CIRCULATORY SYSTEM (circulatory system), a group of organs involved in blood circulation in the body.
The normal functioning of any animal body requires efficient blood circulation as it carries oxygen, nutrients, salts, hormones and other vital substances to all organs of the body. In addition, the circulatory system returns blood from the tissues to those organs, where it can be enriched with nutrients, as well as to the lungs, where it is saturated with oxygen and released from carbon dioxide (carbon dioxide). Finally, the blood must flow to a number of special organs, such as the liver and kidneys, which neutralize or eliminate metabolic waste products. The accumulation of these products can lead to chronic ill health and even death. Also on topic:
HUMAN ANATOMY
This article discusses the human circulatory system. (For information on circulatory systems in other species, see the article COMPARATIVE ANATOMY.)
Components of the circulatory system.
In its most general form, this transport system consists of a muscular four-chamber pump (heart) and many channels (vessels), the function of which is to deliver blood to all organs and tissues and its subsequent return to the heart and lungs. Based on the main components of this system, it is also called cardiovascular, or cardiovascular.
Also on topic:
COMPARATIVE ANATOMY
Blood vessels are divided into three main types: arteries, capillaries and veins. Arteries carry blood away from the heart. They branch into vessels of ever smaller diameter, through which blood flows to all parts of the body. Closer to the heart, the arteries have the largest diameter (about the size of a thumb); in the limbs they are the size of a pencil. In the parts of the body furthest from the heart, the blood vessels are so small that they can only be seen under a microscope. It is these microscopic vessels, capillaries, that supply cells with oxygen and nutrients. After their delivery, blood, loaded with metabolic waste products and carbon dioxide, is sent to the heart through a network of vessels called veins, and from the heart to the lungs, where gas exchange occurs, as a result of which the blood is freed from the carbon dioxide load and is saturated with oxygen.
Also on topic:
BLOOD
As it passes through the body and its organs, some of the liquid seeps through the walls of the capillaries into the tissues. This opalescent, plasma-like fluid is called lymph. The return of lymph to the general circulatory system is carried out through the third system of channels - the lymphatic tracts, which merge into large ducts that flow into the venous system in close proximity to the heart. (For a detailed description of lymph and lymphatic vessels, see the article LYMPHATIC SYSTEM.)
3. Symptoms and diagnosis
Pulmonary hemorrhage may appear suddenly or develop gradually from hemoptysis, but in any case it is accompanied by sallow pallor, cold hyperhidrosis, cyanotic discoloration of the skin of the extremities, a sharp decrease in blood pressure, tachycardia, tinnitus, dizziness, weakness, often anxious-panic disorganization of the psyche, disorders vision, convulsions, confusion with transition to deep fainting, stuporous state or agony.
Death usually occurs due to asphyxia and/or hypovolemic shock caused by rapid massive blood loss.
There is usually very little time left for diagnosis and taking emergency life-saving measures, and in such cases, much depends on the doctor’s ability to pay attention to the color of the blood, the nature of pulmonary wheezing, breathing patterns, heart murmurs, etc. An urgent consultation with a specialized specialist (gastroenterologist, parasitologist, oncologist, etc.) or instrumental examination (FEGDS, MRI, CT, radiography, bronchoscopy) is often necessary. Samples of biomaterial (sputum, blood, pus, etc.) are sent for laboratory biochemical, histological, microbiological analysis.
About our clinic Chistye Prudy metro station Medintercom page!
WORK OF THE CIRCULATORY SYSTEM
Pulmonary circulation.
It is convenient to begin describing the normal movement of blood throughout the body from the moment when it returns to the right half of the heart through two large veins. One of them, the superior vena cava, brings blood from the upper half of the body, and the second, the inferior vena cava, brings blood from the lower half. Blood from both veins enters the collecting compartment of the right side of the heart, the right atrium, where it mixes with blood brought by the coronary veins, which open into the right atrium through the coronary sinus. The coronary arteries and veins circulate the blood necessary for the functioning of the heart itself. The atrium fills, contracts, and pushes blood into the right ventricle, which contracts to force blood through the pulmonary arteries into the lungs. The constant flow of blood in this direction is maintained by the operation of two important valves. One of them, the tricuspid valve, located between the ventricle and the atrium, prevents the return of blood to the atrium, and the second, the pulmonary valve, closes when the ventricle relaxes and thereby prevents the return of blood from the pulmonary arteries. In the lungs, blood passes through the branches of the vessels, entering a network of thin capillaries that are in direct contact with the smallest air sacs - the alveoli. An exchange of gases occurs between the capillary blood and the alveoli, which completes the pulmonary phase of blood circulation, i.e. the phase of blood entering the lungs (see also RESPIRATORY ORGANS).
Systemic circulation.
From this moment the systemic phase of blood circulation begins, i.e. phase of blood transfer to all tissues of the body. Cleared of carbon dioxide and enriched with oxygen (oxygenated), blood returns to the heart through four pulmonary veins (two from each lung) and enters the left atrium at low pressure. The path of blood flow from the right ventricle of the heart to the lungs and return from them to the left atrium is the so-called. pulmonary circulation. The left atrium, filled with blood, contracts simultaneously with the right and pushes it into the massive left ventricle. The latter, when filled, contracts, sending blood under high pressure into the artery of the largest diameter - the aorta. All arterial branches supplying the tissues of the body depart from the aorta. Just like on the right side of the heart, there are two valves on the left. The bicuspid (mitral) valve directs blood flow into the aorta and prevents blood from returning to the ventricle. The entire path of blood from the left ventricle until it returns (through the superior and inferior vena cava) to the right atrium is designated as the systemic circulation.
Arteries.
In a healthy person, the diameter of the aorta is approximately 2.5 cm. This large vessel extends upward from the heart, forms an arch, and then descends through the chest into the abdominal cavity. Along the course of the aorta, all the large arteries that enter the systemic circulation branch off from it. The first two branches, extending from the aorta almost at the very heart, are the coronary arteries, which supply blood to the heart tissue. Apart from them, the ascending aorta (the first part of the arch) does not give off branches. However, at the top of the arch, three important vessels branch off from it. The first, the innominate artery, immediately divides into the right carotid artery, which supplies blood to the right side of the head and brain, and the right subclavian artery, which passes under the collarbone into the right arm. The second branch from the aortic arch is the left carotid artery, the third is the left subclavian artery; These branches carry blood to the head, neck and left arm.
From the aortic arch begins the descending aorta, which supplies blood to the organs of the chest, and then enters the abdominal cavity through an opening in the diaphragm. Separated from the abdominal aorta are two renal arteries that supply the kidneys, as well as the abdominal trunk with the superior and inferior mesenteric arteries, which extend to the intestines, spleen and liver. The aorta then divides into two iliac arteries, which supply blood to the pelvic organs. In the groin area, the iliac arteries become femoral; the latter, going down the thighs, at the level of the knee joint pass into the popliteal arteries. Each of them, in turn, is divided into three arteries - the anterior tibial, posterior tibial and peroneal arteries, which nourish the tissues of the legs and feet.
Along the entire length of the bloodstream, the arteries become smaller and smaller as they branch, and finally acquire a caliber that is only several times larger than the size of the blood cells they contain. These vessels are called arterioles; as they continue to divide, they form a diffuse network of vessels (capillaries), the diameter of which is approximately equal to the diameter of a red blood cell (7 μm).
Structure of arteries.
Although large and small arteries differ somewhat in their structure, the walls of both consist of three layers. The outer layer (adventitia) is a relatively loose layer of fibrous, elastic connective tissue; the smallest blood vessels (the so-called vascular vessels) pass through it, feeding the vascular wall, as well as branches of the autonomic nervous system that regulate the lumen of the vessel. The middle layer (media) consists of elastic tissue and smooth muscles, which provide elasticity and contractility of the vascular wall. These properties are essential for regulating blood flow and maintaining normal blood pressure under changing physiological conditions. Typically, the walls of large vessels, such as the aorta, contain more elastic tissue than the walls of smaller arteries, which are predominantly muscle tissue. Based on this tissue feature, arteries are divided into elastic and muscular. The thickness of the inner layer (intima) rarely exceeds the diameter of several cells; It is this layer, lined with endothelium, that gives the inner surface of the vessel a smoothness that facilitates blood flow. Through it, nutrients flow to the deep layers of the media.
As the diameter of the arteries decreases, the walls become thinner and the three layers become less distinguishable until—at the arteriolar level—they contain mostly spiral muscle fibers, some elastic tissue, and an inner lining of endothelial cells.
Capillaries.
Finally, the arterioles imperceptibly turn into capillaries, the walls of which are lined only with endothelium. Although these tiny tubes contain less than 5% of the volume of circulating blood, they are extremely important. The capillaries form an intermediate system between the arterioles and venules, and their networks are so dense and wide that no part of the body can be pierced without piercing a huge number of them. It is in these networks that, under the influence of osmotic forces, oxygen and nutrients are transferred to individual cells of the body, and in return, products of cellular metabolism enter the blood.
In addition, this network (the so-called capillary bed) plays a critical role in regulating and maintaining body temperature. The constancy of the internal environment (homeostasis) of the human body depends on maintaining body temperature within narrow limits of normal (36.8–37°). Normally, blood from the arterioles enters the venules through the capillary bed, but in cold conditions the capillaries close and blood flow decreases, primarily in the skin; in this case, blood from the arterioles enters the venules, bypassing many branches of the capillary bed (bypass). On the contrary, when there is a need for heat transfer, for example in the tropics, all capillaries open and skin blood flow increases, which promotes heat loss and maintains normal body temperature. This mechanism exists in all warm-blooded animals.
Vienna.
On the opposite side of the capillary bed, the vessels merge into numerous small channels, venules, which are comparable in size to arterioles. They continue to connect to form larger veins that carry blood from all parts of the body back to the heart. Constant blood flow in this direction is facilitated by a system of valves found in most veins. Venous pressure, unlike pressure in the arteries, does not directly depend on the tension of the muscles of the vascular wall, so blood flow in the desired direction is determined mainly by other factors: the pushing force created by the arterial pressure of the systemic circulation; the “suction” effect of negative pressure that occurs in the chest during inhalation; the pumping action of the muscles of the limbs, which, during normal contractions, push venous blood to the heart.
The walls of veins are similar in structure to arterial ones in that they also consist of three layers, however, much less pronounced. For the movement of blood through the veins, which occurs practically without pulsation and at relatively low pressure, it does not require such thick and elastic walls as those of the arteries. Another important difference between veins and arteries is the presence of valves in them, which maintain blood flow in one direction at low pressure. The valves are found in greatest numbers in the veins of the extremities, where muscle contractions play a particularly important role in moving blood back to the heart; large veins, such as the cava, portal and iliac veins, lack valves.
On their way to the heart, the veins collect blood flowing from the gastrointestinal tract through the portal vein, from the liver through the hepatic veins, from the kidneys through the renal veins, and from the upper extremities through the subclavian veins. Two vena cavae form near the heart, through which blood enters the right atrium.
The vessels of the pulmonary circulation (pulmonary) resemble the vessels of the systemic circulation, with the only exception that they lack valves, and the walls of both arteries and veins are much thinner. In contrast to the systemic circulation, venous, non-oxygenated blood flows through the pulmonary arteries into the lungs, and arterial, i.e., flows through the pulmonary veins. saturated with oxygen. The terms “arteries” and “veins” refer to the direction of blood movement in the vessels - from the heart or to the heart, and not to the type of blood they contain.
Auxiliary organs.
A number of organs perform functions that complement the work of the circulatory system. The spleen, liver and kidneys are most closely associated with it.
Spleen.
As red blood cells (erythrocytes) pass through the circulatory system repeatedly, they are damaged. Such “waste” cells are removed from the blood in many ways, but the main role here belongs to the spleen. The spleen not only destroys damaged red blood cells, but also produces lymphocytes (which are white blood cells). In lower vertebrates, the spleen also plays the role of a reservoir of red blood cells, but in humans this function is weakly expressed. See also SPLEEN.
Liver.
To carry out its more than 500 functions, the liver needs a good blood supply. Therefore, it occupies an important place in the circulatory system and is provided by its own vascular system, which is called the portal system. A number of liver functions are directly related to the blood, such as removing waste red blood cells from the blood, producing clotting factors, and regulating blood sugar levels by storing excess sugar in the form of glycogen. See also LIVER.
Kidneys.
The kidneys receive approximately 25% of the total blood volume ejected by the heart every minute. Their special role is to cleanse the blood of nitrogen-containing waste. When this function is disrupted, a dangerous condition develops - uremia. Loss of blood supply or kidney damage causes a sharp rise in blood pressure, which, if left untreated, can lead to premature death from heart failure or stroke. See also KIDNEYS; UREMIA.
BLOOD (ARTERIAL) PRESSURE
With each contraction of the left ventricle of the heart, the arteries fill with blood and stretch. This phase of the cardiac cycle is called ventricular systole, and the phase of ventricular relaxation is called diastole. During diastole, however, the elastic forces of large blood vessels come into play, maintaining blood pressure and preventing the flow of blood to various parts of the body from being interrupted. The change of systole (contraction) and diastole (relaxation) gives the blood flow in the arteries a pulsating character. The pulse can be found in any major artery, but is usually felt in the wrist. In adults, the pulse rate is usually 68–88, and in children – 80–100 beats per minute. The existence of arterial pulsation is also evidenced by the fact that when an artery is cut, bright red blood flows out in spurts, and when a vein is cut, bluish (due to lower oxygen content) blood flows evenly, without visible tremors.
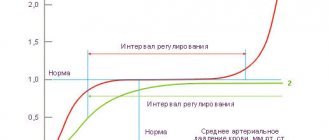
To ensure proper blood supply to all parts of the body during both phases of the cardiac cycle, a certain level of blood pressure is needed. Although this value varies widely even in healthy people, normal blood pressure averages 100–150 mmHg. during systole and 60–90 mm Hg. during diastole. The difference between these indicators is called pulse pressure. For example, a person with a blood pressure of 140/90 mmHg. pulse pressure is 50 mm Hg. Another indicator, mean arterial pressure, can be approximated by averaging systolic and diastolic pressure or adding half the pulse pressure to diastolic pressure.
Normal blood pressure is determined, maintained and regulated by many factors, the main ones being the strength of heart contraction, the elastic recoil of the artery walls, the volume of blood in the arteries and the resistance of small arteries (muscular type) and arterioles to the movement of blood. All these factors together determine the lateral pressure on the elastic walls of the arteries. It can be measured very accurately by using a special electronic probe inserted into the artery and recording the results on paper. Such devices, however, are quite expensive and are used only for special studies, and doctors, as a rule, make indirect measurements using the so-called. sphygmomanometer (tonometer).
A sphygmomanometer consists of a cuff that is wrapped around the limb where the measurement is made, and a recording device, which can be a column of mercury or a simple aneroid manometer. Typically, the cuff is wrapped tightly around the arm above the elbow and inflated until there is no pulse at the wrist. The brachial artery is located at the level of the elbow and a stethoscope is placed over it, after which the air is slowly released from the cuff. When the pressure in the cuff drops to a level at which blood flow through the artery resumes, a sound audible with a stethoscope is produced. The readings of the measuring device at the moment of the appearance of this first sound (tone) correspond to the level of systolic blood pressure. With further release of air from the cuff, the nature of the sound changes significantly or it disappears completely. This moment corresponds to the level of diastolic pressure.
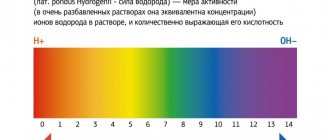
In a healthy person, blood pressure fluctuates throughout the day depending on the emotional state, stress, sleep and many other physical and mental factors. These fluctuations reflect certain shifts in the normally existing delicate balance, which is maintained both by nerve impulses coming from the centers of the brain through the sympathetic nervous system, and by changes in the chemical composition of the blood, which have a direct or indirect regulatory effect on the blood vessels. With strong emotional stress, the sympathetic nerves cause a narrowing of small muscular arteries, which leads to an increase in blood pressure and pulse rate. Of even greater importance is the chemical balance, the influence of which is mediated not only by the brain centers, but also by individual nerve plexuses associated with the aorta and carotid arteries. The sensitivity of this chemical regulation is illustrated, for example, by the effect of carbon dioxide accumulation in the blood. As its level increases, the acidity of the blood increases; this both directly and indirectly causes contraction of the walls of peripheral arteries, which is accompanied by an increase in blood pressure. At the same time, the heart rate increases, but the blood vessels of the brain paradoxically expand. The combination of these physiological reactions ensures a stable supply of oxygen to the brain by increasing the volume of incoming blood.
It is the fine regulation of blood pressure that allows you to quickly change the horizontal position of the body to a vertical one without significant movement of blood to the lower extremities, which could cause fainting due to insufficient blood supply to the brain. In such cases, the walls of the peripheral arteries contract and oxygenated blood is directed primarily to vital organs. Vasomotor (vasomotor) mechanisms are even more important for animals such as the giraffe, whose brain, when it raises its head after drinking, moves up almost 4 m in a few seconds. A similar decrease in blood content in the vessels of the skin, digestive tract and liver occurs in moments of stress, emotional distress, shock and trauma, which helps provide more oxygen and nutrients to the brain, heart and muscles.
Such fluctuations in blood pressure are normal, but changes are also observed in a number of pathological conditions. In heart failure, the force of contraction of the heart muscle may decrease so much that blood pressure becomes too low (hypotension). Likewise, loss of blood or other fluids due to a severe burn or bleeding can cause both systolic and diastolic blood pressure to drop to dangerous levels. With some congenital heart defects (for example, patent ductus arteriosus) and a number of lesions of the valvular apparatus of the heart (for example, aortic valve insufficiency), peripheral resistance drops sharply. In such cases, systolic pressure may remain normal, but diastolic pressure decreases significantly, which means an increase in pulse pressure.
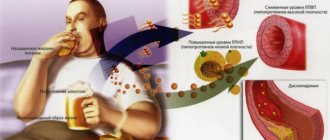
Some diseases are accompanied not by a decrease, but, on the contrary, by an increase in blood pressure (arterial hypertension). Older people whose blood vessels lose elasticity and become stiffer usually develop a benign form of arterial hypertension. In these cases, due to a decrease in vascular distensibility, systolic blood pressure reaches a high level, while diastolic blood pressure remains almost normal. In some diseases of the kidneys and adrenal glands, very large amounts of hormones such as catecholamines and renin enter the blood. These substances cause constriction of blood vessels and, therefore, hypertension. With both this and other forms of increased blood pressure, the causes of which are less understood, the activity of the sympathetic nervous system also increases, which further enhances the contraction of the vascular walls. Long-term arterial hypertension, if left untreated, leads to accelerated development of atherosclerosis, as well as an increased incidence of renal diseases, heart failure and strokes. See also ARTERIAL HYPERTENSION.
Regulating blood pressure in the body and maintaining the necessary blood supply to organs best allows us to understand the colossal complexity of the organization and operation of the circulatory system. This truly remarkable transport system is a real “lifeline” of the body, since insufficient blood supply to any vital organ, primarily the brain, for at least a few minutes leads to irreversible damage and even death.
BLOOD VESSEL DISEASES
Diseases of blood vessels (vascular diseases) are conveniently considered in accordance with the type of vessels in which pathological changes develop. Stretching of the walls of blood vessels or the heart itself leads to the formation of aneurysms (sac-like protrusions). This is usually a consequence of the development of scar tissue in a number of diseases of the coronary vessels, syphilitic lesions or hypertension. Aneurysm of the aorta or ventricles of the heart is the most serious complication of cardiovascular diseases; it may rupture spontaneously, causing fatal bleeding.
Aorta.
The largest artery, the aorta, must accommodate the blood ejected under pressure from the heart and, due to its elasticity, move it to smaller arteries. Infectious (most often syphilitic) and arteriosclerotic processes can develop in the aorta; rupture of the aorta due to injury or congenital weakness of its walls is also possible. High blood pressure often leads to chronic enlargement of the aorta. However, aortic diseases are less important than heart diseases. Its most severe lesions are extensive atherosclerosis and syphilitic aortitis.
Atherosclerosis.
Aortic atherosclerosis is a form of simple arteriosclerosis of the inner lining of the aorta (intima) with granular (atheromatous) fatty deposits in this layer and under it. One of the serious complications of this disease of the aorta and its main branches (innominate, iliac, carotid and renal arteries) is the formation of blood clots in the inner layer, which can obstruct blood flow in these vessels and lead to a catastrophic disruption of the blood supply to the brain, legs and kidneys. This kind of obstructive (obstructing blood flow) lesions of some large vessels can be eliminated surgically (vascular surgery).
Syphilitic aortitis.
A decrease in the prevalence of syphilis itself makes the inflammation of the aorta it causes less common. It manifests itself approximately 20 years after infection and is accompanied by significant dilation of the aorta with the formation of aneurysms or the spread of infection to the aortic valve, which leads to its insufficiency (aortic regurgitation) and overload of the left ventricle of the heart. Narrowing of the mouth of the coronary arteries is also possible. Any of these conditions can lead to death, sometimes very quickly. The age at which aortitis and its complications manifest itself ranges from 40 to 55 years; the disease is more common in men.
Arteriosclerosis
of the aorta, accompanied by loss of elasticity of its walls, is characterized by damage not only to the intima (as in atherosclerosis), but also to the muscular layer of the vessel. This is a disease of old age, and as the population lives longer, it is becoming more common. Loss of elasticity reduces the efficiency of blood flow, which in itself can lead to aneurysm-like dilatation of the aorta and even rupture, especially in the abdominal region. Nowadays, this condition can sometimes be treated with surgery (see also ANEURYSM).
Pulmonary artery.
Lesions of the pulmonary artery and its two main branches are few. Arteriosclerotic changes sometimes occur in these arteries, and congenital defects also occur. The two most important changes are: 1) dilation of the pulmonary artery due to increased pressure in it due to some obstruction of blood flow in the lungs or on the path of blood into the left atrium and 2) blockage (embolism) of one of its main branches due to the passage of a blood clot from inflamed large veins of the leg (phlebitis) through the right half of the heart, which is a common cause of sudden death.
Arteries of medium caliber.
The most common disease of the middle arteries is arteriosclerosis. When it develops in the coronary arteries of the heart, the inner layer of the vessel (intima) is affected, which can lead to complete blockage of the artery. Depending on the degree of damage and the general condition of the patient, either balloon angioplasty or coronary bypass surgery is performed. In balloon angioplasty, a catheter with a balloon at the end is inserted into the affected artery; inflation of the balloon leads to flattening of deposits along the arterial wall and expansion of the lumen of the vessel. In bypass surgery, a section of a vessel is cut out from another part of the body and sewn into the coronary artery, bypassing the narrowed area, restoring normal blood flow.
When the arteries of the legs and arms are damaged, the middle, muscular, layer of blood vessels (media) thickens, which leads to their thickening and curvature. Damage to these arteries has relatively less severe consequences.
Arterioles.
Damage to arterioles creates an obstruction to free blood flow and leads to increased blood pressure. However, even before the arterioles become sclerotic, spasms of unknown origin may occur, which is a common cause of hypertension.
Vienna.
Vein diseases are very common. The most common are varicose veins of the lower extremities; this condition develops under the influence of gravity due to obesity or pregnancy, and sometimes due to inflammation. In this case, the function of the venous valves is disrupted, the veins stretch and fill with blood, which is accompanied by swelling of the legs, pain and even ulcerations. Various surgical procedures are used for treatment. Alleviation of the disease is facilitated by training the lower leg muscles and reducing body weight. Another pathological process - inflammation of the veins (phlebitis) - is also most often observed in the legs. In this case, there are obstructions to blood flow with disruption of local circulation, but the main danger of phlebitis is the detachment of small blood clots (emboli), which can pass through the heart and cause circulatory arrest in the lungs. This condition, called pulmonary embolism, is very serious and often fatal. Damage to large veins is much less dangerous and is much less common.
4.Treatment
Obviously, the strategy and tactics of care are determined by the diagnosed (or most likely, taking into account clinical data) causes of bleeding.
It is not possible to list or describe at least the main options for conservative and/or surgical treatment. However, in all cases, the primary task is hemostasis (stopping bleeding), stabilization of basic vital signs (blood pressure, heart rate, respiratory rate), elimination of the root cause and/or relief of exacerbation of the underlying disease, blood replacement according to indications, decisive measures to prevent severe complications, the likelihood of which given these conditions circumstances is very high.