1.General information
The connection between the condition of the kidneys, blood pressure and characteristic swelling has been known for a long time, and not only to doctors. Seeing a pale man with bags under his eyes, rubbing his temples or the back of his head with his fingers, the most discerning among us will immediately ask: is it from the kidneys?
Indeed, in many cases, high blood pressure is caused by kidney dysfunction, and vice versa: lack of blood supply, for example, with atherosclerosis of the renal arteries, leads to damage to the nephron parenchyma (the main tissue of the kidneys, consisting of millions of filtering elements called nephrons) and chronic renal failure.
These processes are complex even for a specialist; research in this area continues, but the widespread prevalence of this type of pathology creates the need to understand at least the basic terms and modern ideas about “renal pressure.”
Arterial hypertension (AH, persistent excess of blood pressure above the conditional threshold of 140/90, hypertension) is classified into two main groups. Essential or primary hypertension is an independent polyetiological disease, against the background of which numerous disorders and complications develop. On the contrary, secondary (symptomatic) hypertension is itself a complication of any pathological process or condition.
Statistical estimates regarding various types of hypertension vary widely, but it is known that the absolute majority of hypertension (up to 95%) are primary.
Regarding secondary hypertension, there are also no clear statistical data or generally accepted classification. The role of renal pathology in this regard is one of the main causes of symptomatic hypertension; According to various estimates, nephrogenic hypertension accounts for from 1-2% to a third of all secondary hypertension. A number of studies highlight an alarming age-related trend: persistent hypertensive blood pressure levels are found in 20-30% of children and adolescents, which is also associated with kidney dysfunction, and in cities this trend is twice as pronounced as in rural areas.
And finally, a few words about terminology. Secondary nephrogenic (renal) hypertension is an indication only of the general cause of high blood pressure; this diagnosis, in fact, is not complete and not specific. The term “renal hypertension” comes from the name of the substance “renin” discovered at the end of the 19th century (in Latin, “kidney” - ren). Renin is a vasopressor produced by the renal glomeruli, i.e. hormone that increases blood pressure. However, the definition of “renal” cannot be considered complete, because An excess of renin in the blood can be caused by both its hypersecretion and disturbances in biochemical processing due to damage to the parenchyma. Therefore, in the literature today one can find clarifying diagnoses of “renoparenchymal”, “renovascular”, “vasorenal” hypertension.
A must read! Help with treatment and hospitalization!
The essence of the diagnosis
Renovascular hypertension is considered a secondary pathology arising from arterial hypertension and manifests itself against the background of the underlying disease. The main cause of the disease is defects in the renal vessels, mainly the branches of the renal artery. With this pathology, due to concomitant provoking factors such as atherosclerosis and vasculitis, the amount of blood entering the kidney through the incoming capillaries decreases.
As a result, insufficient blood supply develops, leading to ischemia - oxygen starvation of the kidney tissue. To compensate for the insufficient amount of incoming blood, the kidney restores it independently by increasing pressure, which increases the production of the vasoconstrictor components angiotensin, renin, and aldosterone. They enter the general blood supply and cause an increase in blood pressure.
As the disease progresses, its own sources of pressure regulation are depleted, and the production of prostaglandins, kinin and kallikrein in the kidney decreases. Increased pressure is no longer able to cope with the problem, kidney nutrition becomes worse, and the disease becomes chronic. Against the background of advanced arterial and renovascular hypertension, high blood pressure causes the development of dangerous consequences. These include myocardial infarction, thrombosis of large vessels, hemorrhages in the fundus and brain (stroke), and left ventricular failure.
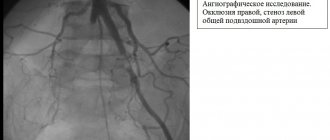
The disease can be cured as long as it is not complicated by target organ damage and does not cause renal artery stenosis. Stenosis is considered to be a narrowing of the arterial lumen by 70% of the original diameter or dilatation located immediately behind the site of pathological narrowing of more than 50%. Developed unilateral or bilateral renal stenosis causes rapid progression of renal failure, which is fraught with dangerous consequences.
There are two types of renovascular hypertension:
- fibromuscular hypertension - its share of the total cases of recorded disease is 10%, it is diagnosed more often in women at a young age. This form of pathology progresses with the appearance of new foci of stenosis or worsening of existing ones;
- ischemic kidney disease - diagnosed in 90% of cases of the disease, the risk of development is higher in patients with diabetes mellitus, cardiac ischemia, heart failure, as well as in elderly and smoking patients.
To restore normal blood flow in the renal system, surgical methods are used, and conservative treatment is prescribed if it is impossible to use other methods (for systemic vasculitis). Medicines are also recommended for subsequent prevention of thrombosis and vascular atherosclerosis. Surgical intervention is carried out by an angiosurgeon, and conservative therapy is carried out by a therapist.
2. Reasons
The most common congenital cause of renal hypertension is a fibromuscular malformation of the renal artery. Many other anomalies of the structure of the kidneys and renal vessels, bladder, ureters and urethra are also described as congenital causes.
Acquired causes include:
- atherosclerosis in the renal artery basin (statistically the most common cause);
- prolapse of the kidney (nephroptosis);
- an abnormal connection between the renal artery and vein, formed, for example, due to injury;
- arterial inflammation;
- mechanical pressure on the artery (by a growing tumor, cyst, hematoma, etc.).
It should be noted that the two most common causes, one congenital and one acquired (see above), together account for up to 98-99% of renovascular hypertension.
As for renin itself, its secretion and subsequent regulatory role represent a complex endocrine cascade, which involves protein precursor compounds, two forms of angiotensin, angiotensin-converting enzyme (ACE), and aldosterone (a hormone of the adrenal cortex). It is obvious that any failure in this multi-stage process, any damage or injury to secretory and/or receptor cells can cause endocrine imbalance and, accordingly, an excess of vasopressor hormones. Hypersecretion of renin may be a response to a purely mechanical reduction in the vasculature (blood supply) of the kidneys, however, the water-electrolyte balance is also grossly disturbed during inflammatory processes in the kidneys - glomerulo- and pyelonephritis, which leads to an excess volume of blood pumped by the heart and, as a consequence, to hypertension ( for example, bilateral pyelonephritis is accompanied by arterial hypertension in more than 40% of cases).
Visit our Cardiology page
Stages of development
Renovascular hypertension can be a consequence of damage to one or both kidneys at once. A permanent increase in pressure is characterized as a benign or malignant process.
Benign renovascular hypertension is said to occur when the pathology develops gradually, smoothly, without pronounced symptoms. In this case, the tonometer readings will change as follows: the systolic level is increased to moderate limits (130-140), while the diastolic level reaches significant high levels (up to 110 inclusive). The clinical picture is complemented by shortness of breath, general weakness, and chronic fatigue.
If we are talking about malignant renovascular hypertension, then in this case we can note a sharp deterioration in the patient’s well-being. It manifests itself with the following symptoms: excruciating headache with attacks of nausea and even vomiting, severe dizziness, decreased vision. The lower pressure rises to 120.
There are three main stages in the development of renal hypertension:
- The stage of complete compensation of pathological disorders in blood vessels.
- The stage of partial compensation, when signs of renovascular hypertension appear, which is difficult to respond to therapeutic intervention; the damaged organ begins to shrink to a small size, and the amount of urine excreted decreases.
- The stage of lack of effective compensation, the pressure remains constantly at a high level, the treatment does not give any effect, significant swelling appears in the tissues of the organ, the kidney decreases even more in volume and almost does not function.
Renovascular hypertension, characteristic of the last stage, requires emergency measures to eliminate it. Otherwise, the consequences can be very sad, even fatal.
3. Symptoms and diagnosis
There are some symptoms that are very characteristic of nephrogenic hypertension, but none of them are pathognomonic (characteristic of only one disease and not found in others). Thus, there are sharp and sudden increases in pressure against the background of normal heart rate, therapeutic resistance to conventional antihypertensive treatment (even intensive). However, in general, the symptoms can correspond to any form of arterial hypertension, so diagnosis in this case usually requires the involvement of several related specialists (cardiologist, vascular surgeon, endocrinologist, always an ophthalmologist, etc.). The primary task is to differentiate the renoparenchymal form of hypertension from the renovascular one. The anamnesis is carefully studied, examination, auscultation and percussion are performed, and a detailed and multifaceted laboratory examination is carried out. Of the instrumental diagnostic methods, the most informative are ultrasound, MSCT, various types of contrast urography and angiography (X-ray examination of blood vessels), kidney scintigraphy, radioimmunoassay of renin concentration in the blood, captopril test, etc. It should be noted that if a parenchymal form of renal hypertension is suspected, X-ray examinations should be prescribed with great caution and strictly according to indications, since both radiation exposure and X-ray contrast agents can aggravate damage to renal tissues and structures.
About our clinic Chistye Prudy metro station Medintercom page!
Differences between the renovascular type of pathology and the classical one
To make it clearer how renovascular hypertension differs from essential (classical) hypertension, you need to talk about the features of this form of the disease:
- characterized by stable upper blood pressure (BP) levels of 120–240 mmHg. Art. and lower 100–160 mm Hg. Art.;
- manifests itself at a young age in patients aged 20–45 years;
- Diagnosed in women 5 times more often than in men;
- the symptoms of the disease are not eliminated by taking antihypertensive drugs;
- in 30–60% of cases it becomes malignant;
- rarely causes the development of hypertensive crises - 3 times less often than arterial hypertension of the classical form;
- Due to the developing oxygen starvation of the kidneys, pain in the lumbar region appears.
Another difference between the renovascular form of hypertension is that it occurs against the background of an underlying disease or as a result of a defect in the renal vessels. The pathology appears suddenly at high diastolic (lower) pressure levels - 100–120–160 mm Hg. Art., while the difference between systolic and diastolic pressure is small, up to 20–30 mm Hg. Art.
4.Treatment
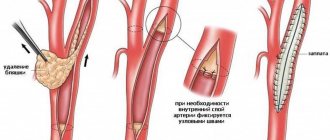
As statistical analysis of the data accumulated in the world shows, conservative methods (medication, nutrition, etc.) are much less effective than active therapy and can only be used as auxiliary, preoperative, supportive measures, as well as palliative treatment in the presence of contraindications to surgical intervention. Surgical correction of renal arterial hypertension in most cases brings a lasting and pronounced positive result and significantly increases the life expectancy of such patients. Abdominal, endoscopic or percutaneous surgery is performed (depending on the clinical characteristics of a particular case) to restore the patency of stenotic arteries, eliminate congenital defects, or completely remove the affected and non-functioning kidney, which in some cases is the only effective answer. Approximately one third of patients may no longer take maintenance antihypertensive drugs.
Palliative antihypertensive therapy as an alternative to surgery, however, is also characterized by fairly high efficiency (although we can only talk about constant drug control of blood pressure) and allows one to normalize blood pressure to one degree or another in more than 90% of cases.
Further reading[edit]
- Advances in the research and treatment of renal hypertension: 2012 edition: ScholarlyPaper. Scientific publications. 2012-12-26. ISBN 9781481636018.
- Textor, Stephen S. (2009). "Current approaches to renovascular hypertension". Medical clinics of North America
.
93
(3): 717–32, Contents. DOI: 10.1016/j.mcna.2009.02.012. PMC 2752469. PMID 19427501. - Mehta, Ankit N.; Fenves, Andrew (2010). "Current views on renovascular hypertension". Progress
.
23
(3): 246–9. DOI: 10.1080/08998280.2010.11928627. PMC 2900976. PMID 20671820.
Complications of renovascular hypertension
Renal hypertension is a dangerous condition, especially a malignant form of pathology. A prolonged increase in pressure entails irreversible changes in the main organs; in acute cases, it is necessary to take urgent measures to help the patient. Sometimes the minutes count. Failure to promptly receive emergency treatment can cost a person his life or lead to disability.
The severe consequences of a sustained rise in pressure include the following:
- damage to the visual organs leading to loss of vision (hemorrhage in the retinal area, retinal detachment);
- acute and chronic heart failure;
- myocardial infarction;
- cerebral hemorrhage, swelling and hypoxia of brain tissue, leading to stroke;
- renal failure.
To prevent dangerous conditions, timely diagnosis of the disease, which serves as a platform for the development of renovascular hypertension, is necessary.