Pulmonary hypertension is a disease in which blood pressure in the pulmonary artery increases by 20 mmHg. or more at rest and more than 30 mm Hg. under loads. In terms of frequency, this disease is in third place among cardiovascular diseases in people over the age of 30 (the first and second places are occupied by ischemic heart disease and arterial hypertension, respectively).
- Causes and pathogenesis
- Symptoms and diagnosis
- Treatment of pulmonary hypertension
- Forecast
Causes and pathogenesis
Pulmonary hypertension is divided into congenital and acquired. Otherwise, these forms are called primary and secondary. Among the causes of increased pressure in the pulmonary artery are the following:
- chronic lung diseases (bronchial asthma, COPD, sarcoidosis, interstitial pulmonary fibrosis, tuberculosis, silicosis, asbestosis)
- heart diseases (heart failure, acquired and congenital heart defects)
- stay in the highlands
- vasculitis
- effects of drugs on the body
- TELA
Pulmonary hypertension without a known cause is called primary hypertension. The cause of PH may be an increase in pressure in the pulmonary veins. Growth is provoked by the following factors:
- left ventricular failure
- mitral valve defects
- pulmonary vein compression
- left atrium myxomas
Increased pulmonary blood flow can also trigger pulmonary hypertension:
- patent ductus arteriosus
- ventricular septal defect
- atrial septal defect
Among the causes of the disease in question is an increase in pulmonary vascular resistance, which can be caused by:
- taking drugs that reduce appetite (fenfluramine) or chemotherapy drugs
- obstruction of the pulmonary artery and its branches
- inflammatory changes in the lung parenchyma
- destruction of the pulmonary vascular bed (with chronic destructive lung diseases, pulmonary emphysema)
- chronic alveolar hypoxia (for example, when staying high in the mountains)
Valvular defects lead to the occurrence of passive PH as a result of the transfer of pressure from the left atrium to the pulmonary veins and then to the pulmonary artery system. With mitral orifice stenosis, there can sometimes be a reflex spasm of the pulmonary arterioles due to increased pressure at the mouths of the pulmonary veins and in the left atrium. Long-term development of PH leads to irreversible sclerotic changes in arterioles and their obliteration.
If a person has congenital heart defects, PH results from increased blood flow in the pulmonary artery system and resistance to blood flow in the pulmonary vessels. Left ventricular failure, which occurs with dilated cardiomyopathy, coronary heart disease, and hypertension, can also cause pulmonary hypertension because the left atrium and pulmonary veins become higher than normal.
In chronic diseases of the respiratory organs, PH for a long period of time has a compensatory nature, because hypoxic pulmonary vasoconstriction turns off non-ventilated areas of the lungs from perfusion, which eliminates the shunting of blood in them, and hypoxemia decreases. At this stage, the use of a drug such as aminophylline reduces pressure in the pulmonary circulation, reduces compensatory vasostriction, and reduces intrapulmonary shunting of blood with deterioration of oxygenation. As lung disease progresses, PH becomes a factor in the pathogenesis of the formation of chronic “pulmonary heart.”
Symptoms and diagnosis
The main manifestation of pulmonary hypertension is shortness of breath, which has the following features:
- noted when a person is at rest, physically passive
- increases even with little physical activity
- noted even when the person is sitting (cardiac dyspnea does not have this feature)
Patients with pulmonary hypertension may also have the following symptoms:
- Dry (non-productive) cough
- Fast fatiguability
- Edema of the lower extremities
- Chest pain (caused by dilation of the pulmonary artery and right ventricular myocardial ischemia)
- Pain in the area of the right hypochondrium
- In some cases, the voice is hoarse because the nerve is compressed by the dilated trunk of the pulmonary artery and the recurrent laryngeal nerve.
- Syncope during exercise is likely because the right ventricle cannot increase cardiac output to meet the demands of the body, which increase with exercise.
During examination, the doctor notes cyanosis, which occurs due to reduced cardiac output and arterial hypoxemia. Pulmonary cyanosis differs from cardiac cyanosis by peripheral vasodilation, which is caused by hypercapnia, which explains the warmth of the patients' upper extremities. Also likely to be detected during examination are pulsations in the second intercostal space to the left of the sternum, which is associated with the trunk of the pulmonary artery; pulsations in the epigastric region associated with a hypertrophied right ventricle.
With severe heart failure, examination reveals swelling of the jugular veins both during exhalation and inhalation, which is a typical manifestation of right ventricular heart failure. Hepatomegaly and peripheral edema are also detected.
Auscultation of the heart reveals the following signs:
- Fixed second tone splitting
- Systolic click and accent of the second tone over the pulmonary artery
- Systolic murmur is heard in the projection of the 3-leaf valve as a result of its insufficiency
- In the second intercostal space to the left of the sternum - systolic ejection murmur
If pulmonary hypertension is suspected, a diagnostic method such as X-ray examination is also used. It makes it possible to detect the expansion of the pulmonary artery trunk and the roots of the lungs. PH is manifested by dilatation of the right descending branch of the pulmonary artery by more than 16-20 mm.
ECT may show changes as a result of the following factors:
- turning the heart
- pulmonary hypertension
- cardiac disposition due to emphysema
- myocardial ischemia
- changes in blood gas composition
- metabolic disorders
If the electrocardiogram is normal, the diagnosis of pulmonary hypertension cannot be rejected. Signs of right ventricular hypertrophy, deviation of the electrical axis of the heart to the right, etc. may be detected.
Echocardiography may reveal thickening of the right ventricular wall and dilation of the right atrium and right ventricle. Also, using this method, the pressure in the right ventricle and the pulmonary artery trunk is determined using the Doppler method.
Catheterization of the cardiac cavities and direct manometry are reliable methods for diagnosing the disease in question. They can detect an increase in pressure in the pulmonary artery, while the pulmonary artery wedge pressure remains low or below normal.
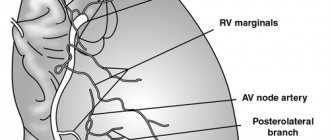
Lung vessels
The pulmonary trunk (truncus pulmonalis) with a diameter of 30 mm emerges from the right ventricle of the heart, from which it is delimited by its valve. The beginning of the pulmonary trunk and, accordingly, its opening are projected onto the anterior chest wall above the place of attachment of the cartilage of the third left rib to the sternum. The pulmonary trunk is located anterior to the remaining large vessels of the base of the heart (aorta and superior vena cava). To the right and behind it is the ascending aorta, and to the left is the left ear of the heart. The pulmonary trunk, located in the pericardial cavity, is directed in front of the aorta to the left and posteriorly and at the level of the IV thoracic vertebra (cartilage of the II left rib) is divided into the right and left pulmonary arteries. This place is called the bifurcation of the pulmonary trunk (bifurcatio tninci pulmonalis). Between the bifurcation of the pulmonary trunk and the aortic arch there is a short arterial ligament (ligamentum arteriosum), which is an overgrown arterial duct (ductus arteriosus).
The right pulmonary artery (a.pulmonalis dextra) with a diameter of 21 mm follows to the right to the gate of the right lung behind the ascending aorta and the terminal section of the superior vena cava and anterior to the right bronchus. In the region of the right lung hilum, in front of and under the right main bronchus, the right pulmonary artery divides into three lobar branches. Each lobar branch in the corresponding lobe of the lung is in turn divided into segmental branches. In the upper lobe of the right lung, there is an apical branch (r.apicalis), posterior descending and ascending branches (rr.posteriores descendens et ascendens), anterior descending and ascending branches (rr.anteriores descendens et ascendens), which follow into the apical, posterior and anterior segments of the right lung.
The branch of the middle lobe (rr.lobi medii) is divided into two branches - lateral and medial (r.lateralis et r.medialis).
These branches go to the lateral and medial segments of the middle lobe of the right lung. The branches of the lower lobe (rr.lobi inferioris) include the upper (apical) branch of the lower lobe [r.superior (apicalis) lobi inferioris], heading to the apical (upper) segment of the lower lobe of the right lung, as well as the basal part (pars basalis). The latter is divided into 4 branches: medial, anterior, lateral and posterior (rr.basales medialis, anterior, lateralis et posterior). They carry blood to the basal segments of the same name in the lower lobe of the right lung.
The left pulmonary artery (a.pulmonalis sinistra) is shorter and thinner than the right, passes from the bifurcation of the pulmonary trunk along the shortest path to the gate of the left lung in the transverse direction in front of the descending aorta and left bronchus. On its way, the artery crosses the left main bronchus, and at the hilum of the lung is located above it. According to the two lobes of the left lung, the pulmonary artery is divided into two branches. One of them breaks up into segmental branches within the upper lobe, the second - the basal part - with its branches supplies blood to the segments of the lower lobe of the left lung.
The branches of the upper lobe (rr.lobi superioris) are sent to the segments of the upper , which give off the apical branch (r.apicalis), anterior ascending and descending (rr.anteriores ascendens et descendens), posterior ( r.posterior) and lingual r .lingularis) branches. The superior branch of the lower lobe (r.superior lobi inferioris), as in the right lung, follows into the lower lobe of the left lung, to its upper segment. The second lobar branch - the basal part (pars basalis) is divided into four basal segmental branches: medial, lateral, anterior and posterior (rr.basales medialis, lateralis, anterior et posterior), which branch in the corresponding basal segments of the lower lobe of the left lung.
In the lung tissue (under the pleura and in the area of the respiratory bronchioles), small branches of the pulmonary artery and bronchial branches extending from the thoracic aorta form systems of interarterial anastomoses. These anastomoses are the only place in the vascular system in which blood can move along a short path from the systemic circulation directly to the pulmonary circulation.
The figure shows the arteries corresponding to the segments of the lungs.
Right lung
Upper lobe
- apical (S1);
- rear (S2);
- anterior (S3).
Average share
- lateral (S4);
- medial (S5).
Lower lobe
- upper (S6)
- ;mediobasal (S7);
- anterobasal (S8);
- lateralobasal (S9);
- posterobasal (S10).
Left lung
Upper lobe
- apical-posterior (S1+2);
- anterior (S3);
- upper reed (S4);
- lower reed (S5).
Lower lobe
- upper (S6);
- anterobasal (S8);
- lateralobasal, or laterobasal (S9);
- posterobasal (S10).
PULMONARY VEINS
Venules begin from the capillaries of the lung, which merge into larger veins and form two pulmonary veins in each lung.
Of the two right pulmonary veins, the upper one has the larger diameter, since blood flows through it from the two lobes of the right lung (upper and middle). Of the two left pulmonary veins, the inferior vein has the larger diameter. At the gates of the right and left lungs, the pulmonary veins occupy their lower part. In the posterior upper part of the root of the right lung is the main right bronchus, anterior and inferior to it is the right pulmonary artery.
- LVLV - left superior pulmonary vein
- RSPV - right superior pulmonary vein
- ILV - inferior pulmonary vein
- RPA - right pulmonary artery
- LPA - left pulmonary artery
At the top of the left lung is the pulmonary artery, posterior and inferior to it is the left main bronchus. In the right lung, the pulmonary veins lie below the artery, follow almost horizontally and on their way to the heart are located behind the superior vena cava, the right atrium and the ascending aorta. Both left pulmonary veins, which are somewhat shorter than the right ones, are located under the left main bronchus and are also directed to the heart in the transverse direction, anterior to the descending aorta. The right and left pulmonary veins, perforating the pericardium, flow into the left atrium (their terminal sections are covered with the epicardium).
Treatment of pulmonary hypertension
Therapy depends on the cause that led to the development of pulmonary hypertension. It must be remembered that the pressure in the pulmonary artery may exceed normal due to the following factors:
- physical exercise
- hypothermia
- pregnancy
- stay in the highlands
The condition of a person with pulmonary hypertension can be alleviated by inhaling oxygen. But it is contraindicated for those who have right-to-left shunting and arterial hypertension.
In chronic nonspecific lung diseases, pulmonary hypertension can be reduced with the help of such medications6
- slow calcium channel blockers
- aminophylline
- nitrates
But they do not affect the life expectancy of people with PH, which was proven by studies no more than 20-30 years ago. It is possible to reduce PH and increase life expectancy with long-term low-flow oxygen therapy.
Taking diuretics reduces the severity of right ventricular failure. But when prescribing, some caution is needed, because in patients with pulmonary hypertension, large diuresis can reduce the preload on the right ventricle and cardiac output will decrease. A relevant drug is furosemide, which is prescribed at a dose of 20-40 mg per day. Taken orally. Hydrochlorothiazide is also effective at a dose of 50 mg/day orally.
Slow calcium channel blockers are used to reduce pulmonary artery pressure in patients with established pulmonary hypertension. The effect is exerted by nifedipine at a dose of 30-240 mg/day or diltiazem at a dose of 120-900 mg/day.
Cardiac glycosides are not effective drugs for the treatment of patients with PH. They can be used in small doses for atrial fibrillation to slow the heart rate. It should be taken into account that in patients with PH, glycoside intoxication develops faster as a result of hypoxemia and hypokalemia during diuretic therapy.
If drug treatment does not produce results, lung or heart-lung transplantation is recommended.
Degrees of pulmonary hypertension by pressure
Doctors at the Yusupov Hospital use echocardiography or cardiac catheterization to determine the severity of the disease. There are three degrees of severity of pulmonary hypertension:
- Increase in pressure in the pulmonary artery by 25 - 45 mmHg. Art. Indicates stage I of the disease;
- Increase in pressure by 45-65 mmHg. Art. – pulmonary hypertension II degree;
- An increase in pressure of more than 65 mm Hg. Art. – pulmonary hypertension stage III.
Pulmonary hypertension syndrome is also classified depending on the observed clinical picture. In this case, 4 classes are distinguished:
- Class I: patients do not experience a decrease in physical activity. Habitual loads do not cause shortness of breath, dizziness, weakness and pain;
- Class II: patients experience a decrease in physical activity. During normal exercise, the patient experiences dizziness, shortness of breath, chest pain, and weakness. At rest, these symptoms disappear;
- Class III: the physical activity of patients is significantly impaired. With a slight load, symptoms characteristic of this disease appear;
- Class IV: significant decrease in activity. Stage 4 pulmonary hypertension is characterized by severe symptoms both at rest and with minimal physical activity.