Basic functions of platelets
In appearance, platelets are round or oval red plates with a smooth surface. They are formed in the bone marrow. They mature in approximately 8 days. These components constantly circulate in the bloodstream.
The main function of platelets is to ensure blood clotting. In addition, the ability of these blood components to stop bleeding is important. This is ensured by the fact that individual platelets can stick together and stick to sites of vascular damage. The process is automatically started by the human body when there is a risk of bleeding.
An important question is how long platelets live. Their viability time lasts approximately 10 days. Depending on the age of the red plates, their size changes: from 2 to 5 microns in diameter.
The process of platelet renewal in the blood occurs constantly. Therefore, an important factor to ensure the maintenance of blood condition is the balance between the formation of red plates and their death. Otherwise, there may be a tendency to blood clots or increased bleeding.
Cytoskeleton and shape change
The platelet cytosol is permeated by a three-dimensional network of water-insoluble protein threads (filaments), which forms the cytoskeleton. The filaments consist of polymerized actin protein and ensure that the platelet changes shape when activated. In addition, just below the plasma membrane is a membrane skeleton associated with the cytoplasmic “tails” of some receptors. It consists of short actin filaments connected to each other using special proteins. The membrane skeleton not only supports the plasma membrane, regulating the contours of the cell, and stabilizes it, preventing fragmentation, but also regulates the distribution of receptors attached to it in the plane of the membrane. It is also suggested that it plays an important role in the regulation of various intracellular events that are triggered upon activation.
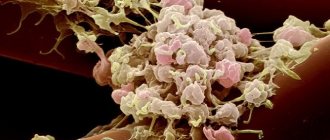
Rice. 5.
Scanning electron micrographs of the process of spreading an activated platelet (
a–d
) over the surface []
Interestingly, the cytoskeleton is a dynamic structure, thanks to which a platelet can not only change shape, but also grow “tentacles” (filopodia). With their help, it spreads over the surface of the damaged vessel (Fig. 5) and more easily adheres to other platelets (Fig. 6). Relatively recently, it was discovered that upon strong activation (by thrombin alone or together with collagen), platelets are divided into two groups (subpopulations), very different in properties and even shape, which suggests a fundamentally different organization of the cytoskeleton in them. Some of them (“regular” activated) have the appearance of amoebas - lumps with filopodia, others (procoagulant, since there is a lot of phosphatidylserine on the outer surface of their membrane) - balls without “tentacles”. The data obtained in our laboratory indicate that some membrane receptors responsible for binding cells to the surface and to each other are unequally attached to the cytoskeleton in platelets from the two subpopulations. This means that they can interact differently with the damaged vascular wall and with each other in the forming blood clot.
The sequence of processes during the restructuring of the platelet cytoskeleton has generally been studied quite little, but here is a new question: why do some cells become “amoebas” when activated, and others become “balls”?
Blood test for platelets
A complete blood test can determine the platelet count. The main indications for its implementation are the following:
- Increased bleeding of gums.
- Heavy menstruation.
- The appearance of bruises from minor impacts.
- Frequent nosebleeds.
- Difficulty stopping bleeding from minor injuries.
The number of platelets in the blood is measured in thousands per 1 microliter of blood. Counting is carried out in specialized laboratories in various ways that guarantee high accuracy.
The normal platelet count in the blood depends on gender and age and is:
- For men, 200–400 thousand.
- In women, 180–320 thousand, during menstruation the amount can decrease to 75–220 thousand, and during pregnancy to 100–310 thousand.
- In children, indicators depend on age, and the corresponding values are given in special tables.
To conduct a general blood test, blood is taken from a finger. No special preliminary preparation is required before this. To ensure accurate results, it is better to donate blood in the morning on an empty stomach. At the same time, 12 hours before the procedure it is not recommended to consume fatty spicy foods, carbonated drinks, and alcohol.
Additionally, to determine blood clotting indicators, Sukharev and Lee-White tests are performed. They are informative and allow you to obtain the necessary additional data about the pathological condition. This will allow you to carry out correct treatment measures and avoid dangerous consequences.
Platelet aggregation
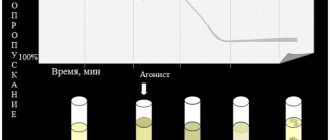
To assess platelet function, CIR Laboratories LLC performs an analysis for induced platelet aggregation. This is a high-quality analysis performed on an automatic aggregometer.
To assess platelet function, the CIR Laboratory performs an analysis for induced platelet aggregation. This is a high-quality analysis performed on an automatic aggregometer. Since this test changes dramatically when taking drugs that affect blood clotting (antiplatelet agents, for example, aspirin, thromboass, anticoagulants, for example, heparin), it is advisable to take it before starting to take these drugs. For each aggregogram, the laboratory doctor issues a conclusion.
A platelet aggregation test is recommended in the following cases: miscarriage, unsuccessful IVF attempts, a history of severe pregnancy complications, infertility of unknown origin, as well as increased bleeding: easy bruising, menorrhagia, nosebleeds.
The aggregation curve evaluates the amplitude of aggregation, the shape of the curve, the presence of one or two waves, and the presence of disaggregation.
The sample shown shows: 1—zeroing of the device, 2—before adding the inductor, 3—peak associated with dilution of the sample by the inductor, 4—reference point, first wave, 5—second wave, 6—disaggregation.
Important information: the combination of taking foods, herbal medicines and nutritional supplements containing components from this list with taking antiplatelet agents (thromboASS) and anticoagulants (heparin) is a dangerous combination due to the risk of bleeding (category D according to the FDA classification). The risk of bleeding in most cases outweighs the potential benefit.
More details At CJSC Laboratories CIR, platelet aggregation is performed with the following inducers:
- Aggregation with ADP
- Aggregation with arachidonic acid
- Aggregation with adrenaline (epinephrine)
- Aggregation with ristocetin. The first three inducers make it possible to evaluate the function of platelets from different sides; they complement each other. Aggregation with ristocetin allows one to suspect a dangerous bleeding condition - von Willebrand disease (von Willebrand factor deficiency). When planning a pregnancy, this analysis is important to eliminate the risk of bleeding during childbirth.
Aggregation with ADP (blue line) and arachidonic acid.
The aggregation response is sharply reduced. There is virtually no disaggregation.
Aggregation with ADP.
The aggregation response is reduced. There is virtually no disaggregation.
Platelet aggregation when taking NSAIDs
(aspirin has the maximum effect)
Aggregation with arachidonic acid. There is no aggregation response. A common situation when taking non-steroidal anti-inflammatory drugs
Also, platelet aggregation with ADP and adrenaline may decrease.
Aggregation with ADP, response reduced. Partial disaggregation.
Aggregation with ristocetin, the aggregation response is sharply reduced.
The analysis is given in Maryino on weekdays and Saturdays from 9.00 to 11.00, on Tretyakovskaya and Voykovskaya on weekdays from 8.00 to 10.00.
What medications affect platelet aggregation?
| Pathogenetic mechanism | The way to realize the impact | Drugs |
| Inhibitors of thromboxane A2 formation | ||
| Phospholipase inhibitors | Prevents the formation of arachidonic acid, inhibits collagen, ADP and adrenaline aggregation | Quinacarpine, high-dose corticosteroids |
| COX inhibitors | Acythelate platelet and COX membranes, block the formation of prostacyclin in the endothelium, inhibiting aggregation and release reactions. Against the background of drugs that block COX, arachidonic acid levels are sharply reduced. | PVP (aspirin, indomethacin, butadione, ibuprofen, sulpirazone), indocid, fenoprofen |
| Thromboxane synthetase inhibitors | They block the synthesis of thromboxane A2 without affecting the synthesis of prostacyclin. Inhibits aggregation under the influence of arachidonic acid | Prostacyclin and its synthetic analogues, imidazole and its derivatives (individual sensitivity) |
| Competitive antagonists of thromboxane A2 | Block thromboxane receptors and inhibit aggregation. Inhibits aggregation under the influence of arachidonic acid | 1,3-Azoprostanoic acid and its derivatives |
| Drugs that increase cAMP levels in platelets | ||
| Adenylate cyclase stimulators | They block the synthesis of thromboxane A2 without affecting the synthesis of prostacyclin. Inhibits aggregation under the influence of arachidonic acid. | Prostacyclin, PGE, diterpene foscolin |
| Phosphodiesterase inhibitors | Prevents cAMP degradation. Inhibit platelet adhesion to the subendothelium, the second wave of aggregation, disrupt the release reaction | Dipyridamole, papaverine, aminophylline, intensain |
| Stimulators of prostacyclin synthesis | They enhance the synthesis of prostacyclin, its release from the endothelium, and weaken its degradation | Anabolic steroids, nicotinic acid, vasopressin |
| Drugs that interfere with calcium transport | ||
| Suppress the second wave of aggregation | Isoptin, nifedipine | |
| Impairs the adhesive-aggregation function of platelets | Furosemide in high concentrations | |
| Disrupts the initial and second wave of ADP-collagen- and adrenaline-platelet aggregation | Nitrofurantoin, aminazine, imipramine, amitriptyline, antihistamines, α- and β-blockers, high (over 20 million units/day) doses of penicillin, carbenicillin | |
| Drugs of different groups | ||
| Anticoagulants | In high concentrations they reduce aggregation | Pelentan, warfarin |
| Dextrans | Reduce platelet aggregation | Reopoliglyukin |
| Anesthetics | Reduce ADP aggregation | Nitrous oxide, cyclopropane, phenobarbital |
| Alcohol | Reduces collagen and ADP aggregation | |
| Antiplatelet agents | Reduce all types of aggregation, significantly enhance the effect of prostacyclin, disrupt the connection between platelets and fibrinogen | Tiklid |
Presentation “Platelet aggregation”
- what is platelet aggregation
- What are platelet granules and what do they contain?
- what platelet activators are there in a living organism and what does the laboratory use?
- requirements for conducting research
- factors affecting platelet aggregation
- interpretation of aggregograms
Assessment of platelet aggregation and pregnancy planning What are you taking?
Effect of drugs on platelet aggregation The use of four inducers in the analysis of platelet aggregation, APS, gene polymorphism Reduced aggregation, polymorphism of hemostasis genes, coagulogram Why take platelet aggregation before pregnancy? Aggregation cost Tags:
Aggregation, ADP, platelets, von Willebrand disease, aspirin
Back to section
Increased platelet levels
Elevated platelets are a pathological condition. It is called thrombocytosis. The main danger of the pathology is the increased risk of blood clots.
The cause of an increase in the level of platelets in the blood can be various diseases. Most often thrombocytosis occurs against the background of:
- Malignant neoplasms.
- Infectious diseases.
- Helminthic infestations.
- Surgical operations.
- Autoimmune pathologies.
- Kidney failure.
High levels of platelets in the blood are observed in older people. Temporarily, indicators may increase after heavy physical exertion, for example, after playing sports.
The symptoms of thrombocytosis are characteristic, but mild. It is imperative to conduct a general blood test if the following symptoms are noted:
- Pain in the fingers and toes.
- Itching of skin surfaces.
- Unreasonable weakness, which leads to decreased performance.
- Lack of appetite.
Decreased platelet levels
Low platelet levels, the norm of which differs between men and women, provoke the development of a condition known as thrombocytopenia. Very often it occurs against the background of uncontrolled use of medications: antidepressants and antibiotics.
The reasons for a decrease in the level of platelets in the blood can be various infectious diseases: ARVI, hepatitis, herpes, etc. Thrombocytopenia can be observed when a large number of blood thinning products are included in the diet. These are ginger, cherries, garlic, onions, etc.
Non-infectious factors that reduce the level of platelets in the blood include pregnancy, vitamin deficiency, alcohol or heavy metal poisoning.
Thrombocytopenia can be suspected based on the following signs:
- Heavy menstruation.
- Frequent nosebleeds.
- The appearance of hematomas.
With a constant pathological decrease in the level of platelets in the blood, the risks of developing severe bleeding and stroke conditions, which are life-threatening, increase.
Restoring platelet levels in the blood
You can normalize the level of platelets in the blood with a balanced diet. It is important to saturate your diet with foods high in materials and microelements. You need to give up spicy food, alcohol, fast food and sweet carbonated drinks, lead a healthy lifestyle and maintain a drinking regime.
If it is not possible to normalize the indicators using natural methods, then you need to undergo a full examination by a hematologist. If platelet levels are elevated, special medications may be prescribed - anticoagulants or antiplatelet agents. They thin the blood and minimize the risk of blood clots. But at the same time, they should be taken only as prescribed by a doctor. It should be understood that stabilization of the condition is possible only after eliminating the underlying causes that provoke deviations from the norm.
References
- Clinical laboratory diagnostics, National guidelines, Volume 1, Dolgov V.V., Menshikov V.V., 2012, pp. 761-765
- Kozlovsky V. I., Kovtun O. M., Seroukhova O. P., Detkovskaya I. N., Kozlovsky I. V. Research methods and clinical significance of platelet aggregation. Focus on spontaneous aggregation // Vestnik VSMU. 2013. No. 4.
- Puri RN, Colman RW.ADP-induced platelet activation.Crit Rev BiochemMol Biol. 1997;32(6):437-502. doi: 10.3109/10409239709082000. PMID: 9444477.
- "Clinical and laboratory diagnosis of platelet function disorders." Vasiliev S.A., Berkovsky A.L., Melkumyan A.L., Suvorov A.V., Mazurov A.V., Kozlov A.A. Federal State Budgetary Institution Hematological Research Center, Ministry of Health of the Russian Federation, Moscow, 2013.