Functional insufficiency of the tricuspid valve, as a rule, is understood as its insufficiency without organic changes in the elements, against the background of dilatation and dysfunction of the right ventricle, dysfunction of the left ventricle, pulmonary hypertension, which occur with pathology of the mitral and, less commonly, aortic valves. According to the authors [3, 6], functional insufficiency of the tricuspid valve occurs in 8-35% of those operated for mitral or aortic valve disease. In the Framingham study [11], functional tricuspid regurgitation occurred in 16.7% of the general population. At the same time, tricuspid regurgitation is one of the predictors of progression of chronic heart failure and increased mortality after adequate correction of valve defects of the left heart [4, 5, 7]. Currently, in our country there remains a fairly significant group of patients with valvular heart defects of rheumatic etiology, amounting to about 50% [1]. In this regard, it seems important to evaluate the relationship between functional tricuspid valve insufficiency and right ventricular myocardial dysfunction and determine their impact on the condition of patients with rheumatic mitral valve disease.
The purpose of the study was to determine the effect of functional tricuspid insufficiency on the results and course of the disease in patients operated on for rheumatic mitral valve disease.
Tricuspid valve defects
Tricuspid valve defects
Tricuspid valve defects are a group of heart diseases that include tricuspid valve insufficiency, tricuspid stenosis, and tricuspid valve defects with predominant stenosis.
The tricuspid valve is located between the right ventricle and the atrium. Its role is to control the flow of blood from the atrium to the right ventricle.
Tricuspid valve insufficiency leads to its abnormal functioning, as well as failure of the entire heart muscle. The two main types of this pathology include:
- the tricuspid valve does not close tightly or does not close at all, causing blood to flow in the opposite direction;
- stenosis (narrowing) of the tricuspid valve, in which the valve flaps are very stiff and do not open wide enough, causing a restriction in blood flow.
Tricuspid valve defects can be caused by:
- infections, such as infective endocarditis or rheumatism;
- expansion of the right ventricle due to increased rigidity of the tricuspid valve ring;
- increased pressure in the valve;
- Less common causes include birth defects, tricuspid valve prolapse, trauma, carcinoid heart disease, tumors, Ebstein's anomaly, and trauma.
If tricuspid valve insufficiency is caused by rheumatism, then the disease usually occurs in combination with pathology of the aortic or mitral valve.
Heart valve insufficiency - symptoms and treatment
To make a diagnosis, examination, percussion (tapping), electrocardiography, X-ray and ultrasound examination are performed. To clarify the diagnosis, transesophageal echocardiography, catheterization of cavities, computed tomography and magnetic tomography of the heart may be required. Transesophageal echocardiography and catheterization are performed only in the hospital. Computed tomography and magnetic tomography can be done in medical centers or hospitals, usually in large cities.
Inspection, palpation, measurement of pulse and pressure
With aortic insufficiency , due to sharp fluctuations in pressure, pulsation of the peripheral arteries (especially the carotid arteries - “carotid dance”) occurs, visible upon examination. The patient shakes his head rhythmically (Musset's sign). With intense pressure on the top of the nail, the bed at its base alternately turns red and pale (pseudocapillary pulse or Quincke's sign). Sometimes pulsation occurs in the right hypochondrium in the liver projection area. This pulsation is noticeable both during inspection and palpation. This condition is characterized by high blood pressure and a racing pulse, i.e. it is different with each measurement.
When examining and palpating the heart area, there is a noticeable shift in the apical impulse (pulsation of the chest wall) to the left and down, which indicates thickening and expansion of the left ventricle. At the same time, pulsation is observed in the lower part of the thoracic and epigastric regions.
On palpation, the apical impulse is normally dense (“dome-shaped”), its weakening means a strong decrease in myocardial contractility.
Tricuspid valve insufficiency leads to a significant increase in the volume of the right ventricle, diffuse pulsation may be visible throughout the cardiac region. Blood pressure is often reduced, and venous pressure increases to 200–300 mm H2O. Art.
In case of aortic valve insufficiency, you can see and feel the pulsation at the base of the heart, and also detect the pulsation of the aorta in the 2nd intercostal space to the right of the sternum. In patients with aortic valve insufficiency above the femoral artery, instead of one tone, two are detected (double Traube sound), which is associated with sharp fluctuations of the vascular wall both during contraction and relaxation of the heart.
If the defect develops in childhood, then due to the increased contraction of the enlarged heart, the child’s pliable ribs are deformed. As a result, a uniform protrusion appears in the area of the heart - the cardiac hump.
Percussion and auscultation
Using percussion (tapping), it is possible to detect dilation of the heart chambers with tricuspid valve insufficiency and in later stages with mitral valve insufficiency.
With mitral valve insufficiency, the left atrium dilates.
With the simultaneous development of several heart defects, the borders of the heart increase in all directions (cardiomegaly, “bull’s heart”).
With the help of auscultation (listening), it is possible to identify murmurs characteristic of valve insufficiency and weakening of heart sounds.
X-ray diagnostics
Radiography is a screening method, i.e., rapid diagnosis. It allows you to determine the location of the atria and ventricles, as well as identify blood stagnation in the pulmonary circulation.
With mitral valve insufficiency, the left atrium and ventricle enlarge. The heart acquires a mitral configuration: its waist is flattened, first due to a sharp increase in the left sections, and then the right ones.
With aortic valve insufficiency, the size of the left ventricle sharply increases, so the heart takes on an aortic configuration: a “boot” or “sitting duck” shape.
With tricuspid valve insufficiency, increased transparency of the lungs and pronounced cardiomegaly (enlargement of the heart) with a spherical heart shadow due to an enlargement of the right atrium are visible. The arch of the pulmonary artery often disappears.
With pulmonary valve insufficiency, the arch of the pulmonary artery, on the contrary, protrudes, the vascular pattern of the lungs is strengthened, and the right parts of the heart are dilated.
Electrocardiography (ECG)
On the ECG you can see signs of thickening of the heart chambers, their overload, arrhythmia and conduction disturbances.
In case of aortic and mitral valve insufficiency, thickening of the left ventricular myocardium is noticeable on the ECG, even in the asymptomatic period. At later stages, signs of left ventricular overload and relative coronary insufficiency appear. A left bundle branch block may develop.
With tricuspid valve insufficiency on the ECG, the amplitude of the P waves increases, which indicates an enlargement of the right atrium. Blockages may appear and the rhythm may be disrupted.
In case of pulmonary valve insufficiency, ECG data also indicate an increase and overload of the right parts of the heart [7] .
Ultrasound of the heart (transthoracic echocardiography)
Transthoracic (superficial, transthoracic) echocardiography (ECHO-CG) is a simple and safe method for diagnosing heart diseases, including valve insufficiency. It is based on the ability of an ultrasound beam to penetrate tissue and be reflected from it. The reflected ultrasonic signal is perceived by the sensor, processed and converted into an image. Ultrasound allows you to examine the heart, its chambers, valves, endocardium (inner lining), record slight movements of the walls and valves of the heart, record improper attachment of valve leaflets, their anomalies and changes in movement.
Transesophageal echocardiography (TEE-CG)
TEE-KG is a method in which a small ultrasound sensor attached to a device is placed in the esophagus. This position of the sensor increases the resolution of the device and allows you to examine parts of the heart that are closed from the ultrasound beam by dense material (for example, the left atrium can be covered with a mechanical mitral valve prosthesis).
Indications for transesophageal echocardiography for valve insufficiency:
- Infective endocarditis or suspicion of it with low information content of transthoracic ECHO-CG and in all cases of endocarditis of an artificial heart valve.
- Artificial heart valves.
- The need to determine the degree and cause of mitral regurgitation.
- Observation during valve surgery.
- Poor “ultrasonic window”, excluding superficial examination. There are areas in the anterior chest through which the doctor performs an ultrasound. If, after applying the sensor to the desired location, interference appears and it is impossible to get a picture on the monitor, the doctor describes this condition as a “poor ECHO window” or “narrow ECHO window.” Occurs in obesity and narrow intercostal spaces.
Doppler echocardiography
Doppler echocardiographic techniques include color Doppler, continuous wave, pulsed wave and tissue Doppler. They are used to study the speed and direction of blood flow in the chambers of the heart, and to identify and evaluate the degree of regurgitation on the valves.
In a healthy heart, all blood flows at approximately the same speed and in the same direction. If the valves are insufficient, a turbulent blood flow is created in areas of pressure difference, i.e. turbulence appears, layers and blood particles move in different directions. Turbulent flows can be detected using Doppler echocardiography. When performing color Doppler scanning, flows inside the chambers of the heart can be detected and the degree of valvular insufficiency can be determined [8] .
Radionuclide diagnostics (angiography and ventriculography)
Radionuclide diagnostics allows you to assess general and regional contractility of the heart, visualize the valves and walls of the myocardium. It is performed in a special apparatus (gamma camera), which forms an image after the introduction of a radioactive drug. Like CT, radionuclide diagnostics does not carry radiation exposure.
Spiral computed tomography and magnetic resonance imaging (SCT and MRI)
SCT and MRI allow you to obtain an accurate image of the heart, providing information about the condition of the valves and blood flow at the site of the defect.
During CT angiography of the heart, a radiocontrast agent based on iodine is necessarily used, and the body receives radiation exposure. CT contrast can improve the clarity of images of the heart and coronary arteries, but allergies to the injected drug may occur.
Magnetic resonance imaging does not have such side effects and radiation exposure. However, it is contraindicated in patients with installed electronic devices and metal in the body.
Cardiac catheterization
Cardiac catheterization is a minimally invasive procedure performed to both diagnose and treat valvular insufficiency. The surgeon inserts a thin, long and flexible catheter tube, moving it from the groin area to the heart. Through it, a contrast agent is injected into the blood and an image of the heart is obtained in various projections. Thanks to the introduction of a contrast agent, it is possible to evaluate the size of the heart, the contraction of the heart muscle and the function of the valves. During the procedure, if necessary, the pressure in the cavities of the heart is determined. For example, with mitral regurgitation, the pressure in the left atrium and left ventricle is the same.
With the help of catheterization, it is possible to perform plastic surgery on the valve and its prosthetics. Contraindications for catheterization include severe heart failure, infectious and colds, serious heart rhythm disturbances (paroxysmal tachycardia, atrial fibrillation with a large pulse deficit).
Diagnostics
Tricuspid stenosis is usually diagnosed during a routine medical examination. While listening to a child with a phonendoscope, the doctor hears a systolic murmur caused by abnormal blood flow through the valve. A specialist can determine other signs by measuring the pulse and the development of abnormal pulsation in the neck.
Diagnostic studies include the following procedures:
- echocardiography;
- electrocardiography;
- chest x-ray;
- transesophageal echocardiography;
- cardiac catheterization;
- radionuclide scanning;
- Magnetic resonance imaging.
Material and methods
A retrospective analysis of the results of treatment of 56 patients with rheumatic mitral valve disease, operated on in the cardiac surgery department No. 1 of the State Budgetary Institution of Healthcare with Special Clinical Clinical Hospital No. 1 in the period from 2005 to 2010 was carried out. Patients with concomitant interventions, such as operations on the aortic valve and ascending aorta, myocardial revascularization, rhythm restoration interventions were not included in the study.
The majority of patients were women ( n
=47; 84%), average age 55.9±8.2 years. The average NYHA functional class was 3.4±0.5. In 25 (45%) patients, long-term rhythm disturbances in the form of atrial fibrillation or atrial flutter were detected. 21 (38%) patients had a previous history of closed mitral commissurotomy. The left ventricular ejection fraction averaged 58.5±9.7%. The table shows the main clinical characteristics of patients before surgery.
Clinical characteristics of patients before surgery
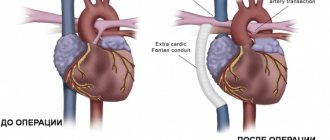
All patients underwent mitral valve replacement using standard techniques under conditions of artificial circulation, normothermia, cold blood cardioplegia, with cannulation of the ascending aorta and vena cava. In 50 (89%) patients a mechanical prosthesis was implanted, in 6 (11%) - a biological one. In 37 (66%) cases, tricuspid valve annuloplasty was performed: 7 patients underwent support ring repair, and 30 patients underwent DeVega annuloplasty. The average degree of tricuspid regurgitation before surgery was 0.8±0.8: in patients with annuloplasty - 0.9±0.9, without annuloplasty - 0.4±0.5 ( p
=0.029).
The average index of the diameter of the fibrous ring in patients was 18.6±2.4 mm/m2 (in patients with annuloplasty - 18.8±2.4 mm/m2, without annuloplasty - 18.2±2.4 mm/m2; p
=0.38); systolic pressure in the pulmonary artery - 42.7±12.3 mmHg. The decision to perform tricuspid valve repair and its variant was made by the operating surgeon.
Between November 2013 and January 2014, all patients underwent an examination, including examination by a cardiologist, electrocardiography, questionnaires, and echocardiography. The median follow-up period was 58.5 months (36–105 months). To assess right ventricular dysfunction, the echocardiographic protocol additionally included measurement of the amplitude of tricuspid annulus motion (TAPSE) and its peak systolic velocity (TAPSV) [8, 9].
Statistical processing of the data was carried out using the SPSS Statistics 17.0 program. To compare qualitative characteristics, Fisher's test or χ2 was used. When comparing quantitative characteristics, analysis of variance or Student's test was used. If the data did not conform to a normal distribution, Mann–Whitney analysis was used for comparison. To determine the relationship between characteristics, use the Spearman rank correlation method. Differences were considered statistically significant at p
<0,05.
Treatment
Drug treatment of tricuspid stenosis
Your doctor may recommend regular monitoring of your tricuspid valve disease, with or without predominant stenosis. Clinic visits during which medical examinations are performed may occur once a year or more frequently, depending on your doctor's orders. Diagnostic tests are repeated at certain intervals.
Medicines may also be prescribed by a doctor to relieve symptoms of the disease. Medicines include drugs to relieve symptoms of heart failure or control irregular heart rhythms.






![Rice. 1. Functioning of the glymphatic system of the brain (according to [11]) 1. Glymphatic system functioning (according to [11])](https://expert35.ru/wp-content/uploads/ris-1-funkcionirovanie-glimfaticheskoj-sistemy-mozga-po-11-fig-1-330x140.jpg)
