Left ventricular aneurysm is difficult to diagnose because... pathology is a complication of diseases or (much less often) injuries. People who have had a myocardial infarction are at risk. At the site of damage to the heart, the muscle tissue becomes thinner, bulges outward under blood pressure, loses its contractility, which leads to poor circulation and the formation of blood clots. An aneurysm appears in a limited area of the anterior wall of the left ventricle, the apex of the heart, or extremely rarely on the lateral wall of the left ventricle.
The pathology often develops in old age in patients with coronary artery disease against the background of the development of transmural myocardial infarction. It is dangerous due to complications and consequences: the development of severe heart failure, thromboembolic complications, arrhythmia, rupture of the aneurysm itself with fatal bleeding.
Causes
The main reason for the development of a left ventricular aneurysm is damage to the heart tissue due to a previous disease. Additional factors for the appearance of pathology are:
- non-cardiac diseases – infectious diseases;
- trauma – the occurrence of pathology due to the consequences of physical impact (gunshot or piercing wound);
- congenital - negative factors affecting the formation of the heart during embryonic development;
- consequences of surgical intervention are extremely rare.
The disease affects people suffering from high blood pressure, coronary heart disease and patients who do not follow doctor's orders after a heart attack: refusal to take medications, ignoring bed rest, returning to work in the acute post-infarction period.
Features of the structure and functioning of the heart. Automaticity of the heart
"Biology. Human. 8th grade". D.V. Kolesova and others.
Question 1. Where is the heart? What are its dimensions? The heart is located in the middle between the right and left lungs and is slightly shifted to the left side. The size of a person's heart is approximately equal to the size of his fist.
Question 2. What layers does the heart wall consist of? The heart wall consists of three layers: the endocardium (the inner epithelial layer), the myocardium (the middle muscular layer) and the epicardium (the outer layer consisting of connective tissue and covered with serous epithelium). The main mass of the heart is the myocardium - it is a striated muscle, which in a number of ways differs from striated skeletal muscle. The outside of the heart is covered by a pericardial sac - the pericardium. The walls of the pericardium secrete fluid, which reduces the friction of the heart during contraction.
Question 3. Why is the wall of the left ventricle more powerful than the right ventricle? Why are the walls of the atria thinner than the walls of the ventricles? The thickness of the muscular wall of the heart depends on the load it performs. The walls of the atria are thinner than the walls of the ventricles, since the force of their contractions only ensures the passage of blood from them to the neighboring chambers - the ventricles. The ventricles send blood to tissues and organs, with the left ventricle through the systemic circulation, and the right through the pulmonary circulation. Hence the difference in the thickness of their walls.
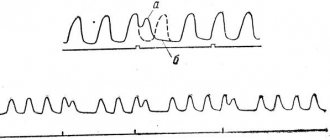
Question 4. What happens in each phase of the cardiac cycle? During the day, the heart contracts 100,000 times and pumps 10 tons of blood. Heart rhythm consists of three phases. Atrial contraction phase Duration of the phase: 0.1 s Blood moves: from the atria to the ventricles State of the valves: Leaflet - open Semilunar - closed Ventricular contraction phase Duration of the phase: 0.3 s Blood moves: from the ventricular arteries State of the valves: Semilunar open Leaflet closed, rise, slam shut and prevent the return of blood to the atria, the threads holding them and the papillary muscles are tense. This prevents blood from entering the atria. Under its pressure, the semilunar valves open at the border between the ventricles and the efferent vessels, and blood is directed from the left ventricle to the aorta, and from the right ventricle to the pulmonary arteries. Relaxation phase Phase duration: 0.4 s. Blood moves: into the atria and ventricles. State of the valves Leaflet - open Semilunar - closed The arteries are stretched under the pressure of the pushed out blood, and the semilunar valves slam shut, and blood rushes through the arteries. The semilunar valves prevent blood from returning to the ventricles of the heart. During the pause, the heart chambers fill with blood. Flap valves are open. From the veins, blood enters the atria and partially flows into the ventricles. This alternating contraction and relaxation allows the myocardium to work throughout a person’s life without getting tired.
Question 5. What is cardiac automatism and how is it combined with nervous and humoral regulation? Automaticity of the heart muscle is the ability of the heart to contract rhythmically under the influence of impulses arising in the heart muscle itself. Thanks to this, the sequence of operation of the heart chambers is maintained regardless of the body’s regulatory systems. Changes in the frequency and strength of heart contractions occur under the influence of impulses from the central nervous system - nervous regulation (sympathetic nerves increase the frequency and strength of heart contractions, and parasympathetic nerves reduce the frequency and strength of heart contractions) and biologically active substances (hormones) entering the blood - humoral regulation ( adrenaline, calcium ions increase the frequency and force of heart contractions, and potassium ions and acetylcholine slow down the activity of the heart and reduce the force of heart contractions).
Symptoms of left ventricular aneurysm
There are no special manifestations of the disease. Clinical symptoms are caused by the underlying pathology or its complications. Most often patients may be concerned about:
- chest pain – occurs during physical exertion or after emotional stress. The attack of pain goes away after rest or taking medication (nitroglycerin);
- shortness of breath, attacks of suffocation - appear after a slight exertion or even at rest. Lack of air can be bothersome during sleep;
- increased heart rate;
- weakness;
- increased fatigue;
- swelling of the limbs;
- memory impairment.
Because the symptoms are subtle and can be bothersome from time to time, it is dangerous to miss the disease and its progression. At the slightest ailment, it is important to consult a specialist. At the cardiology center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, doctors with many years of experience will conduct an examination, give you their recommendations and tell you about a comprehensive heart study that you can undergo in our institution. Do not delay going to the doctor, the consequences of the disease may be irreparable.
Causes of left ventricular chord formation
In 92% of cases, an additional chord arises due to a hereditary tendency to the disease. It is transmitted through the maternal line, less often through the paternal line. Therefore, if a mother knows that an additional chord in the left ventricle of the heart was previously discovered in her, it is worth thinking about examining her child, since the chord does not make itself felt for a long time, and this can cause a complex disease in the future.
Diagnostics
During the appointment, it is important for the doctor to collect a complete medical history, because The pathology may be indicated by an underlying disease - myocardial infarction. After a survey and physical examination, the patient is referred for instrumental studies. Depending on the severity of the symptoms and the patient’s well-being, the doctor determines the research method. In our center, when diagnosing an aneurysm, we use:
- ECG;
- Echocardiography of the heart;
- chest x-ray;
- computed tomography of the heart;
- coronary angiography and ventriculography.
Diagnosis of heart abnormality
In order to accurately diagnose an additional chord in the left ventricle of the heart, the doctor prescribes an ultrasound examination. Thanks to ultrasound, the doctor can quickly, painlessly and accurately diagnose a heart disease or pathology. In addition, echocardiography allows you to study the heart in real time and in motion. The problems of the additional chord are also studied using the Doppler method, which helps determine the length of the thread, its thickness, the location of attachment and the speed of blood flow through it.
Prevention
Prevention is aimed at treating myocardial infarction, which causes the development of an aneurysm. It is important to take medications as prescribed by your doctor and not to violate the dosage regimen. Visit a cardiologist in a timely manner and do not ignore routine examinations.
Additionally, patients should:
- stick to a diet;
- control blood pressure;
- eliminate psycho-emotional stress;
- do exercises and physical warm-up;
- control weight;
- quit smoking.
Following simple rules of treatment and prevention will help improve your health and prevent relapse and progression of the disease. You can contact our specialist for advice and undergo examination in the cardiology department. Only comprehensive measures can help in the fight against the disease.
Treatment of left ventricular aneurysm
In most cases, conservative therapy is used only to relieve symptoms. Drug treatment does not give the desired result. According to numerous scientific studies, the five-year survival rate of patients with cardiac aneurysm with conservative therapy is significantly lower than with timely surgical treatment. The only effective method is cardiac surgery.
Surgical treatment is a radical method of treating cardiac aneurysm. Depending on the area of damage to the left ventricle and its contractile ability (contractility), the cardiac surgeon in our Cardiology Center performs one of the methods of left ventricular plastic surgery: linear plastic surgery, septoventriculoplasty (with the heart’s own tissues), plastic surgery with a biological or synthetic patch.
- If the pathology is accompanied by a blood clot, it is removed during surgery,
- If arrhythmia is present, ablation (cauterization) of areas prone to arrhythmia is performed.
- If normal blood flow is disrupted, coronary artery bypass grafting (CABG) can be performed as an additional step;
Heart failure - symptoms and treatment
The following forms of heart failure are distinguished:
- left- and right-handed;
- systolic and diastolic (heart failure with reduced and preserved ejection fraction);
- acute and chronic.
Left ventricular failure
Left-sided heart failure can be left ventricular or left atrial. It is characterized by a decrease in left ventricular output and/or stagnation of blood on the way to the left parts of the heart, that is, in the veins of the pulmonary circulation.
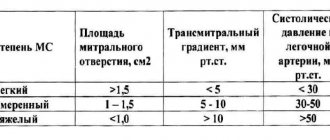
Left ventricular failure usually develops with coronary heart disease (CHD), hypertension, cardiomyopathy, congenital heart defects, heart valve insufficiency, and left atrial failure - with narrowing of the mitral valve opening and, in rare cases, with left atrial myxoma - a benign heart tumor [14].
Symptoms of left-sided heart failure (HF): weakness, dizziness, pale skin, shortness of breath and fatigue.
Right ventricular failure
Right ventricular failure is characterized by a decrease in right ventricular output and stagnation of blood in the veins of the systemic circulation. The condition is usually caused by pre-existing left ventricular failure or severe pulmonary disease [14].
Symptoms of right-sided heart failure: peripheral edema, cyanosis and fluid accumulation in the abdominal cavity.
Isolated heart failure is rare and short-lived. Subsequently, the disorder affects all chambers of the heart and typical symptoms of the disease develop.
Some sources use the term “global heart failure” to describe heart failure of both ventricles. This formulation is incorrect and is not used by doctors. In the literature, the term “total heart failure” is used to describe this condition [17].
Systolic and dystolic heart failure
Impaired pumping function of the left ventricle can be caused by systolic and diastolic dysfunction. Systolic dysfunction is more common and is associated with decreased contractility of the myocardium, the muscle tissue of the heart. In most cases, the cause of systolic chronic heart failure is coronary artery disease, combined with arterial hypertension and diabetes mellitus.
Diastolic dysfunction is caused by impaired active relaxation or increased myocardial stiffness. Patients with this form of the disease are less likely to suffer from coronary artery disease, and more often from arterial hypertension and atrial fibrillation. Among them there are more elderly people, women and obese patients[16].
In addition to the familiar terms “diastolic heart failure” and “systolic heart failure,” the names “ heart failure with preserved LV ejection fraction (HFpEF) ” and “heart failure with reduced ejection fraction (HFrEF)” .
We are talking about the same conditions, but the use of the terms diastolic and systolic HF requires objective evidence obtained using echocardiography, magnetic resonance imaging and isotope studies of the heart. In some sources, these terms are used as synonyms [14][18].
Symptoms for systolic and diastolic HF are similar [13]. These forms of the disease can only be distinguished using instrumental diagnostic methods. Many patients experience both types of dysfunction simultaneously [17].
Acute and chronic heart failure
Symptoms of chronic and acute heart failure differ only in intensity and timing of development.
Stages of development of heart failure
The modern classification of chronic heart failure combines the modified classification of the Russian School of Cardiology according to stages that can only worsen (V. Kh. Vasilenko, M. D. Strazhesko, 1935), and the international classification according to functional classes, which are determined by the patient’s ability to tolerate physical activity (6-minute walk test) and may worsen or improve (New York Cardiology Classification).[2]
Classification of CHF by the Russian Society of Heart Failure Specialists
| FC | FC of CHF (may change during treatment) | NK | Stages of CHF (do not change during treatment) |
| 1FC | There are no restrictions on physical activity; increased workload is accompanied by shortness of breath and/or slow recovery | 1 tbsp | Hidden heart failure |
| 11FC | Minor limitation of physical activity: fatigue, shortness of breath, palpitations | 11a st | Moderately severe hemodynamic disturbances in one of the circulation circles |
| 111FC | Noticeable limitation of physical activity: compared with usual activities, accompanied by symptoms | 11b st | Severe hemodynamic disturbances in both circulation circles |
| 1U FC | Symptoms of heart failure are present at rest and worsen with minimal physical activity. | 111st | Severe hemodynamic disturbances and irreversible structural changes in target organs. The final stage of damage to the heart and other organs |
New York Heart Association classification of heart failure
Class I: Heart disease does not limit physical activity. Normal exercise does not cause fatigue, palpitations or shortness of breath.
Class II. The disease slightly limits physical activity. There are no symptoms at rest. Normal physical activity causes fatigue, palpitations, or shortness of breath.
Class III. Physical activity is significantly limited. There are no symptoms at rest. Little physical activity causes fatigue, palpitations, or shortness of breath.
Class IV. Marked limitation of any physical activity. Symptoms of heart failure appear at rest and worsen with any activity [15].