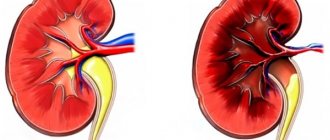
Arterial disease, known as atherosclerosis obliterans, is the irreversible growth of low-density lipoprotein plaques under the inner lining of the arteries.
The term “obliteration” means the gradual complete closure of the lumen of a vessel with the development of ischemia of organs and tissues where blood stops flowing. It reflects the most severe variant of the course of the atherosclerotic process with damage to large and medium-sized arteries. Such vessels include: the aorta, arteries of the kidneys, abdominal cavity, upper and lower extremities.
In medical practice, the diagnosis is more common when describing circulatory disorders in the legs, although it is possible to develop atherosclerosis in an obliterating form in the arms, in the renal and mesenteric arteries.
What does the ICD say?
The International Classification of Diseases (ICD-10) does not have a characteristic name for the disease. It is taken into account in the class “Diseases of the heart and blood vessels”, in the subclass “Diseases of the arteries”, in the group “Atherosclerosis” with code I70.
For atherosclerosis of the vessels of the extremities, the general code I70.2 is established. Separate codes take into account lesions of the renal, mesenteric and other peripheral arteries.
Obliterating atherosclerosis of the arteries of the legs is most clearly and often manifested. Let's consider the reasons for its development, possible approaches to diagnosis and treatment.
Healthy lifestyle, proper nutrition and diets
Diet is a fundamental principle in the prevention and treatment of dangerous vascular pathology.
The main principle of rational nutrition is to minimize the intake of cholesterol and animal fats with food.
If you have obliterating atherosclerosis or if there is a high risk of its development, it is strictly forbidden to use :
- fat meat;
- smoked meats;
- sausages;
- canned food;
- offal;
- high fat dairy products;
- fast food dishes;
- baked goods and sweets;
- margarine;
- butter;
- factory sauces.
Advice! Allowed foods include dietary meat (rabbit, veal, chicken), sea fish, cereals, vegetable soups, vegetables and fruits, shortbread cookies, low-fat dairy products, nuts and eggs (2-3 per week).
Why does this form of atherosclerosis develop?
The reasons for the development of obliterating atherosclerosis of the legs include general factors that accelerate the atherosclerotic process, negatively affect the level of cholesterol in the blood, and typical conditions for damage specifically to the vessels of the lower extremities.
General factors:
- age-related characteristics - it has been established that in people over 40 years of age, immunity is significantly reduced due to the cessation of the activity of the thymus gland, this allows infectious agents to easily destroy the arterial wall, the help of cholesterol in “patching holes” becomes excessive and causes deposits in the form of plaques;
- the greatest changes in men are associated with the protection of the female body by sex hormones and changes during pregnancy;
- nicotine intoxication in smokers promotes spastic contractions of the vascular bed and disrupts the regulation of tone by the nervous system;
- stress, uncontrollable situations, stressful working conditions, nervous breakdowns lead to an increased role of arterial spasm;
- poor nutrition causes an excess intake of fats and light carbohydrates, which are not processed into energy, but are stored as excess weight or increase the level of cholesterol derivatives in the blood, from which plaques are built;
- passive sedentary lifestyle;
- presence of concomitant diseases (hypertension, diabetes mellitus);
- hereditary predisposition.
Local factors contributing to damage to the blood vessels of the legs include:
- frequent hypothermia, frostbite of the legs;
- wearing tight shoes that impede blood supply;
- previous injuries (bruises, fractures).
Causes
The main cause of atherosclerosis is smoking. The nicotine contained in tobacco causes the arteries to spasm, thereby preventing blood from moving through the vessels and increasing the risk of blood clots in them.
Additional factors that provoke atherosclerosis of the arteries of the lower extremities and lead to an earlier onset and severe course of the disease:
- increased cholesterol levels due to frequent consumption of foods rich in animal fats;
- high blood pressure;
- excess weight;
- hereditary predisposition;
- diabetes;
- lack of sufficient physical activity;
- frequent stress.
Frostbite or prolonged cooling of the legs suffered at a young age of frostbite can also be a risk factor.
Mechanism of arterial damage
All of these reasons disrupt fat metabolism, namely the accumulation of low-density lipoproteins and triglycerides. These substances are normally carriers of molecules, but during illness they change, binding to antibodies, becoming accumulations of unnecessary reserves in cells.
The process intensifies with diabetes, hypertension, decreased thyroid function, gout, during menopause, and under the influence of stressful situations.
The other side is impaired utilization of lipoproteins by the liver. This depends on the loss of sensitivity of hepatocyte cells to the changed complexes. Nerve endings (receptors) do not recognize them, so they are not accepted for processing.
Heredity is explained by mutation of genes that control the fat metabolism of cholesterol compounds.
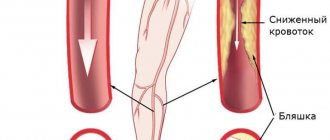
What do diseased leg arteries “look like” from the inside?
Plaques form more often in places of greatest blood flow pressure, in the area of vascular branches. From the inside, the artery wall is yellowish in color, dense, elasticity is lost, deformation and deposition of calcium salts are possible.
The femoral and popliteal arteries have five types of lesions according to location and extent:
- type 1 - limited areas of narrowing (occlusion) in individual segments;
- type 2 - widespread changes in the entire surface of only the external femoral vessel;
- type 3 - widespread occlusion of the external femoral and popliteal arteries, but preservation of patency at the site of the fork of the popliteal branch;
- type 4 - obliteration of the superficial femoral and popliteal arteries in combination with the level of the fork of the popliteal branch, but with preserved patency of the deep femoral artery;
- type 5 is the most severe lesion, since there is narrowing at the level of the superficial, deep femoral and popliteal arteries.
In combined lesions of the arterial vessels of the leg with the popliteal, 3 types are distinguished:
- type 1 - with complete obliteration of the popliteal segment and the initial parts of the tibial arteries, patency in the middle and lower part of the leg is preserved;
- type 2 - narrowing at the level of one or two arteries of the leg, but there is blood flow in the lower part of the popliteal and tibial arteries;
- type 3 - patency is preserved only at the level of small branches on the legs and feet.
Progressive atherosclerosis causes ulceration of the plaque with tissue breakdown. The detached masses migrate to more distant areas of the legs, cause thrombosis, and impair blood circulation.
Another outcome is the formation of an aneurysmal sac, thinning of the wall and internal bleeding from the damaged vessel.
Obliterating atherosclerosis
Obliterating atherosclerosis
| Obliterative atherosclerosis – occlusive-stenotic damage to the arteries of the lower extremities, leading to circulatory failure of varying severity. Obliterating atherosclerosis is manifested by chilliness, numbness of the feet, intermittent claudication, pain, and trophic disorders. Surgical methods include prosthetics , endarterectomy , thromboembolectomy , balloon angioplasty , and bypass surgery . |
- Obliterating atherosclerosis is a chronic disease of peripheral arteries, characterized by occlusive lesions and causing ischemia of the lower extremities. In cardiology and vascular surgery, obliterating atherosclerosis is considered as the leading clinical form of atherosclerosis (the third most common after ischemic heart disease and chronic cerebral ischemia). Obliterating atherosclerosis of the lower extremities occurs in 3-5% of cases, mainly in men over 40 years of age. Occlusive - stenotic lesions often affect large vessels ( aorta , brachiocephalic trunk , common carotid , iliac arteries ) or medium- sized arteries ( vertebral orifices , tibial , femoral ). In obliterating atherosclerosis of the arteries of the upper extremities the subclavian artery usually affected .
Stenosis of the arteries by more than 70% of the normal diameter leads to a change in the nature and speed of blood flow .
Factors predisposing to the occurrence of obliterating atherosclerosis :
- smoking,
- alcohol consumption,
- elevated blood cholesterol levels,
- hereditary predisposition,
- insufficient physical activity,
- nervous overload, menopause.
Obliterating atherosclerosis often develops against the background of existing concomitant diseases - arterial hypertension , diabetes mellitus ( diabetic macroangiopathy ), obesity , hypothyroidism , tuberculosis , rheumatism .
Local factors contributing to occlusive-stenotic damage to the arteries include previous frostbite and leg injuries. Almost all patients with obliterating atherosclerosis have atherosclerosis of the vessels of the heart and brain.
The appearance of plaques on the walls of the internal carotid arteries is fraught with dire consequences. Plaques are sites where blood clots form. This leads to complete blockage of the lumen of the arteries. A so-called ischemic stroke occurs. In addition, thromboembolism may develop. This condition occurs when a small blood clot breaks off from an atherosclerotic plaque, blocking the arteries of the brain. When blockage of small-caliber arteries occurs, a transient ischemic attack develops.
Classification of obliterating atherosclerosis
During obliterating atherosclerosis of the lower extremities, there are
4 stages:
- 1 – pain-free walking is possible over a distance of more than 1000 m. Pain occurs only during heavy physical activity.
- 2a - pain-free walking at a distance of 250-1000 m.
- 2b - pain-free walking at a distance of 50-250 m.
- 3 – stage of critical ischemia. The pain-free walking distance is less than 50 m. Pain also occurs at rest and at night.
- 4 – stage of trophic disorders. Areas of necrosis appear on the heel areas and on the toes, which can subsequently cause gangrene of the limb.
Taking into account the localization of the occlusal - stenotic process the following are distinguished :
- obliterating atherosclerosis of the aorto-iliac segment,
- femoropopliteal segment,
- popliteal tibial segment,
- multi-storey arterial damage. Based on the nature of the lesion, stenosis and occlusion are distinguished.
According to the prevalence of obliterating atherosclerosis of the femoral and popliteal arteries V types of occlusive - stenotic lesions are distinguished :
- I – limited (segmental) occlusion;
- II – widespread lesion of the superficial femoral artery;
- III – widespread occlusion of the superficial femoral and popliteal arteries; the area of trifurcation of the popliteal artery is passable;
- IV – complete obliteration of the superficial femoral and popliteal artery, obliteration of the fork of the popliteal artery; the patency of the deep femoral artery is not impaired;
- V - occlusive-stenotic lesion of the femoral-popliteal segment and deep femoral artery.
Variants of occlusive - stenotic lesions of the popliteal - tibial segment with obliterating atherosclerosis are represented by type III :
- I — obliteration of the popliteal artery in the distal part and the tibial arteries in the initial parts; patency of 1, 2 or 3 arteries of the leg is intact;
- II - obliteration of the arteries of the leg; the distal part of the popliteal and tibial arteries are patent;
- III - obliteration of the popliteal and tibial arteries; individual segments of the arteries of the leg and foot are patent.
Symptoms of obliterating atherosclerosis
The initial manifestations of obliterating atherosclerosis include chilliness and numbness in the feet, increased sensitivity of the legs to cold, “crawling goosebumps”, burning of the skin. Pain soon appears in the calf muscles when walking long distances, which indicates vasoconstriction and a decrease in blood supply to the tissues. After a short stop or rest, the pain subsides, allowing the patient to resume movement. Intermittent claudication or peripheral ischemia syndrome is the most constant and early sign of obliterating atherosclerosis.
With Leriche syndrome - atherosclerotic changes in the aorto-iliac segment, pain is localized in the muscles of the buttocks, thighs, and lumbar region. In 50% of patients, occlusion of the aortoiliac segment is manifested by impotence .
Tissue ischemia in obliterating atherosclerosis is accompanied by a change in the color of the skin of the lower extremities: at the beginning of the disease, the skin becomes pale or ivory; in the late stages of obliterating atherosclerosis, the feet and fingers acquire a purple-bluish color. There is atrophy of the subcutaneous tissue, hair loss on the legs and thighs, hyperkeratosis, hypertrophy and layering of the nail plates. Signs of impending gangrene are the appearance of non-healing trophic ulcers in the lower third of the leg or foot . The slightest damage ( bruises , scratches , abrasions , calluses ) of an ischemic limb can lead to the development of skin necrosis and gangrene .
In acute form of obliterating atherosclerosis (14%), obstruction of the artery site rapidly increases, trophic disorders develop rapidly and rapidly, up to gangrene. Patients require urgent hospitalization and limb amputation . _
In approximately 44% of patients, the clinical picture of obliterating atherosclerosis develops subacutely and occurs with recurrent seasonal exacerbations. In this case, a course of inpatient and outpatient treatment is carried out, which allows to slow down the progression of obliterating atherosclerosis.
The chronic form of obliterating atherosclerosis proceeds relatively favorably : due to the well-preserved patency of the great vessels and the developed collateral network, there are no trophic disorders for a long time. With this clinical variant, outpatient treatment provides a good therapeutic effect.
Diagnosis of obliterating atherosclerosis
The algorithm for diagnostic examination of a patient with suspected obliterating atherosclerosis includes:
- consultation vascular surgeon ,
- determination of pulsation of the arteries of the extremities , measurement of blood pressure with calculation of the ankle - brachial index ,
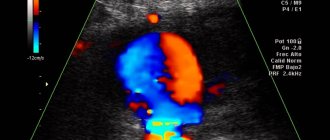
- Doppler ultrasound ( duplex scanning ) of peripheral arteries ,
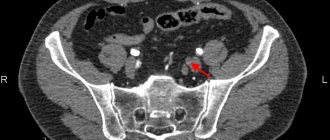
- peripheral aorto-arteriography ,
- MSCT - angiography and MR - angiography
Treatment of obliterating atherosclerosis
- medicinal
- physiotherapeutic
- sanatorium
- angiosurgical treatment
To slow down the progression of atherosclerotic changes in the arteries , it is necessary to eliminate risk factors - correction of arterial hypertension , disorders of carbohydrate and lipid metabolism , quitting smoking , preventing foot injuries , hygienic and preventive foot care , wearing comfortable shoes .
Drug treatment of obliterating atherosclerosis is carried out with drugs that reduce erythrocyte aggregation (infusions of rheopolyglucin, rheomacrodex, pentoxifylline), antithrombotic drugs (aspirin), antispasmodics (papaverine, xanthinol nicotinate, no-spa), and vitamins. To relieve pain, analgesics, paranephric and paravertebral blockades are used.
In case of acute occlusion (thrombosis or embolism), the administration of anticoagulants (subcutaneous and intravenous heparin) and thrombolytics (intravenous streptokinase, urokinase) is indicated.
Physiotherapeutic treatment:
- hyperbaric oxygenation,
- physiotherapeutic (electrophoresis, UHF, magnetic therapy, interference therapy)
- balneological procedures (hydrogen sulfide, pine, radon, pearl baths; mud applications),
- ozone therapy,
- ILBI.
When trophic ulcers form , dressings are performed with topical preparations .
Surgical treatment of stage 2-3 obliterating atherosclerosis can be carried out through endovascular or open interventions .
Methods of revascularization the lower extremities include
- dilatation / stenting of affected arteries ,
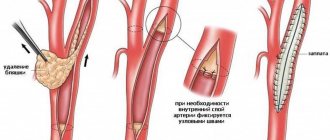
- endarterectomy,
- thromboembolectomy,
- bypass operations ( aorto - femoral , aorto - iliac - femoral , ilio - femoral , femoral - femoral , axillary - femoral , subclavian - femoral , femoral - tibial , femoral - popliteal , popliteal - foot bypass ),
- prosthetics ( replacement ) of the affected vessel with a synthetic prosthesis or autovenous
Palliative interventions for obliterating atherosclerosis are carried out when radical surgical treatment is impossible and are aimed at strengthening collateral circulation in the affected limb. These include lumbar sympathectomy, revascularizing osteotrepanation, periarterial sympathectomy, etc.
At stage 4 of obliterating atherosclerosis, amputation of a limb to an optimal level that takes into account the boundaries of ischemic disorders most often indicated .
The least invasive method of surgical treatment peripheral artery disease is the technique of angioplasty and stenting . It is used if large arteries have been damaged. Angioplasty involves inserting a flexible catheter into the arterial lumen through the femoral vein. After this, a conductor is inserted, delivering a special balloon to the place where the vessel is narrowed. By inflating the balloon, the normal lumen of the vessel is restored.
In more serious cases, arterial bypass surgery . For this purpose, an additional vessel is created. Blood flow passes through it, bypassing the affected area of the artery. Both artificial prostheses and the patient’s veins are used for the shunt.
The endarterectomy method involves surgical removal of the atherosclerotic plaque. To do this, you need to open the artery. However, it is important to consider that such a procedure may disrupt the overall blood flow through the artery. Consequently, the advisability of using endarterectomy is determined taking into account the location of the lesion and the degree of disruption of blood flow in a particular artery.
The absolute indications for surgical treatment are :
1. Chronic critical limb ischemia with patent arteries of the leg .
2. Aneurysm with threat of rupture .
3. Hemodynamically significant (> 60%) stenosis of the internal carotid artery or ulcerated plaque in the presence of symptoms of cerebral ischemia .
4. Embolism , thrombosis or vascular injury with decompensation of blood circulation in the limb .
Other indications for surgery , such as intermittent claudication corresponding to stage II b , sharply reducing the quality of life and not correctable by other treatment methods , asymptomatic stenosis the carotid arteries more than 60%, small abdominal aortic aneurysms , etc. , are considered relative and determined the general condition patient and the capabilities of the medical institution .
Contraindications to surgical treatment :
- wet gangrene with septic condition ,
- the presence of severe dysfunction of vital organs that makes surgical intervention impossible ( myocardial infarction , cerebrovascular accident , heart failure , low coronary circulatory reserve , respiratory , renal , liver failure )
Endarterectomy , as a rule, is performed on patients with segmental arterial occlusions not exceeding 7–9 cm in length. Open endarterectomy is performed within the arteriotomy wound and involves removing the altered intima along with plaques and mural thrombi.
Endarterectomy can be performed in a semi-closed manner: the obliterating masses are peeled off and removed using long vascular rings or other devices. With a significant spread of the occlusive process and severe calcification, endarterectomy is ineffective. In these cases, shunting of the affected segment , the purpose of which is to restore blood flow bypassing the affected area. Prosthetics are performed in patients who require resection of the altered vascular wall.
For occlusive lesions the branches of the aortic arch open endarterectomy most often performed from the common and internal carotid arteries or from the mouth of the vertebral artery .
Carotid endarterectomy , the operation of choice for atherosclerotic lesions of the carotid arteries, has become the standard of preventive surgery.
The surgical operation consists of removing the atherosclerotic plaque. The operation is performed under anesthesia. Its essence is to dissect the tissue above the carotid artery, isolate the vessel, dissect the wall of the carotid artery, and remove the plaque. After this, the vessel is sutured.
This operation is more traumatic, usually takes longer, is performed under anesthesia and carries more complications. The sutures are removed on the 7th day, patients are discharged with a normal course of the postoperative period on the 9-10th day. According to modern international requirements, the level of complications in a clinic where such operations on the carotid arteries are performed should be no higher than 5%. This means that 5 out of 100 patients experience various complications. The operation is contraindicated in the presence of serious somatic diseases (diabetes mellitus with high sugar levels, arterial hypertension, etc.)
Possible postoperative complications of carotid endarterectomy
As with any other surgical operation, complications are possible after carotid endarterectomy. the most serious of these is stroke. The risk of its development is 1–3%. In addition to stroke, there is a complication such as repeated blockage of the carotid artery, called restenosis . It most often occurs in those patients who have not given up smoking. The risk of developing restenosis is 2-3%. Another complication is nerve damage, which leads to voice disturbance (hoarseness), difficulty swallowing, and numbness in the face or tongue. Usually these complications do not require special treatment and resolve on their own within a month.
In case of occlusion of the subclavian artery, leading to the development of subclavian steal syndrome, the operation of choice is carotid - subclavian bypass or resection of the subclavian artery with implantation into the common carotid .
In case of widespread damage to the main arteries of the aortic arch (brachiocephalic trunk, common carotid), their resection with prosthetics or bypass surgery .
open endarterectomy is also most often performed ; in case of widespread damage bypass surgery ( prosthetics is performed .
In the treatment of occlusive lesions of the abdominal aorta and arteries of the lower extremities, the most popular operations are aorto - femoral ( iliac - femoral ) bypass and femoral - popliteal ( femoral - tibial ) bypass . In the aortofemoral position, the most widely used are synthetic prostheses made of fluorlon-lavsan, dacron and polytetrafluoroethylene (PTFE), the five-year patency of which is 85–90%.
| Endoprosthetics at aneurysm peripheral arteries – a method of minimally invasive X-ray surgical treatment of local asymmetric bulging of the arterial wall by installing an intravascular endoprosthesis. Aneurysms of peripheral arteries are a consequence of inflammatory, atherosclerotic, traumatic changes in the walls of the arteries. The endoprosthesis is installed into the lumen of the peripheral artery using the X-ray endovascular method using a special delivery catheter. After implantation of the endoprosthesis, the aneurysmally altered wall is isolated from the blood flow and is not subject to pressure, which eliminates the rupture of the aneurysm. |
Nowadays, reconstructive surgery of the abdominal aorta, carotid arteries, arteries of the lower extremities with atherosclerosis is considered one of the most developed sections of angiosurgery. Despite this, the results of the operations are still far from perfect. The frequency of early postoperative thrombosis of grafts or reconstructed arteries can be 4–13 % , late reocclusions – 8.5–30 % for the aorto - iliac and 22–60 % for the femoral - popliteal segments . In 10% of patients, attempts at reconstructive surgery end in amputation of limbs in the early postoperative period .
Throughout the world, the last decade has been a time of rapid development of X-ray endovascular surgery - one of the highest priority areas. The endovascular technique has emerged as a beneficial alternative to open surgery.
Intravascular ( endovascular ) stents are intraluminal retention devices that look like a thin mesh of metal threads that are strong enough to withstand the resistance of the arterial wall and maintain good patency of the recanalized area .
Preoperative preparation and postoperative management of patients usually carried out according to the following scheme .
The day before stenting, ticlid is prescribed at a dose of 500 mg/day. During the intervention, rheolytics and anticoagulants are administered, symptomatic therapy is carried out (antispasmodics, atropine); After the intervention, patients receive low molecular weight heparin (fraxiparin 0.3–0.6 2 times a day for 3 days), symptomatic therapy continues for 3–5 days. Patients are discharged 3–7 days after surgery. Patients take antiplatelet agents (ticlid or plavix, and in some patients aspirin) for at least 1 month. after the intervention.
According to indications ( if thrombosis or restenosis is suspected in stenting area or if lesions of previously unoperated arteries are detected ) , CTA and / or control angiography is performed .
If these changes are detected , multiple repeated endovascular interventions can be successfully used , thereby significantly delaying the time when a patient with progressive occlusive lesions will require traditional surgical intervention , or avoiding it altogether .
The range of diseases that are subject to minimally invasive treatment in the first place :
l Lesions of an isolated nature ( segmental stenoses , short occlusions ;
l Lesions that are difficult to access for open surgical interventions ( renal arteries , branches the aortic arch , visceral arteries );
l Restenosis after traditional operations , stenosis of vascular anastomoses ;
l Severe concomitant diseases that increase the risk of traditional operations .
Complicated ( embolic-dangerous ) atherosclerotic plaques , as well as a combination of stenotic lesions of the carotid arteries with kinks , tortuosity and looping , accompanied by significant lengthening of the artery and requiring traditional reconstructive surgery are considered a contraindication to stenting .
Stenting of the vertebrobasilar arteries has proven itself in surgical practice and is already the method of choice . Balloon angioplasty and stenting are indicated for stenosis and occlusion of the proximal part of the subclavian artery, accompanied by significant compromise of the vertebrobasilar blood flow, up to the development of steal syndrome, and damage to the brachiocephalic trunk.
Stenting of the arteries of the lower extremities is indicated in patients starting from stage II of ischemia according to the Fontaine-Pokrovsky classification. The ideal type of lesion for stenting is a short concentric stenosis or an isolated occlusion of less than 5 cm in length for the iliac artery and less than 10 cm in length for the superficial femoral artery. The most commonly performed stenting is the iliac, superficial femoral, and popliteal arteries.
In the late postoperative period, due to the progression of atherosclerotic changes in the proximal or distal vascular bed, repeated stenting is possible. Stenting can be used for anastomotic stenoses after previously performed bypass operations. Renal artery stenting is the most advantageous location
Preparation for carotid artery stenting surgery
Typically, preparation for carotid stenting involves taking aspirin a week before surgery. This is necessary to reduce blood clotting.
Are you a candidate for carotid stenting ?
Currently, carotid stenting surgery is indicated for patients at high risk of complications from endarterectomy. Indications for carotid stenting include significant narrowing (60%) of the lumen of the carotid arteries, symptoms of microstroke and stroke. If you do not have any symptoms, the indications for stenting are significant narrowing (80%) of the lumen of the carotid arteries and a high risk of complications from endarterectomy. In addition, carotid stenting is indicated for patients who have previously undergone endarterectomy in cases of recurrent narrowing of the arterial lumen.
Carotid stenting is not recommended for :
- Presence of abnormal heart rhythm
- Allergy to drugs used during the procedure
- Brain hemorrhages within the previous 2 months
- Complete blockage of the carotid artery
Risk factors for complications of carotid stenting
- High blood pressure
- Allergy to
Clinical manifestations, classification of the disease
Symptoms of obliterating atherosclerosis depend on the degree of vasoconstriction and the severity of the disease. In accordance with these signs, clinical stages are distinguished.
Initial (asymptomatic) - from the name it is clear that the patient does not present any complaints, considers himself a healthy person, but a blood test reveals an increase in lipid levels.
Stage of primary signs. The following symptoms are of concern:
- numbness (patients say “as if my leg was sitting”);
- constant chilliness of the feet;
- rarely – muscle cramps;
- unexpressed pain in the legs.
Stage of clinical manifestations. Complaints:
- severe pain in the legs, worsening when walking and causing limping;
- the skin on the feet and legs is pale and cold;
- ulcers or non-healing wounds on the toes may appear.
Unlike endarteritis (thrombangitis), there is no such pronounced intermittent claudication, the pain is constant.
Stage of trophic disturbances. Manifestations:
- severe pain;
- atrophy of the muscles of the leg and thigh;
- trophic ulcers on the feet;
- the onset of gangrene.
The symmetry of the lesion is more typical of atherosclerosis
What should you expect after angioplasty and stenting?
After the operation, hospitalization is required for at least a day. During this time, specialists will monitor your health, especially your blood pressure and heart rate. It is very important not to move the limb where the puncture was made, as this may cause bleeding. Usually there are no complications, but in extreme cases the patient experiences the following symptoms:
- Pallor of the limb.
- Acute pain syndrome.
- Hematoma and swelling in the puncture area.
- Bleeding.
- Numbness and freezing of the limb.
If complications occur, you should immediately notify medical personnel.
During the rehabilitation period, it is advisable to drink more water to cleanse the body. Aerobic and anaerobic exercise is completely prohibited. You can only perform physical therapy and a narrow range of exercises prescribed by your doctor. In addition, blood thinners are taken (this is necessary to prevent the formation of blood clots). It is advisable to regularly undergo a general blood test and coagulogram during recovery to avoid serious complications.
Diagnostics
Diagnosis of different stages of the disease usually does not cause difficulties for the doctor. Cold sweaty foot, decreased pulsation in the dorsal artery, muscle atrophy and trophic changes are beyond doubt.
In the clinic, therapists together with surgeons deal with the problems of atherosclerotic lesions of the blood vessels of the legs. For consultation, referral to a vascular surgery center or department is possible.
In addition to blood tests for cholesterol and lipoproteins, as well as glucose levels, the doctor needs to assess the degree of patency of the arteries.
For this use:
- angiography with the introduction of a contrast agent into the femoral artery - the technique is performed in a hospital setting;
- Vascular ultrasound, Doppler ultrasound in the clinic.
It is necessary to differentiate the diagnosis with obliterating endarteritis, Raynaud's disease, Monkeberg's disease, and sciatic nerve neuritis.
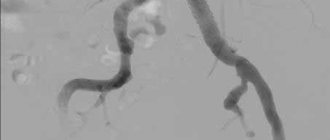
In the picture a) the radiograph shows the branches of the arteries below the knee on the right leg, color Doppler sonography b), taken from the front and back, confirms the obstruction of the vessels from the level of the middle of the shin on the left leg (S)
Raynaud's disease is more characterized by a paroxysmal nature and damage to the hands. Monckeberg's sclerosis is a rare genetic disease in which calcification of not only the peripheral but also the coronary arteries rapidly develops.
With neuritis of the sciatic nerve, the pain is shooting in nature, radiating along the outer surface of the thigh through the lower leg to the big toe. Positive symptoms of tension (Lassegue), pathological knee reflexes, increased pain when moving the spine, bending forward, and palpation at the nerve exit points are detected. There are no pulsation disorders in the arteries of the foot.
Why do they trust us and choose the CELT clinic?
- Our clinic is an expert level of cardiovascular surgery at the level of the best cardiology clinics in Europe and the world. Cardiology and cardiovascular surgery are one of the key areas of CELT.
- We have in stock almost all stents currently available on the market in Russia.
- Highly qualified doctors have more than 20 years of experience in performing endovascular operations of varying severity.
- Our specialists were the first to implant a stent in Russia - in 1993, and for a long time they were evangelists of endovascular surgery in our country, consistently proving to the cardiological community the advantages of stenting over coronary artery bypass grafting (CABG) for a wide range of indications. This is now a generally accepted fact. Most cardiovascular surgeries in Russia, as well as throughout the world, are performed using endovascular techniques.
- Many of our patients choose CELT for angioplasty and stenting operations as an alternative to treatment in Germany, Israel or the USA, not only because of the cost, which is several times lower, but also because of higher quality. It's hard to believe, but it's true!
- We perform operations even on those patients who, due to the severity of their condition, were denied coronary artery bypass grafting.
Treatment
Treatment of obliterating atherosclerosis is carried out taking into account the stage of circulatory disorders. Measures to change lifestyle and diet will be required.
- The patient is required to categorically quit smoking.
- In terms of nutrition, you will have to introduce a low-cholesterol diet with limited consumption of fatty foods, meat, and light carbohydrates.
- It is necessary to observe hygienic foot care (wash your feet twice a day, wipe with a disinfectant solution, change socks more often).
- You should wear comfortable loose shoes, use woolen socks for insulation, and avoid hypothermia. Even minor injuries (cuts, calluses, rubbing) can be dangerous.
You can read more about nutrition principles in this article.
The need for warmth is not a whim, but a real need for the patient
Medicines are conservative methods of therapy and are prescribed only by a doctor. They have to:
- cause dilatation of arterial vessels;
- promote the development of collateral (auxiliary) blood circulation;
- prevent further development of atherosclerosis;
- improve microcirculation at the tissue level.
Prevention
Lost health due to atherosclerosis is the result of your attitude towards yourself at random, therefore, already having such a disease, you must at least now be more attentive to yourself and be sure to carry out prevention. In case of OASNK, it is necessary to choose spacious, comfortable shoes to avoid calluses, bruises, avoid any injuries to the legs, and when sitting, do not cross your legs over each other, because At the same time, the vessels are pinched and the blood supply to the affected leg is disrupted. It is necessary to take walks every day; it is very good for your legs. This also includes proper nutrition with the exception of animal fats, salt, smoked meats, fried, red meat, full-fat milk, and cream.
It is necessary to normalize weight and control blood pressure - the numbers should not exceed 140/85. Reducing blood lipids will protect you from myocardial infarction; eliminating physical inactivity from your daily routine and introducing moderate physical activity will also be useful. Quitting smoking is mandatory (this alone reduces the mortality rate from 54% to 18%). It is better to avoid alcohol in any dose.
It is necessary to promptly treat any chronic diseases, control blood sugar levels, avoid stress, regularly visit a doctor for examinations, and systematically conduct courses of conservative treatment. The prognosis is determined by the presence of other forms of atherosclerosis in the vicinity: cerebral, coronary - which, of course, do not improve health.
When is the use of conservative methods justified?
Vascular surgeons warn about the danger of delaying conservative methods in the presence of severe obliteration of blood vessels and the threat of trophic changes and gangrene.
A course of drug therapy is allowed for:
- stages of chronic arterial insufficiency;
- accompanying severe diseases (myocardial and cerebral ischemia, diabetes mellitus, chronic kidney and lung diseases);
- multilevel vascular lesions with occlusion of the main and terminal arteries.
How to prevent the development of gangrene?
Obliterating atherosclerosis is one of the most common causes of gangrene and amputation of the lower extremities. Severe complications can be avoided by strictly following the recommendations for the prevention of obliterating atherosclerosis.
Additionally, you should pay attention to:
- Shoes. Properly selected shoes prevent injury and rubbing of the feet;
- Temperature outside the window. Hypothermia and frostbite are the main enemies of the lower extremities;
- Amount of sugar consumed. “Sweet” blood provokes tissue destruction and slows down wound healing;
- Wounds, cracks and other skin damage. Timely treatment of wounds and burns is the key to healthy skin;
- Physical activity. Moderate exercise improves blood supply to tissues, but excessive activity can overwork the legs and worsen the condition.
Medicines and their action
To relieve pain, use:
- painkillers;
- novocaine blockades (intraarterial, paravertebral at the level of 2–3 lumbar vertebrae).
Vasospasm is relieved with No-shpa, Halidor, Nicotinic acid, Hexonium.
To prevent thrombosis, Trental, Pentoxifyline, Agapurin, and the aspirin group are used.
In hospital settings, Trental is administered intravenously by drip, then tablets are prescribed in a maintenance dosage
Indirect anticoagulants (reduced blood clotting) are prescribed.
You can stimulate metabolism in tissues with vitamins, Solcoseryl, Parmidine, Prodectin.
The antioxidant effects of vitamins A, C, E, and Probuctol are used.
To restore protective forces, immunomodulatory drugs, ultraviolet irradiation of blood, and hemosorption are used.
Taking into account the autoimmune component in the pathology, desensitizing drugs are prescribed (Pipolfen, Diphenhydramine, Loratadine).
If the diet continues to maintain high levels of lipids in the blood, medications are prescribed to eliminate excess cholesterol.
This is what a removed blood clot looks like along with cholesterol plaques during atherectomy surgery
Surgical methods of treatment
If success with conservative therapy has not been achieved, the level of cholesterol in the blood exceeds 7.5 mmol/l, then angiosurgeons routinely offer:
- performing bypass surgery (creating a bypass for blood flow);
- vascular plastic surgery with removal and replacement with a segment of one’s own vein or alloplast;
- installation of a stent in an artery.
These techniques help restore blood circulation in the affected limb.
In case of severe changes, tissue necrosis, gangrene of the fingers, emergency amputation of the limb is necessary. The level of amputation is determined by the pattern of preserved vessels on the angiogram.
The severe consequences of the disease require patients to take a responsible attitude towards their health. Any pain symptoms in the legs should be consulted with a specialist. Treatment cannot be delayed.
How is stenting performed in CELT?
- Painless
Stenting is performed without anesthesia, since there are no nerve endings inside the vessels. - Safe
When stenting, we use radial access - inserting a catheter through the radial artery at the wrist. This approach avoids serious blood loss and is much more comfortable for the patient than access through the femoral artery. The patient can get up almost immediately after the examination; bed rest is not required. - Effective
When a vessel is narrowed or blocked, we perform balloon angioplasty and arterial stenting. A special balloon is inserted into the affected vessel, which expands the narrowing site, and then a stent is implanted.