In this article we will find out how much a heart transplant costs. Transplantology of this organ is a separate field of medicine. It arose at the intersection of immunology and cardiology. Immunology is a science that deals with human immunity and is of great importance in matters of transplant rejection and engraftment (transplanted biomaterial).
The first research carried out in the field of transplantation began in the 50s of the last century. Surgical interventions that ended successfully were carried out by doctors in the USA and South Africa in the 80s. In the USSR, the first such operation was carried out by V.I. Shumakov in 1988. Due to the fact that the immunological basis associated with the host-graft reaction has not been sufficiently studied, the duration and quality of life after surgical manipulation did not correspond to the desired results, and the prognosis was uncertain. Read about the cost of a heart transplant below.
Currently, the level of knowledge has increased significantly and allows such operations to be carried out with a minimal likelihood of complications. In addition, life expectancy after heart transplantation is sufficient (slightly less than half of patients live more than 10 years after the intervention).
In some cases, it is possible to perform repeated transplants, for example, one of the richest people in the world, according to Forbes, D. Rockefeller, underwent his sixth heart transplant at the age of 99.
Many patients suffering from various pathologies and their relatives are interested in how much a heart transplant costs.
Indications for transplantation
Heart transplantation is the least common procedure in cardiac surgery. This is due not only to high financial costs, but also to certain nuances:
- A limited number of donors are individuals who have a healthy heart but are confirmed brain dead.
- Long time required to select a donor in accordance with waiting lists. This problem is especially relevant in relation to heart transplant operations for a child.
- The problem is of an ethical nature, including from the point of view of religion (in particular, according to Christian ideas, a person is considered alive as long as his heart beats).
- Short shelf life of the donor organ (up to 6 hours).
But, despite the problems described, transplantation operations, although very rare, are carried out, and quite successfully. It is important to find out in advance how much a heart transplant surgery costs.
The main indication for which the patient requires this operation is the final (terminal) stage of heart failure in chronic form, or the third or fourth functional class, not amenable to drug therapy, with a survival prognosis of less than a year in this condition.
It is the symptoms characteristic of the last stage (the occurrence of shortness of breath at rest, significant swelling of the whole body and limbs, significant limitation of activity) in the absence of the effectiveness of conservative treatment that may require a heart transplant. Cost doesn't matter to many people.
Such severe cardiac failure can occur as a result of the following pathologies:
- Cardiomyopathy. This disease is a condition in which a structural restructuring of the myocardial fibers occurs, replacement with scar tissue, as a result of which the process of contraction and relaxation of the heart muscle is disrupted. Typically, CHF develops with ischemic and dilated cardiomyopathy.
- Acquired or congenital inoperable defects of the heart muscle.
- Heart tumors.
- Severe cardiac arrhythmias and uncontrollable angina that are not amenable to drug treatment and have led to severe impairment of cardiac function.
In addition to the indications listed above, the results of objective research methods (pulmonary artery catheterization, cardiac ultrasound) are taken into account:
- Absence of severe pulmonary hypertension.
- The left ventricular ejection fraction is less than 20%.
In addition, when planning surgical intervention, certain conditions must be met:
- The age of the recipient (the patient undergoing an organ transplant) must be less than 65 years.
- The patient’s desire to follow a further strict plan of therapy and observation, his compliance.
What determines the cost of heart muscle?
The heart muscle is rightfully recognized as the most expensive organ in the human body. Most often, people who decide to sell it take such a serious step due to financial problems in their lives. And only sometimes this happens for religious or ethical reasons of the donor. The cost of heart muscle transplantation depends mainly on three factors:
- Purchasing one organ (heart) or the need for a complex transplant (heart and pair of lungs)
- Urgency of transplantation (surgical intervention by doctors costs the patient several times more)
- Selecting a supplier (making a deal through a clinic or purchasing from sellers on the “black market”).
Requirements for a donor heart
How much does a heart transplant cost is a pressing question today. To understand this, you need to understand that an organ donor can be a person who is in a coma and whose brain death has been confirmed, and whose cardiac activity is supported in the intensive care unit with the help of equipment. As a rule, such severe patients are observed in hospitals after strokes or road accidents. That is, the person is actually already dead, since his heart works with the help of medications, and he breathes thanks to a ventilator. If the heart of such a person is transplanted into another person, it will be able to work autonomously in the new body. To remove an organ from a patient’s body, doctors need the consent of the patient himself, drawn up while he was still alive, or his relatives. If there are no relatives, or if the patient is not identified, his heart may be removed without official documentation.
A commission consisting of several people, including the head physician of the medical institution where the donor is located, fills out the necessary papers. After this, a specialist from the transplant center arrives, always with an assisting nurse, and performs an operation during which the donor heart is removed, and then placed in a container filled with a cardioplegic solution and transported to the center. What determines how much a heart transplant costs in Russia?
Donor hearts are selected according to the following criteria:
- There are no malignant tumors.
- There is no viral hepatitis (B, C), HIV infection.
- Absence of cardiac pathologies, as confirmed by the results (coronary angiography, cardiac ultrasound, ECG).
- The blood groups of the recipient and donor are compatible according to the ABO system.
- The heart sizes of the recipient and heart donor are approximate. The assessment is carried out using ultrasound.
Life expectancy and doctors' forecasts
If a heart transplant is successful, how long patients live depends on their age, lifestyle and response to prescribed medications. People are able to take care of themselves and can work in benign conditions. People who have undergone a transplant feel much better than before. Statistics show that successful surgery can extend a person's life by 5 or 10 years.
One year after transplantation, patient survival is 80-85%. Over time, their number becomes smaller, because infectious diseases arise that are very difficult to fight. 5-7 years after transplantation, complications occur in the form of pathologies of the valves and coronary arteries. 45% of patients live about 10 years. There is a category of patients who have set a well-deserved record of survival after a donor heart transplant. Their number is 15%, and they live 15-20 years. There are fewer such patients than others, but these are cases from real medical practice.
Despite the complications, the overall prognosis after surgery can be considered favorable. Much depends on the patient’s state of mind, his self-discipline and mood for a full life. It is in such cases that the life expectancy of a person with a transplanted heart can be maximum.
Waiting time for transplant surgery
To understand how much a heart transplant costs in Moscow, let’s first determine the time frame. In order for a patient to undergo surgery, a waiting list is drawn up at the transplant center. These centers cooperate with medical institutions where possible donors can potentially be observed - neurological, trauma and other hospitals. Periodically, the center requests information from hospitals about the availability of possible heart donors, and then matches the list of patients in need of a transplant with available donors in accordance with the selection criteria listed above. The patient can receive a referral to the transplant center from the attending physician - a cardiac surgeon or cardiologist.
A considerable amount of time may pass from the moment the waiting list is drawn up. If a suitable donor is never found, the patient may die due to cardiac failure without receiving a transplant. If a donor is found, the transplant operation will be carried out in the near future.
Since the predicted survival of a patient for such an indication as CHF is less than a year, a donor should be found within this critical period.
How to get to Germany for treatment?
Clinics in Germany accept foreign patients for surgical treatment, including organ transplantation. A prerequisite for registering for an operation is the correct preparation of a package of medical and administrative documents, registration of permission to enter the country, official confirmation of readiness to perform the operation from the clinic and a number of other nuances.
Most patients and their relatives do not have experience in organizing treatment abroad. They make mistakes and cannot communicate productively with the clinic administration. Therefore, it is better to contact German medical institutions not on your own, but with the help of the international medical tourism operator Booking Health. Booking Health specialists will help you with such important points:
- Choosing the right clinic based on the annual qualification profile
- Direct communication directly with the attending physician
- Preliminary preparation of a treatment program without repeating previously conducted examinations
- Ensuring favorable prices for clinic services, without surcharges and coefficients for foreign patients (savings up to 50%)
- Make an appointment for the desired date
- Control of the medical program at all stages
- Assistance in purchasing and shipping medications
- Communication with the clinic after completion of treatment
- Control of invoices and return of unspent funds
- Organization of additional examinations
- Service of the highest level: booking hotels, plane tickets, transfers
To use the help of Booking Health, leave a request on the website. A medical consultant will contact you within 24 hours and you will begin preparing for your trip.
How much does a heart transplant cost?
All over the world, a law has been passed that prohibits organ trafficking and only family or cadaveric transplants are allowed. In this regard, the patient receives the heart itself free of charge. You will only need to pay for the operation itself, drug support before and after transplantation, as well as the rehabilitation period.
So, how much does a heart transplant cost in Russia? In general, the price varies and ranges from 70-500 thousand dollars. The average cost of a transplant operation is 250 thousand rubles. In the Russian Federation, it is possible to provide citizens with high-tech types of medical care free of charge, as well as to pay for transplantation operations according to quotas (under the compulsory medical insurance system), however, in any case, the possibility of free transplantation and its exact cost should be clarified with the treating specialist.
Where is a heart transplant performed? On the territory of Russia there is only one coordination center that selects donor organs. It operates in the Moscow region and Moscow. Direct heart transplants are performed in the following medical institutions:
- "North-Western Federal Medical Research Center named after. Almazova V.A.” Federal State Budgetary Institution, located in St. Petersburg.
- Research Institute of Circulatory Pathology named after. Meshalkina E.N., located in Novosibirsk.
- Federal Scientific Center for Transplantology and Artificial Organs named after. Shumakova V.I., located in Moscow (FSBI "FNTSTIO").
In recent years, the development of transplantology has begun in Chelyabinsk, namely in the Chelyabinsk Regional Clinical Hospital. What is the cost of a heart transplant in Chelyabinsk? The price must be confirmed with the clinics. But it is not much different from the capital.
In addition, transplantation is also carried out in the capital of Belarus - Minsk. That is, the geography of such operations is rapidly expanding. How much does a heart transplant cost in Minsk? Its price is about 70 thousand dollars.
Due to the fact that in Russia the legal standards for organ donation have not been fully developed, heart transplantation operations are performed very rarely. For example, during 2014, only 200 such manipulations were performed, while approximately 28 thousand transplant operations were performed in the United States during the same period. In addition, due to the legal ban on the removal of donor organs from people under 18 years of age, children requiring heart transplants required expensive treatment abroad (India, Germany and Italy). However, in May 2015, a legislative act was adopted on the procedure for ascertaining brain death in patients older than 1 year. This made it possible for the subsequent development of legislation in the field of child donation.
Question: “How much does a heart transplant cost in Germany?” occurs almost immediately after the decision to undergo surgery is made. Prices vary between clinics. On average this is 400 thousand euros.
What is an artificial heart
The mechanism received the English name “TAN”. If the abbreviation is deciphered and translated from English, “TAN” means “Total Artificial Heart”. This is a device used to replace ventricles during transplantation.
Mechanisms capable of maintaining the human body in a viable state are divided into two large groups:
- Oxygenators are devices that saturate the patient’s blood with oxygen.
- Cardiac prostheses are implants that are installed in the body for its life support.
Both groups of devices are used during prolonged operations on open myocardium and while waiting for a donor heart for further transplantation.
A device capable of driving blood through human veins was invented by Dr. Demikhov in the USSR. In the 30s of the last century, as an experiment, a doctor performed a heart replacement operation on a dog, installing a pump in place of the organ. The device was connected to the engine externally. Almost 30 years later in America, scientists Akutsu and Kolf came up with a plastic heart that includes four valves. The model of the device was as close as possible to a real human organ.
The first successful replacement of a diseased organ with an artificial mechanism took place in 1969 by Dr. Cooley in the USA. His patient had a serious diagnosis - a left ventricular aneurysm. The doctor removed part of the affected myocardium. As a result of the operation, the patient’s body was unable to independently maintain blood flow.
A heart transplant was presented as the only chance to save the patient's life. Dr. Cooley installed a mechanical device that made it possible to disconnect the patient from the external circulation machine. The patient lived with an artificial heart in his chest while his own organ was damaged. The transplant lasted 64 hours! During this time, doctors were able to find a donor organ. The patient underwent a second operation: the artificial organ was replaced with the healthy heart of another person. The transplant was successful.
Dr. Denton Cooley
Ironically, the donor's strong and healthy heart did not save the patient's life. Despite the successful two-stage heart muscle transplantation, the patient lived only two days. He died of pneumonia.
Interestingly, in the last century, all further attempts to create a mechanical model of the heart muscle were unsuccessful. It was only in 2010 that the mechanism was installed for the first time in a patient. This happened in a Moscow clinic. An artificial organ helped the patient survive while waiting for a donor.
The mechanism is installed on the atria, replacing the lower sections - the ventricles. Mechanical valves function near the atria, similar to natural heart valves. They regulate blood flow, direct the blood that enters the affected organ.
The mechanical device installed in the chest is quite large in size and has an impressive volume. It will not fit into every chest cavity. There are no devices that can be installed by children. A smaller artificial heart is currently being developed.
Contraindications for transplantation
Such surgical intervention is contraindicated in the following situations:
- Severe form of pulmonary hypertension (presence of high pressure in the pulmonary artery).
- A severe form of diabetes mellitus, in which there is damage to the retina, kidneys, and blood vessels.
- Active tuberculosis process, HIV infection.
- Acute forms of infectious diseases.
- Severe forms of liver and kidney failure.
- Systemic diseases of an autoimmune nature (rheumatoid arthritis, systemic lupus erythematosus, others).
- Severe degree of chronic obstructive disease.
- Drug and alcohol addiction.
- Oncological diseases.
- Acute stages of mental illness.
We talked about the cost of a heart transplant in Moscow.
The process of preparing for surgery
If a patient is referred to a transplant center and a decision is made to place him on the waiting list for an organ transplant, he is assigned a special examination plan. The tests required in this case are:
- Examination by a urologist, gynecologist.
- Examination by a dentist, otorhinolaryngologist (this is necessary to exclude the presence of chronic infectious foci in the oral cavity and nasopharynx).
- Examination by a cardiac surgeon.
- ECG, ultrasound of the heart, CAG (if necessary).
- General laboratory examination of urine samples.
- Clinical laboratory examination of blood samples, determination of blood group, coagulation system.
- Blood tests for markers of syphilis, viral hepatitis, HIV infection.
- X-ray examination of the chest organs or fluorography.
To be admitted to a transplant center for surgery if a donor is available, the patient must always have copies and originals of the following documentation available:
- Passport, health insurance policy, SNILS.
- An extract received from the sending institution and containing the results of all examinations performed.
- A referral received from a medical institution at the place of registration of the recipient. Information should be collected about the cost of heart transplant surgery.
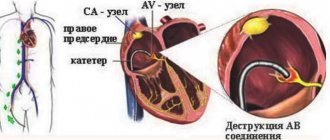
Method of performing transplant surgery
The heart transplant procedure in Moscow begins with the removal of the donor organ from the body and placing it in a container with a cardioplegic solution for no more than 4-6 hours. During this time, preoperative preparation of the recipient is carried out (premedication - sedative and analgesic drugs are administered). Then, in the operating room, using general anesthesia, the recipient's anterior chest wall is cut, large vessels are connected to a machine that performs artificial blood circulation (ACB), which will perform the function of an artificial heart during the operation.
Then the left and right ventricles of the heart are cut off. The atria are preserved. Preserving your own atria allows you to leave the sinus node active, which sets the rhythm of heart contractions and is the pacemaker.
The donor's atria are then sutured to the recipient's atria and a temporary pacemaker is placed to maintain adequate heart rate after transplantation. The chest is sutured and an aseptic bandage is applied. This operation takes several hours, usually no more than 6.
The next stage of surgical intervention is cardiotonic (supporting cardiac activity) and immunosuppressive treatment. Immune suppression (usually through the use of cyclosporine) is required to eliminate rejection reactions and successful graft engraftment.
Heart donors: who are they?
Donors are often people who have suffered in serious car and train accidents. They are sent to the intensive care unit. Such patients are in a comatose state, and doctors keep them alive with a ventilator. Before considering donation, doctors must conclude that the patient's condition is hopeless. Brain death and lack of brain function must be recorded. After the research, doctors can make a request to the patient’s relatives. Practice shows that relatives often make a positive decision about donation.
If relatives express their consent to donation, they sign several documents, and the patient is disconnected from the life support system. In many cases, the decision to donate is made on an emergency basis. The organ is quickly removed from the body and placed in a compound that preserves its properties, and delivered to the patient who needs a transplant.
There is a practice that is gradually becoming real in our country. There are people who, during their lifetime, draw up a will with a notary. In their will, they indicate that their organs can serve medicine and living people posthumously.
Possible complications after transplantation
Among the complications that can occur in the early period after surgery are bleeding from the wound and infectious lesions. The first can be treated quite successfully by reopening the wound and suturing the source of bleeding. To prevent infectious (viral, fungal, bacterial) complications, the patient is prescribed antibiotic medications and an adequate immunosuppression regimen.
In the long-term period after surgery, the development of rejection of the transplanted heart, as well as dysfunction of the coronary arteries, accompanied by myocardial ischemia of the donor organ, is likely.
Complications in the postoperative period
After transplantation, the patient is left with a large vertical scar. It continues from the sternoclavicular joint to the navel. Patients hide it by wearing high-collared clothing or using retouching cosmetics.
Important! The first 10 days after surgery are the most dangerous and difficult period. Adaptation to the transplant occurs.
At the beginning of the period after transplantation, the following complications may occur:
- donor organ rejection;
- formation of blood clots in the great vessels;
- addition of infectious diseases;
- internal bleeding;
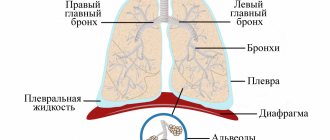
- inflammation of the lungs as a result of stagnation in them;
- renal and hepatic pathologies;
- infectious pericarditis;
- arrhythmic disorders.
Late complications include:
- malignant neoplasms;
- myocardial infarction;
- ischemic processes;
- heart valve insufficiency;
- atherosclerotic changes;
- vascular pathologies.
Late complications may appear several months or years after surgery.
Lifestyle after transplant
The patient’s lifestyle in the postoperative period after a heart transplantation procedure consists of the following components:
- Nutrition. It is important for the patient to switch to a healthy lifestyle, completely stop drinking alcoholic beverages and smoking. It is necessary to follow a diet, excluding harmful foods (smoked, fried, fatty, etc.) from your diet.
- Physical activity. During the first month after surgery, the patient must strictly adhere to the restrictive regime. However, normal daily activity should still be present. After a couple of months, the patient is allowed to return to driving a car, and after a few more, begin light physical activity (walking, gymnastics, etc.).
- Protection against infections. The patient should try to avoid visiting public places for several months after transplantation and contact with people suffering from infectious diseases. It is equally important to wash your hands thoroughly before eating, drink only boiled water, and eat food that has been well heat-treated. This is due to the fact that due to suppressed immunity, the likelihood of the patient becoming infected with viral, fungal, and bacterial diseases increases after the start of immunosuppressive treatment.
- Use of medications. This part of a heart transplant patient's life is the most important. The patient must carefully observe the time of taking medications and strictly follow the dosage prescribed by the doctor. As a rule, we are talking about the use of hormonal drugs and cytostatics, the action of which is aimed at suppressing one’s own immunity, which attacks foreign tissue of the heart muscle.
In general, it should be noted that the patient's life after surgery undoubtedly changes significantly, but the quality of life without swelling, palpitations and shortness of breath changes for the better.
Postoperative prophylaxis
Despite a number of limitations, patients live fully after a heart transplant, and their quality of life becomes much higher. There are cases where patients lived 15 years or more, observing the following preventive measures:
- exclusion of serious physical activity;
- regular walks in the fresh air;
- adherence to sleep, rest and nutrition regimes;
- regularly taking medications prescribed by a doctor;
- avoiding sudden temperature changes;
- eating food that has been heat-treated.
It is also recommended to avoid places where large numbers of people gather. This helps to avoid psychological stress and respiratory diseases that can be “caught” at mass events. Subject to these restrictions, the patient can lead a normal life without arrhythmia, shortness of breath and edema.
Heart transplantation from a religious perspective
Previously, when the field of transplantology was just beginning to develop, representatives of almost all religions had mixed opinions in relation to heart transplantation. For example, representatives of Christianity believed that such an operation was not a godly act, since a person’s still living heart was actually taken away. In addition, it is believed that theoretically a person can emerge from a comatose state after a few months. But due to the fact that doctors clearly differentiate the state of coma and brain death, more and more clergy in recent years have begun to say that saving someone else’s life after one’s own death is the true purpose of a believer, since the basis of such an action is sacrifice. And giving your heart is a benefit to other people.
We looked at the cost of a heart transplant in Russia.