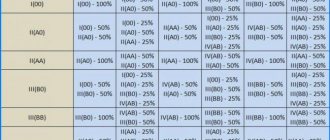
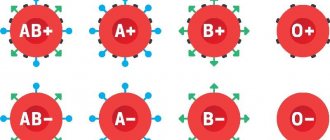
Nowadays, human blood is classified according to the ABO system and the Rh factor. According to this classification, four groups are distinguished: first (0), second (A), third (B), fourth (AB). Each of them can be Rh positive or Rh negative, which means there are 8 types of blood. The question may arise as to which one is the best. Some blood can be considered better than others only if its owner can always quickly find a donor in case of significant blood loss. Thus, we can conclude that the best group is the most common.
What blood is most common?
According to statistics, about half of all inhabitants of the planet have blood of the first group, about 40% are carriers of the second, approximately 8% of the population have the third group, and only 2% of people have the fourth. The vast majority (85%) are owners of Rh-positive blood, and only 15% do not have a specific protein on the surface of red cells - the Rh factor. From this we can conclude that the best group is I positive, and this means that such blood can always be found, unlike the fourth negative.
General principles of inheritance of characters.
Simply put, every trait in the body (hair color, eye color, blood type, Rh factor) is encoded by two genes.
In reality, the number of genes that determine the trait is much greater. For each trait, the child receives one gene from the mother, another from the father. In genetics, dominant and recessive genes are distinguished. The dominant gene is designated by a capital letter of the Latin alphabet, and in its presence the recessive gene, as a rule, does not manifest its properties. A recessive gene is indicated by a capital letter of the Latin alphabet. If for some trait an organism contains two identical genes (two recessive or two dominant), then it is called homozygous for this trait. If an organism contains one dominant and one recessive gene, then it is called heterozygous for this trait, and at the same time those properties of the trait that are encoded by the dominant gene are manifested. For example: A is a dominant gene that determines brown eye color and A is a recessive gene that determines blue eye color
Possible genotype options: AA - homozygote, brown eyes Aa - heterozygote, brown eyes aa - homozygote, blue eyes
Example 1:
wife AA - homozygous, brown eyes, both genes are dominant; husband AA - homozygous, blue eyes, both genes are recessive
When germ cells (egg and sperm) are formed, one gene goes into each germ cell (gamete), i.e. in this case, the female body forms two gametes containing one dominant gene each, and the male body forms two gametes containing one recessive gene each. When germ cells merge, the embryo receives one maternal and one paternal gene for this trait.
wife AA + husband aa Gametes: A A a a Child: Aa Aa Aa Aa
Thus, in this situation, 100% of the children will have brown eyes and be heterozygotes for this trait.
Example 2:
wife Aa - heterozygote, brown eyes husband Aa - heterozygote, brown eyes wife Aa + husband Aa gametes: A a A a child: AA, Aa, Aa, aa
In this case, the probability of having children with brown eyes (homozygotes) is 25%, heterozygotes are 50% with brown eyes, and blue eyes (homozygotes) are 25%.
Example 3:
wife Aa - heterozygote, brown eyes husband aa - homozygote, blue eyes Wife Aa + husband aa Gametes: A a a a Child: Aa, Aa, aa, aa
In this case, 50% of children have brown eyes and are heterozygotes and 50% have blue eyes (homozygotes)
The best one is universal?
Group 0 (first) blood is called universal because it is believed that it can be transfused to everyone. The fact is that it does not have antigens A and B on red blood cells, which means that the recipient’s body will not begin to produce antibodies against them. Thus, the first group can be considered the best, since its carrier can save any person in case of blood loss.
On the other hand, AB can be transfused only to owners of the same one, and to no one else. At the same time, anyone can become a donor for a person with IV, since AB blood plasma does not contain antibodies to antigens A and B.
You should know that such compatibility exists only theoretically. In modern conditions, it is forbidden to transfuse another group and with a different rhesus. The donor and recipient must have the same blood in both respects. An exception to the rules can be made only in case of urgent need.
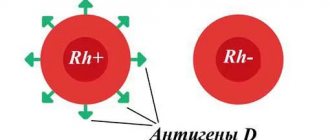
Rhesus system
Levine and Stetson discovered Rh antigens in 1939. Scientists studied the reasons for the development of hemolytic reactions in women in labor during transfusions of husbands' erythrocytes identical in the AB0, MN and P systems. A year later, Landsteiner and Wiener produced antibodies by immunizing rabbits with red blood cells from rhesus monkeys. The antibodies are called anti-RH antibodies. The resulting agglutinins entered into an agglutination reaction with the erythrocytes of rhesus monkeys and with the erythrocytes of 85% of New York citizens of the white race. The antigen that caused the formation of antibodies was called RH factor (D factor).
The Rhesus system combines 45 antigens. Agglutinogens are inherited and remain unchanged throughout life. Immunogenicity decreases in the following order: D > c > E > C > e. Each agglutinogen is encoded by one of two closely related genes: RHD is responsible for the production of the D antigen, RHCE is responsible for the production of the Cc and Ee antigens. Rh-positive donors are considered individuals with D, C or E antigens on the surface of red blood cells. In the absence of the above agglutinogens, donors are considered Rh negative.
In rare cases, human red blood cells do not contain any Rh antigen. The phenotype is designated RhNULL. The Xro gene in this case is presented in homozygous form and suppresses the production of all antigens. Holders of the RhNULL phenotype do not exhibit agglutinogenic activity, but have the ability to transmit antigens by inheritance.
Among Europeans, the frequency of Rh D antigen-positive individuals is 85%. There are usually about 10,000 – 30,000 D molecules located on the membrane of red blood cells. There are two special types of D-positive individuals: Du (weak) and Dpartial (partial). The immune system of Du and Dpartial is capable of producing anti-D antibodies.
Weak antigen occurs in 1.5% of Rh-positive individuals and is characterized by a low number (100–500) of D molecules on the membrane. Is immunogenic for Rh-negative individuals. In this case, transfusion of D-positive erythrocytes to patients with weak D may cause sensitization of the donor’s blood cells. Erythrocytes with Du are weakly agglutinated or do not at all enter into a direct agglutination reaction with complete anti-Rh antibodies. Determination of Rh status is carried out using an indirect antiglobulin test. Du carriers are considered Rh-positive donors and Rh-negative recipients.
Partial D is deficient in one or more epitopes of a protein molecule. The immune system of people with Dpartial is capable of producing antibodies to the missing epitopes. Among partial antigen carriers, seven groups of individuals are distinguished. The DVI carriage (only epitope Z is present) has the greatest clinical significance: owners of this category produce antibodies to the unchanged antigen and to partial antigens DI - DV, DVII. The technique for detecting the Rh factor DVI consists in the sequential use of two diagnostic kits: monoclonal IgM anti-D antibodies (coliclone Anti-D-Super or Anti-D IgM) and polyclonal or monoclonal IgG antibodies anti-D (standard universal reagent or coliclone Anti-D D). A negative reaction result in the first and a positive result in the second stage of the study indicates the detection of DVI. Typically, the DVI category corresponds to the CcDee genotype. Pregnant women with DVI who carry a fetus with complete D are prescribed anti-Rhesus immunoglobulin.
Antibodies against Rh antigens are immune. They arise due to isosensitization. Specificity is determined by the antigens that provoke the formation of antibodies. Complete and incomplete antibodies are isolated.
Complete are IgM antibodies. They are distinguished by their large molecular weight and are detected less frequently compared to incomplete antibodies. Capable of agglutinating Rh-positive red blood cells. They are less important during transfusions.
Incomplete ones predominantly belong to the IgG class. They are attached to the surface of Rh-positive erythrocytes without the formation of agglutinates. The gluing of blood cells is carried out in the presence of colloidal solutions and proteolytic enzymes or after treatment with antiglobulin serum. They have a smaller molecular weight compared to full antibodies. Capable of passing through the placenta. During sensitization, complete antibodies are first produced, then incomplete antibodies (IgG immunoglobulins) are produced to a greater extent.
Over 90% of complications during blood transfusions are caused by incompatibility of the donor and recipient with the Rho(D) antigen. The hr'(c) antigen is also of great importance. Agglutinogen is present in 80–82% of the population. The remaining 18–20% of individuals fall into the high-risk group due to the high likelihood of hr'(c) incompatibility with donors and the development of post-transfusion complications.
Technique for identifying the Rh factor using zoliclon Anti-D-Super
Tsoliklon Anti-D-Super is a complete human anti-D IgM antibody. To obtain reliable results, the analyzed sample must contain a sufficient number of red blood cells.
- Provide good lighting and room temperature in the room.
- Place one large drop (approximately 0.1 ml) of Anti-D IgM on the plate.
- Place one small drop (approximately 0.03 ml) of the red blood cells being tested nearby.
- Mix two drops with a sterile stick.
- After 10–15 seconds, gently rock the plate for 20–30 seconds.
- Check for agglutination three minutes after mixing.
If a reaction occurs, the blood is assessed as Rh-positive (Rh+), if there is no reaction - as Rh-negative (Rh-). If agglutination is negative or weak, it is necessary to repeat the test with incomplete anti-D IgG antibodies in order to detect weak or partial D antigen.
reaction result
visual assessment of reaction results in transmitted light
registration of analysis results
Method for determining the Rh factor Du in a tube test
In parallel with the analysis, three control samples are performed: the reagent coliclone Anti-D (anti-D IgG) with standard Rh-positive and Rh-negative erythrocytes, the analyzed erythrocytes with a gelatin solution without the anti-D IgG diagnosticum.
- Place 0.05 - 0.1 ml (one drop) of red blood cells from a clot of coagulated blood or washed from a preservative into a test tube.
- Add 0.1 ml (two drops) of 10% gelatin heated until liquefied at 45 - 50 °C.
- Add one drop of Anti-D Zoliclone (Anti-D IgG).
- Perform mixing.
- Incubate the tube in a water bath for 10–15 minutes or in a thermostat at 48 °C for half an hour.
- Add 5 - 6 ml of isotonic solution.
- Invert the test tube 1 – 2 times.
- Assess for the presence of agglutination in transmitted light.
The absence of reaction results with anti-D IgM and pronounced agglutination with anti-D IgG indicate the detection of weak forms of antigen D. In case of weak agglutination, the test should be repeated in the indirect Coombs test.
Blood type and predisposition to disease
There is an assumption that, depending on the blood, people are prone to certain diseases, but this has no scientific basis.
I (0)
These people are considered to be mentally stable. As for diseases, they are predisposed to arterial hypertension and diseases of the digestive system. Due to the increased acidity of gastric juice, they may develop gastritis, peptic ulcers, and colitis. They suffer from influenza and ARVI more often than others, they have a tendency to form stones in the urinary system, and have poor blood clotting. With negative Rh, skin pathologies may be observed.
II (A)
These people are not very resistant to stress. Their weak point is the thyroid gland (insufficient production of hormones). They are prone to dental diseases. In addition, they are advised to be more careful about their heart: diseases such as ischemic heart disease, hypertension, and heart attack cannot be ruled out. They are susceptible to gastritis with secretory insufficiency, cholelithiasis and urolithiasis, osteoporosis, and diabetes mellitus. It is recommended to monitor your weight and keep it normal, quit smoking and lead an active lifestyle.
Blood type may indicate predisposition to certain diseases
III (B)
Among the carriers of this group, neurasthenics and people prone to psychosis are most often found. There is a high risk of developing hypertension, pancreatitis, rheumatism, and Parkinson's disease. Women are especially susceptible to genitourinary infectious diseases. It is believed that people with group 3 are less likely than others to have a heart attack. They are advised to give up bad habits, move more, and eliminate fatty foods.
IV (AB)
Those with this blood are resistant to ARVI, influenza, bronchitis, and pneumonia. They do not have skin problems, they can boast of healthy teeth, and kidney pathologies are rarely observed. There is a tendency to hypertension, atherosclerosis, obesity, hepatitis, and anemia. These people's blood clots quickly, hence thrombosis and thrombophlebitis.
Question 3:
What dose of anti-Rhesus immunoglobulin and in what time frame is administered to a woman with Rh-negative blood after childbirth? Is it true that the administered dose of the drug should be increased after a caesarean section?
Answer
: Women with Rh-negative blood after childbirth are given anti-Rhesus immunoglobulin in an amount of 1-1.5 ml (200-300 µg) no later than 24-48 hours after birth for prophylactic purposes. During surgical interventions, transplacental bleeding may increase, and therefore the administered dose of anti-Rhesus immunoglobulin is increased by 1.5 times.
Compatibility of father and mother
We now know that the discrepancy between the blood characteristics of a pregnant woman and the embryo has serious consequences. They are especially severe in the case when the child has a third negative blood group, and the mother has the first or second. But let us note once again that the danger is real only for problematic pregnancy.
But now let’s move on to the Rh harmony of father and mother. Let's look at the compatibility of parents who have blood group 3:
- The third is negative in a woman. A suitable father is with blood types 1 and 3.
- The third is negative in a man. A suitable mother is with the 3rd and 4th blood groups.
What threatens the incompatibility of mother and father by Rhesus?
Methods for determining blood categories
Diagnostics to calculate blood groups is carried out after obtaining venous or blood material from the patient. To establish the Rh factor, you will need blood from a vein, which is combined with two serums (positive and negative).
The presence of one or another Rh factor in a patient is indicated by a sample where there is no agglutination (sticking together of red blood cells).
To determine the blood mass group, the following methods are used:
- Express diagnostics is used in emergency cases; an answer can be obtained within three minutes. It is carried out using plastic cards with dried reagents applied to the bottom. Shows group and rhesus at the same time.
- Double cross-reaction is used to clarify a questionable test result. The result is assessed after mixing the patient's serum with red blood cell material. The information is available for interpretation after 5 minutes.
- In this method of diagnosis, zoliclonization replaces natural sera with artificial zoliclones (anti-A and -B).
- Standard bloodstream categorization is performed by combining a few drops of the patient's blood with serum samples with four instances of known antigenic phenotypes. The result is available within five minutes.
If agglutination is absent in all four samples, then this sign indicates that this is the first group. And in contrast to this, when erythrocytes stick together in all samples, this fact indicates the fourth group. With regards to the second and third categories of blood, each of them can be judged in the absence of agglutination in the biological sample of serum of the determined group.
General information
Blood is a biological fluid that circulates throughout the body of every person in a volume of 5-6 liters (approximately 7% of body weight). Researcher K. Landsteiner discovered four of its categories:
- The first one is O.
- The second is A.
- Third - V.
- The fourth is AB.
The most common option is the first, the rarest is the fourth. The third negative will be in honorable second place in terms of non-prevalence.
How to determine the third negative?
The determination method is universal for all groups - this is giving a blood sample for analysis. The collection is carried out from a vein. The study can be carried out by almost any clinic. This procedure is worth going through not only out of curiosity. You will receive vital information for donation and family planning. The event always precedes blood transfusion, tissue and organ transplantation.
Preparing for the analysis is simple:
- It is better to donate blood in the morning and on an empty stomach (at least 4 hours after the last snack).
- After completing the course of drug treatment, at least 2 weeks should pass.
- If it is not possible to stop taking your medication, be sure to tell your specialist what you are taking.
- The day before the procedure, avoid alcohol, salty, fatty, and spicy foods.
- Before taking blood, protect yourself from physical and emotional stress.
The third negative blood category is one of the rarest. However, for its carriers the fact will not be a problem. On the contrary, this is a feature of the psychological portrait of the individual, which, according to scientists, is also influenced by antigens. It is important to know this blood group for planning pregnancy, donating blood, tissues, and organs.
Other group classifications
The discovery of unexpected group incompatibility in all the tests performed continues to develop and does not stop research into the meaning of different erythrocyte antigens.
- The Kell system takes third place in identification after Rhesus, takes into account 2 antigens “K” and “k”, and forms three possible combinations. Important during pregnancy, the occurrence of hemolytic disease of the newborn, complications of blood transfusion.
- Kidd system - includes two antigens associated with hemoglobin molecules, provides three options, is important for blood transfusion.
- Duffy system - adds 2 more antigens and 3 blood groups.
- The MNSs system is more complex, includes 9 groups at once, takes into account specific antibodies during blood transfusion, and clarifies pathology in newborn babies.
The definition is shown taking into account different group systems
The Vel-negative group was discovered in 1950 in a patient suffering from colon cancer. She had a severe reaction to a repeat blood transfusion. During the first transfusion, antibodies to an unknown substance were formed. The blood was of the same Rhesus group. The new group began to be called “Vel-negative”. It was subsequently found that it occurs with a frequency of 1 case in 2.5 thousand. Only in 2013, an antigen protein called SMIM1 was discovered.
In 2012, joint research by scientists from the USA, France and Japan identified two new protein complexes of the erythrocyte membrane (ABCB6 and ABCG2). In addition to their antigenic properties, they transport electrolyte ions from outside to inside cells and back.
In medical institutions it is not possible to find out blood groups based on all known factors. Only group affiliation in the AB0 system and the Rh factor are determined.
Nutrition
People with a third negative blood group are, as a rule, omnivorous and unpretentious, and have a good appetite. But when there is a large choice, they give preference to meat products, smoked meats, overly spicy and salty dishes, which leads to intestinal problems.
Dietary recommendations to maintain their health include moderate consumption of meat - lamb, poultry, preference for protein foods from fish and seafood. Any cereals, low-fat dairy products and cheeses, nuts, legumes, and almost all vegetables and fruits are recommended. Black tea and coffee are recommended to be consumed in moderation.
The following products are not recommended for consumption:
- fatty meat of pork, chicken, duck;
- smoked meat and fish products;
- crustacean dishes, shrimp;
- baked goods, ice cream, cakes;
- tomatoes and ketchup;
- alcohol;
- from herbs and infusions - aloe, hops, linden.
Herbal teas and drinks made from rosehip, mint and lemon balm, ginger, sage will be very useful, that is, they have a calming effect on the nervous system and improve digestion.