into atrial and ventricular. Even an absolutely healthy person can experience extrasystoles several times a day. However, their appearance is a reason to consult a cardiologist. Like all arrhythmias, extrasystole is not an independent disease, but only a sign of some disease. The examination will be aimed at finding the cause of the arrhythmia. Atrial fibrillation is the most common arrhythmia
What is atrial fibrillation
Atrial fibrillation is a type of rhythm disorder in which the atria are excluded from the coordinated work of the heart. An electrical impulse runs at high frequency through the atria, causing chaotic contraction of muscle fibers (fibrillation). Therefore, atrial fibrillation is also sometimes called atrial fibrillation. Some impulses break through to the ventricles, which contract due to this in an incorrect, irregular rhythm. The absence of the correct rhythm is the main sign of atrial fibrillation. Sometimes it is not possible to identify the cause of atrial fibrillation, then they talk about its idiopathic form. Most often, atrial fibrillation is a sign of heart disease, coronary heart disease, arterial hypertension, etc. Not only cardiovascular diseases can lead to atrial fibrillation. Common causes include diseases of the thyroid gland, lungs, acute and chronic poisoning (for example, alcohol) and many other diseases. It is important that for success in the treatment of atrial fibrillation, it is necessary not only to correctly prescribe special antiarrhythmic drugs, but also to correct its cause.
Manifestations (symptoms) of atrial fibrillation
The most common manifestation of atrial fibrillation is a feeling of palpitations. It is due to the fact that the average ventricular rhythm during atrial fibrillation usually increases and can reach 130-150 beats per minute. Interruptions in the functioning of the heart are often felt, sometimes a sharp feeling of lack of air, pain in the heart area, and dizziness. Approximately 1 in 10 patients does not feel the appearance of atrial fibrillation at all.
Types of atrial fibrillation
Long-term atrial fibrillation is called permanent. If it occurs paroxysmally, they speak of the paroxysmal form. Atrial fibrillation with a high heart rate is called tachysystolic, with a normal frequency - normosystolic and with a low frequency - bradysystolic form.
Is it necessary to treat atrial fibrillation?
According to various estimates, from 1.5 to 5% of humanity suffers from this type of arrhythmia. This is the most common type of arrhythmia requiring treatment. The appearance of atrial fibrillation (if left untreated) significantly (5-7 times) increases the risk of stroke and pulmonary embolism. The likelihood of developing heart failure also increases. Additional factors such as age and the presence of severe concomitant diseases further increase the risk of stroke and heart failure in patients with atrial fibrillation. Therefore, atrial fibrillation must be treated without fail.
Restoring the correct heart rhythm
The goal of treatment for a patient suffering from atrial fibrillation is, if possible, the restoration of the sinus (correct) heart rhythm and its subsequent maintenance. There are several ways to restore the correct rhythm. The first - the simplest - can be tried by the patient himself. The method is based on the possibility of stimulating the vagus, a nerve that slows down the heart rate. You need to take a deep breath. Then hold your nose and mouth tightly and try to exhale forcefully. This method can also stop other attacks of palpitations. Unfortunately, this method does not help all patients. The most common is restoring the heart rhythm with the help of medications. These medications are called antiarrhythmics. Typically, medications are administered intravenously. However, in some cases, the patient himself can take a previously selected medicine, which stops the attack of atrial fibrillation. Unfortunately, there are no special signs to determine which medicine will be more effective. In practice, you have to try several medications before choosing the drug that is most suitable for the patient. In some cases, when an attack of atrial fibrillation cannot be treated with medications, if it has existed for a long time, there is an immediate threat to the patient’s life, so-called electrical cardioversion is used to restore the rhythm. The patient falls asleep for a short time (1-2 minutes), then a special synchronized (i.e. applied at a certain phase of the cardiac cycle) electric current discharge restores the heart rhythm. The method has several disadvantages - the need to put the patient to sleep, the need for special equipment to carry out the procedure. In addition, this procedure must be performed in a hospital that has highly trained personnel. But there are also significant advantages. Thus, the rhythm is restored in almost all cases (unlike drugs, which restore the rhythm only in 60-80%). This method is the safest, since any medicine has side effects. If they appear, then it takes time for the medicine to leave the blood. Taking these advantages into account, special devices sewn under the skin - cardioverters - were created that detect atrial fibrillation and stop it. However, these devices are not yet widely used. After the rhythm is restored, it is necessary to maintain it. It is necessary to treat the disease that led to atrial fibrillation and eliminate the factors that provoke the attack. If attacks are rare, then sometimes special antiarrhythmic therapy is abstained. However, most often you have to take medicine to prevent the attack from developing. Sometimes, for frequent attacks that are difficult for patients to tolerate, surgical treatment has to be used.
Maintaining a normal heart rate when rhythm cannot be restored
In some cases, it is necessary to refuse to restore the normal rhythm. Usually in this case the patient has a so-called permanent form of atrial fibrillation. The main therapeutic measures are to maintain a normal heart rate and prevent complications.
Prevention of complications of atrial fibrillation
Since the main complications of atrial fibrillation are stroke and heart failure, their prevention should also be carried out in a patient with atrial fibrillation. The method of such prevention is chosen by your doctor.
Recommendations for a patient with atrial fibrillation
Try to find out and tell your doctor what precedes the next attack of atrial fibrillation. This may be unusual physical activity, increased blood pressure, taking any medications, drinking alcohol, exacerbation of lung disease, etc. Learn to count your pulse (or ask your doctor to teach you) and recognize whether you have atrial fibrillation or whether your heart rhythm is correct. If the attack does not go away on its own within 2-3 hours, does not go away with regular medications, or causes discomfort, pain, or shortness of breath, consult a doctor. The sooner from the moment the attack begins to treat it, the easier it is to restore the correct rhythm. Be sure to have your latest (or several recent) electrocardiograms with you. They may be needed for comparison in an emergency. Do not rely on your memory; have a sheet of paper with you with the name and dosage of the medications you are taking. This may be very important if you are being given a new medicine because many of the substances interact with each other. If you are taking phenylin or syncumar - medications that reduce prothrombin levels and prevent stroke and thromboembolism - do not forget to consult your doctor if:
- signs of bleeding appeared (nosebleeds, blood on the gums when biting, bruises began to appear)
- if you start taking new medications or change the dosage of previously taken medications
- if the diet has changed (for example, a new season has begun)
- if you have a cold, if you have an upset stomach, or any new illness. If you are planning any surgery or tooth extraction, tell your doctor that you are taking these medications.
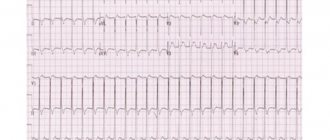
Examination of a patient with arrhythmias
In order to properly treat arrhythmia, it is necessary to undergo a special examination. It consists of two parts. The first is the identification of the arrhythmia itself, the conditions for its occurrence and cessation. The second is the search for the disease that led to the arrhythmia. To detect an arrhythmia, it must be registered. To do this, an electrocardiogram is recorded. The desired arrhythmia is not always detected on a regular ECG. Therefore, the next step is to record an electrocardiogram over a long period of time (usually a day), then, using a special computer, the recording is deciphered. This examination method is called 24-hour Holter ECG monitoring. In some clinics, patients are given special devices to take home that allow them to transmit an ECG to their doctor if necessary. This method also allows you to record rare rhythm disturbances. Physical activity often provokes arrhythmias, so exercise testing is sometimes used to measure the level of acceptable physical activity and evaluate the preventive effect of antiarrhythmic drugs.
Features of heart block
The blockade is associated with a slowdown or cessation of the passage of electrical impulses through the structures of the heart muscle. The root cause may be any myocardial damage, congenital heart disease, atherosclerosis, overdose of certain drugs, dysfunction of the thyroid gland, menopause, etc. The blockade is of the following types:
- depending on the course - transient (passing) or intermittent (arising and disappearing many times during ECG recording), progressive or constant;
- depending on the location - sinoauricular, intraatrial, interatrial, atrioventricular, intraventricular (bundle branch block, conduction disturbance in the myocardium).
Symptoms of heart block, the treatment of which is often necessary, include periodic loss of pulse, fainting, and convulsions.
Missed heartbeat after exercise
Oleg
June 23, 2021
Hello, I’m 31. After minor physical activity, my heart begins to skip a beat. It doesn’t feel like extrasystoles because there is an extraordinary contraction first after a pause, maybe of course I’m wrong, I’m not a specialist in this) But the condition is very frightening, especially when such freezing occurs 5 times in a minute one after another as soon as, for example, I jump off the horizontal bar, and at these moments there is an unpleasant feeling in the throat. In November 2021, I had a mild form of Covid without damage to the lungs, after which I felt fine until February, I’ll say right away that I went in for sports immediately after Covid (. But in February, on the morning after an evening feast, after smoking 1 cigarette, I felt unwell, my limbs went numb, darkening in my eyes , a feeling of fear of death and a pre-fainting state. After drinking Corvalol 40 drops, it didn’t help, they called an ambulance and admitted me to cardiology. At the hospital, when they arrived, everything went away, while I was lying there I had an ECG a couple of times, a 24-hour holter, they took blood, urine, calla, and also did a CT scan of the chest It seems like I was in a standing position. All these tests find nothing, everything is absolutely normal. They are discharged when my condition improves, in the evenings I was sometimes still tormented by a feeling of fear, some kind of anxiety, I also did a separate ultrasound of the heart, which showed everything was normal, and an ultrasound of the thyroid glands (thyroid hormones are normal) discovered small nodules, the endocrinologist prescribed iodomarin for 6 months and said there was nothing wrong. And actually, since February, my life has been like complete hell, I have no feelings of fear for a long time, but to this day I am tormented by some kind of compression in the chest, fullness, heavy breathing, then I can’t exhale completely when I’m relaxed, then I can’t breathe in hard, and there’s a kind of pressure in my throat, I constantly feel my heart pulsating in my throat or in my chest, some kind of spontaneous muscle twitching, I’ve been following a complete healthy lifestyle since February I do sports moderately on the parallel bars, it even becomes easier, but I feel my heart strongly, but I’m used to it. and then literally 3 weeks ago I began to feel these fading described above and accordingly gave up sports and any physical activity. Of the tablets I take: iodomarin, afobazole 3 times a day (already 4 packs since February with breaks), panangin 3 times a day (I only drank half a pack), Nexium from the stomach I finish the pack (I have chronic gastritis since the army and the ulcer was 3mm, at the moment there are no ulcers), I constantly drip into my nose after Covid and my nose is stuffy, maybe that’s because of them. At rest, I don’t experience freezing or I experience it very rarely, but as soon as I do 40 push-ups from the floor and go one after another. Tell me, can I still undergo an ECG under stress, or some other heart examination? I heard that myocarditis occurs after Covid in 70% and can develop into chronic, what’s wrong with me? Maybe it’s just some kind of nervousness, or osteochondrosis of the spine (by the way, my back sometimes hurts in the morning and it’s stiff on the sides, but after exercise everything is fine) In 2021 I was lying with renal colic with an attack, but nothing was found, perhaps the sand had passed. What else can I say, and for about a year now I have been observing how my left side sometimes ache when I sit for a long time in the area somewhere between the pelvic bone and the pubic bone. Please give me some advice, these freezes scare me, what if it freezes and won’t start? Could this happen in my situation? I would be grateful for a good consultation, I’m already exhausted and don’t know what to do.
The question is closed
heart
arrhythmia
fading
COVID-19
Consequences and complications
In the absence of timely treatment, arrhythmias and heart block provoke attacks of angina, pulmonary edema, and thromboembolism. Acute heart failure and even cardiac arrest are possible. According to statistics, in 10-15% of cases, blockades and other types of arrhythmia lead to death. Pathological tachycardia can provoke myocardial infarction. Complete atrioventricular block or asystole can provoke loss of consciousness, which is associated with a decrease in blood supply to the brain. Every sixth case of thromboembolic complications of atrial fibrillation leads to stroke. For arrhythmias caused by different causes, treatment is selected individually.
Causes of arrhythmia
Arrhythmias can be caused by both heart pathologies and diseases of other organs and systems. Among the main reasons are the following:
- diseases of a cardiovascular nature (coronary heart disease, cardiomyopathy, hypertensive crisis, etc.);
- states of shock;
- intoxication (poisoning with alcohol, drugs, food poisoning);
- diseases of the endocrine system (diseases of the thyroid gland, adrenal glands);
- heart surgeries, heart injuries, and many others.
The danger of arrhythmia is that even in the absence of pronounced clinical manifestations and discomfort, without treatment it can lead to serious complications. In particular, a complication of atrial fibrillation is the development of acute heart failure, pulmonary embolism, and cerebrovascular accidents.
Diagnostics
The primary stage of diagnosing arrhythmia and heart block is carried out by a therapist or cardiologist. Based on the patient’s complaints and examination results, the following examinations may be prescribed:
- electrocardiography (including 24-hour Holter monitoring);
- transesophageal/intracardiac electrophysiological study;
- treadmill test (diagnosis of arrhythmias with imitation of conditions causing blockade or other disorders).
If necessary, the doctor prescribes auxiliary diagnostic studies and tests. The accuracy of the results affects the effectiveness of treatment of the blockade or arrhythmia.
Treatment
The choice of treatment for cardiac arrhythmia depends on the type of pathology and the general condition of the patient. In some cases, it is enough to carry out therapy to eliminate the underlying disease. But often special treatment for arrhythmia in the clinic is required, namely:
- medications (membrane stabilizing drugs, β-blockers, etc.);
- cardiac surgery (implantation of a pacemaker or cardioverter-defibrillator, radiofrequency ablation, open heart surgery).
Treatment of atrial block is not required if the patient feels well.
Prevention
- Elimination of cardiac pathology.
- Exclusion of extracardiac factors of arrhythmia or blockade (intoxication, autonomic dysfunction, stress, etc.).
- Limit intake of caffeine-containing products and alcohol.
We will help make a diagnosis at an early stage of the development of blockade, tachycardia or other disorders and provide timely treatment for cardiac arrhythmia. Further observation will allow maintaining a good quality of life. For questions regarding the treatment of cardiac arrhythmia in Moscow, please contact us by dialing the number +7.