The blood of each person has its own characteristics and characteristics. It is determined by specific proteins - antigens found on the surface of red blood cells, as well as natural antibodies to them contained in plasma.
There are many possible combinations of antigens. Nowadays, the AB0 and Rh systems are used to classify blood. Based on them, four varieties are distinguished: 0, A, B, AB, or in other words - I, II, II, IV. In turn, each of them can be Rh-positive or Rh-negative. Many may have a question about how blood type and Rh factor are inherited.
These characteristics are inherited from parents and are formed in the mother's womb. Antigens on the surface of red cells appear by two to three months, and at the time of birth they are already accurately determined. From about three months, natural antibodies to antigens are detected in the serum, and only by ten years do they reach their maximum titer.
Neither the group nor the Rh factor changes during life, their inheritance is in no way connected with each other, and probability calculations are made separately.
General principles of inheritance of characters.
Simply put, every trait in the body (hair color, eye color, blood type, Rh factor) is encoded by two genes.
In reality, the number of genes that determine the trait is much greater. For each trait, the child receives one gene from the mother, another from the father. In genetics, dominant and recessive genes are distinguished. The dominant gene is designated by a capital letter of the Latin alphabet, and in its presence the recessive gene, as a rule, does not manifest its properties. A recessive gene is indicated by a capital letter of the Latin alphabet. If for some trait an organism contains two identical genes (two recessive or two dominant), then it is called homozygous for this trait. If an organism contains one dominant and one recessive gene, then it is called heterozygous for this trait, and at the same time those properties of the trait that are encoded by the dominant gene are manifested. For example: A is a dominant gene that determines brown eye color and A is a recessive gene that determines blue eye color
Possible genotype options: AA - homozygote, brown eyes Aa - heterozygote, brown eyes aa - homozygote, blue eyes
Example 1:
wife AA - homozygous, brown eyes, both genes are dominant; husband AA - homozygous, blue eyes, both genes are recessive
When germ cells (egg and sperm) are formed, one gene goes into each germ cell (gamete), i.e. in this case, the female body forms two gametes containing one dominant gene each, and the male body forms two gametes containing one recessive gene each. When germ cells merge, the embryo receives one maternal and one paternal gene for this trait.
wife AA + husband aa Gametes: A A a a Child: Aa Aa Aa Aa
Thus, in this situation, 100% of the children will have brown eyes and be heterozygotes for this trait.
Example 2:
wife Aa - heterozygote, brown eyes husband Aa - heterozygote, brown eyes wife Aa + husband Aa gametes: A a A a child: AA, Aa, Aa, aa
In this case, the probability of having children with brown eyes (homozygotes) is 25%, heterozygotes are 50% with brown eyes, and blue eyes (homozygotes) are 25%.
Example 3:
wife Aa - heterozygote, brown eyes husband aa - homozygote, blue eyes Wife Aa + husband aa Gametes: A a a a Child: Aa, Aa, aa, aa
In this case, 50% of children have brown eyes and are heterozygotes and 50% have blue eyes (homozygotes)
Principle of inheritance
At the moment, scientists know the principle of plasma inheritance and the Rh factor. This has been proven in the last century. Expectant parents are constantly worried about inheritance. After all, there have been cases when a child’s plasma does not match the paternal and maternal plasma.
Blood
According to scientists, the principle of inheritance is complex. The baby will inherit the type of plasma of the parents, but this is far from true. You can easily find out the child's blood type by the blood type of the parents. As a result, peculiar patterns are obtained that are easily explained from a scientific point of view.
- Negative Rh factor during pregnancy consequences
Blood types of parents and children
The inheritance of plasma in the body of a born child is controlled by an autosomal gene. It contains 2 alleles. The baby receives one from each parent.
Patterns of inheritance of blood group and Rh factor.
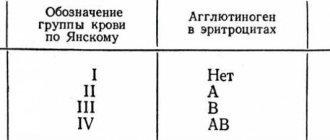
Inheritance of blood type is controlled by an autosomal gene. The locus of this gene is designated by the letter I, and its three alleles by the letters A, B and 0. Alleles A and B are equally dominant, and allele 0 is recessive to both of them. There are four blood types. The following genotypes correspond to them: First (I) 00 Second (II) AA; A0 Third (III) BB; B0 Fourth (IV) AB
Example 1:
wife has the first blood group (00) husband has the second blood group and is homozygous (AA) wife 00 + husband AA gametes: 0 0 A A child: A0 A0 A0 A0
All children have a second blood group and are heterozygotes for this trait.
Example 2:
wife has the first blood group (00) husband has the second blood group and is a heterozygote (A0) wife 00 + husband A0 gametes: 0 0 A 0 child: A0 A0 00 00
In a given family, in 50% of cases it is possible to have a child with a second blood group, and in 50% of cases the child’s blood type will be first.
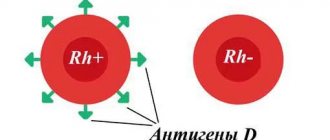
Inheritance of the Rh factor is encoded by three pairs of genes and occurs independently of the inheritance of blood type. The most significant gene is designated by the Latin letter D. It can be dominant - D, or recessive - d. The genotype of a Rh-positive person can be homozygous - DD, or heterozygous - Dd. The genotype of a Rh negative person may be dd.
Example 1:
wife has a negative Rh factor (dd) husband has a positive Rh factor and is a heterozygote (Dd) wife dd + husband Dd gametes: dd D d child: Dd Dd dd dd
In a given family, the probability of having a Rh-positive child is 50% and the probability of having a Rh-negative child is also 50%.
Example 2:
wife has a negative Rh factor (dd) husband has a positive Rh factor and is homozygous for this trait (DD) wife dd + husband DD gametes: dd DD child: Dd Dd Dd Dd
In this family, the probability of having a Rh-positive child is 100%.
The most basic thing about the concept of blood group
The child's blood depends on the parents and is inherited with the so-called ABO gene, which is located on chromosome 9. The following table will show how likely it is that a group will be taken from its parents.
| Parents' blood types | Heritable blood type in a child as a percentage | ||||
| I | II | III | IV | ||
| I and I | 100% | — | — | — | — |
| I and II | 50% | 50% | — | — | |
| I and III | 50% | — | 50% | — | |
| I and IV | — | 50% | — | 50% | |
| II and II | 25% | 75% | — | — | |
| II and III | 25% | 25% | 25% | 25% | |
| II and IV | — | 50% | 25% | 25% | |
| III and III | 25% | — | 75% | — | |
| III and IV | — | 25% | 50% | 25% | |
| IV and IV | — | 25% | 25% | 50% | |
With 100 percent probability we can say which blood type will be passed on to the baby if they both have the first.
Features of the course of pregnancy with Rh factor incompatibility. Rhesus conflict.
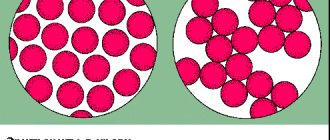
Hemolytic disease of the fetus and newborn is a condition that occurs as a result of incompatibility of the blood of mother and fetus for certain antigens. Most often, hemolytic disease of the newborn develops due to Rh conflict. In this case, the pregnant woman has Rh-negative blood, and the fetus has Rh-positive blood. During pregnancy, the Rh factor with the red blood cells of the Rh-positive fetus enters the blood of the Rh-negative mother and causes the formation of antibodies to the Rh factor in her blood (harmless to her, but causing the destruction of the fetal red blood cells). The breakdown of red blood cells leads to damage to the liver, kidneys, brain of the fetus, and the development of hemolytic disease of the fetus and newborn. In most cases, the disease develops quickly after birth, which is facilitated by the entry of a large number of antibodies into the baby’s blood when the integrity of the placental vessels is disrupted.
Less commonly, hemolytic disease of the newborn is caused by group incompatibility of the blood of mother and fetus (according to the AB0 system). In this case, due to agglutinogen (A or B), present in the fetal red blood cells but absent in the mother, antibodies to the fetal red blood cells are formed in the maternal blood. Most often, immune incompatibility manifests itself when the mother has blood group I, and the fetus has blood group II, and less often, blood group III.
The process of immunization of a pregnant woman begins with the formation of antigens in the red blood cells of the fetus. Since antigens of the Rh system are contained in the blood of the fetus from the 9-10th week of pregnancy, and group antigens - from the 5-6th week, in some cases early sensitization of the mother’s body is possible. The penetration of antigens into the maternal bloodstream is facilitated by infectious factors that increase the permeability of the placenta, minor injuries, hemorrhages and other damage to the placenta. As a rule, the first pregnancy in an Rh-negative woman, in the absence of previous sensitization of the body, proceeds without complications. Sensitization of the body of a Rh-negative woman is possible through transfusions of incompatible blood (carried out even in early childhood), during pregnancy and childbirth (if the fetus has Rh-positive blood), after abortions, miscarriages, and operations for ectopic pregnancy. According to the literature, after the first pregnancy, immunization occurs in 10% of women. If a woman with Rh-negative blood avoided Rh immunization after her first pregnancy, then during a subsequent pregnancy with an Rh-positive fetus, the probability of immunization again is 10%. Therefore, after any termination of pregnancy in a woman with Rh-negative blood, it is necessary to administer anti-Rhesus immunoglobulin for prophylactic purposes. During pregnancy, in a woman with Rh-negative blood, it is necessary to determine the titer of Rh antibodies in the blood over time.
All about rhesus
Each cell contains 50 different types of proteins. The Rh factor is a protein D located in the membrane of blood cells. It has antigenic characteristics.
- Blood type of parents and children - how to determine what the child will have
The Rhesus determination system has five more different antigens - d, C, c, E, e. Thanks to combinations of these antigens, the Rh genotype is revealed, which consists of 18 combinations.
Each antigen is subdivided into several more, with different strengths.
The Rh factor system carries rare genotypes. Rh factor zero is extremely rare. There are no antibodies in the fluid.
Positive
In a situation where a person’s medical record shows a positive sign, this means that he has antigen D. In blood group tables, the international sign is Rh(+) and is indicated on the cover of the card.
About 85% of the world's population are carriers of positive Rhesus, and among Asian citizens these figures can be 93%.
Negative
This type of Rhesus does not affect human health in any way. This is a feature that is taken into account during blood transfusion (transfusion) or during gestation. It is considered negative when a person does not have antigen D.
Question 2:
I have a negative Rh factor. I recently had an abortion. Will I be able to have children? Is there a chance that the baby will be sick during the next pregnancy?
Answer
: The presence of a negative Rh factor does not directly affect conception. During an abortion (if it was performed at 9-10 weeks of pregnancy), there was a possibility of sensitization of the body to the Rh factor. Before a planned pregnancy, it is advisable to do a blood test for the presence of antibodies to the Rh factor.
What can a child inherit?
The principles of transmission of hereditary characteristics from parents to children were formulated more than a century and a half ago by the Austrian biologist, monk Gregor Johann Mendel. Mendel's experiments were understood and recognized only half a century after his death. Thus, classical genetics appeared at the beginning of the 20th century, Dmitry Okunev, a therapist and senior medical consultant at the Teledoctor24 service, tells Izvestia.
“Despite this, today parents are still concerned about the same questions: who will the baby look like, why did he become the owner of wonderful curls or a square chin. At this point, it is appropriate to recall that brown eye color and the gap between the front teeth are caused by a dominant gene, and the gene for straight hair is recessive, explains the doctor.
Blood for blood
Photo: Depositphotos/Paha_L
Pathogenic engineering: Izvestia found a patent for an “invisible” assembly of the genome of viruses
This method makes it possible to discreetly modify SARS-like microorganisms
According to him, recently in Russia there has been a steady increase in diseases transmitted by inheritance. Approximately 35–40 children suffer from them per thousand newborns.
— If we talk about the characteristics of hereditary diseases, then daughters are passed on from their mothers not only a tendency to be overweight and the entire range of characteristics of the monthly cycle, but even such a formidable disease as migraine (associated with the level of female sex hormones), depressive states, eye disease glaucoma and osteoporosis , metabolic disease. At the same time, the main parental figure for the child remains the maternal grandmother,” says Izvestia’s interlocutor.
On the paternal side, boys are transmitted the characteristics of the functioning of the male reproductive system, the degree of baldness and testosterone levels. In addition, heart and dental diseases can be transmitted to the child.
Question 3:
What dose of anti-Rhesus immunoglobulin and in what time frame is administered to a woman with Rh-negative blood after childbirth? Is it true that the administered dose of the drug should be increased after a caesarean section?
Answer
: Women with Rh-negative blood after childbirth are given anti-Rhesus immunoglobulin in an amount of 1-1.5 ml (200-300 µg) no later than 24-48 hours after birth for prophylactic purposes. During surgical interventions, transplacental bleeding may increase, and therefore the administered dose of anti-Rhesus immunoglobulin is increased by 1.5 times.