Why do hot flashes occur, how to prevent and treat them?
Contents of the article
Hot flashes are sudden attacks of heat, most often associated with menopause or perimenopause. These two terms are basically the same in time and refer to the period during which ovarian function gradually declines.
Perimenopause begins 4-5 years before menopause, or around age 45. Menopause occurs around age 50 and marks the last menstruation of a woman's life. We can conclude that this is a complete cessation of the menstrual cycle if there has been no bleeding for a year.
Hot flashes affect not only women during menopause, but also men. Hot flashes or sudden heat waves are a very unpleasant phenomenon caused by an increase in body temperature and dilation of blood vessels in the skin, which becomes warmer and redder. The hot flash ends with severe sweating and a temporary drop in temperature. They can occur 20 to 30 times a day.
They last up to 10 minutes, during which the heart rate increases and shortness of breath occurs. After the hot flash passes, the woman's clothes become covered in sweat, which cools the body and interferes with normal daily life.
Popular questions
Hello!
Constant hot flashes tormented me. I started drinking Gynocomfort Klimafemin. It helped right away. But it turned out that it was not available in any pharmacy! It was difficult to buy only one package. Has this product been discontinued? Hello! Gynocomfort climafemin continues to be produced. You can purchase it in pharmacies that sell other VERTEX products.
Hello, I have up to 10 hot flashes per day, more at night. A year ago I took the drug Femoston 2 for three months, it helped, everything was fine for six months, but it all started again. Is it possible to correct this condition without hormonal drugs?
Hello! The Ginocomfort line of drugs includes the drug Climafemin. It contains antioxidants and phytoestrogens, which will correct the vegetative manifestations of menopause. If there is no effect after 1 month of use, you should consult your doctor again.
Hot flashes, insomnia, what to do? I take Klimanalin, it doesn’t help.
Hello! Vivid vegetative manifestations in the menopause are caused not only by hormonal changes, but also by a possible combination of thyroid pathology - hypothyroidism, vertebrobasilar insufficiency. Therefore, it is advisable: consultation with an endocrinologist or neurologist. OMT ultrasound, flora smear, cytology, which will allow prescribing menopausal hormone therapy in the absence of contraindications. At this stage, pending examination results, you can add Gynocomfort climafemin to treatment. The drug contains phytoestrogens and antioxidants, which has a beneficial effect on well-being and eliminates the symptoms of menopause. The drug is taken 1 t once a day for 3 months.
I am 49 years old and suffered from frequent hot flashes. How to prevent them?
Hello!
These are manifestations of menopausal syndrome associated with the extinction of ovarian function. At this stage, I recommend using a herbal-based drug that allows you to stop bursts of vegetative reactions - Ginocomfort Klimafemin 1 t once a day for 3 months. During this time, conduct an examination: ultrasound OMT, they say. glands, flora smear, oncocytology, oak, lipid spectrum, FSH, TSH levels. Consult a therapist and other related specialists if you have chronic diseases that would be a contraindication for prescribing menopausal hormone therapy. This will help the obstetrician-gynecologist correctly select further treatment. For an accurate diagnosis, contact a specialist
Menopausal waves
Hot flashes are most often associated with perimenopause or menopause, when there is a sudden drop in estradiol, one of the three estrogens synthesized in a woman's body.
Up to 45% of early postmenopausal women wake up every other night due to hot flashes and sweating. Two-thirds of them said they were chronically sleep-deprived as a result.
Associated with this are mental disorders that destroy quality of life through the so-called “domino effect.” Waves of nightly hot flashes and sweats lead to insomnia, which causes irritability, anxiety, depression, emotional lability, fear of aging and loss of attractiveness, and finally a drop in energy and libido.
An interesting study conducted in the US involving 60,000 women over 10 years found that women who experienced hot flashes during perimenopause and menopause were less susceptible to heart and cardiovascular disease.
Types of menopause
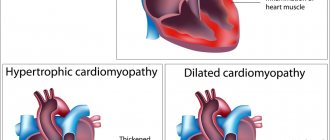
According to the age of onset, menopause can be premature (up to 40 years), early (40-45 years) and late (55-60 years).
Any such deviation from the average age of 45-55 years is considered a pathology and indicates the presence of serious diseases in the body. Pathological menopause is a condition when hormonal changes are accompanied by severe disturbances in the endocrine, cardiovascular, nervous systems and psychological state of a woman.
Artificial menopause occurs after removal of both ovaries (oophorectomy) during radical treatment of severe gynecological diseases, after chemotherapy or radiation therapy and as a result of primary ovarian failure (inability to produce estrogen).=
Duration of tides
The duration of a fever attack is difficult to determine; it is individual for each woman. For some people, hot flashes may last a very short time and soon stop completely, while for others they may continue to occur for the rest of their lives. In any case, the longer they occur, the weaker they become.
The decrease in estradiol levels is recorded mainly one to two years before menopause (the last menstrual period in life, usually around age 50) and continues into early postmenopause. In postmenopause, the period after the last menstruation, they occur in 70-80% of women of this age, and in more than half they last for more than 2-3 years.
Numerous habits or substances can contribute to hot flashes, so it is recommended:
- limit hot drinks, spicy foods, alcohol and caffeine;
- do not wear tight or synthetic clothing;
- no smoking;
- avoid stressful situations;
- Do not stay in excessively warm rooms.
The climacteric period (menopause, menopause) is a physiological period of a woman’s life, during which, against the background of age-related changes in the body, involutionary processes in the reproductive system dominate. It is characterized by a gradual decrease and “switching off” of ovarian function due to the depletion of the supply of eggs and the development of symptoms of estrogen deficiency. Up to 60–80% of peri- or postmenopausal women experience vasomotor symptoms, the onset of which begins during the transition period and reaches its peak approximately a year after menopause [1, 2].
A sudden feeling of heat in the upper body, especially on the face, neck and chest, is called a hot flash. These episodes last approximately 1 to 5 minutes and are characterized by sweating, flushing, chills, a clammy feeling, anxiety, and sometimes rapid heartbeat. Vasomotor symptoms can also disrupt sleep and cause chronic insomnia in some women [2, 3]. Hot flashes vary in frequency and duration: studies show that 87% of women experience hot flashes daily, with approximately 33% experiencing hot flashes 10 times a day or more [1]. These symptoms significantly reduce the quality of life of women and force them to seek medical help.
The pathophysiology of hot flashes has not yet been fully elucidated. It is known that hot flashes occur in women taking tamoxifen for breast cancer, after oophorectomy, as well as in hypogonadism in men during androgen blocking therapy for prostate cancer [4, 5]. It is clear that changes in the level of sex hormones play a major role and are the cause of the occurrence of vasomotor symptoms, which is confirmed by their disappearance when taking estrogen. However, a decrease in estrogen levels and a natural increase in follicle-stimulating hormone (FSH) levels through feedback mechanisms alone cannot explain the occurrence of hot flashes, as well as the variability in the severity and frequency of symptoms, since they do not correlate with the level of sex hormones. Additionally, despite low estrogen levels in postmenopause, some women experience symptoms while others do not. The main discussion is about disruption of thermoregulation processes in the hypothalamus due to estrogen deficiency, which leads to a narrowing of the thermoregulatory zone and an increase in its sensitivity to small changes in body temperature.
Moreover, back in 1979, experiments [6, 7] showed that hot flashes are closely associated with impulses of luteinizing hormone (LH) activity. Therefore, research in recent decades has been focused specifically on the central mechanisms of regulation of reproductive function. For the first time, the quintessence of accumulated knowledge on the nature of hot flashes, with an emphasis on central regulatory mechanisms, was reported at the XV International Congress on Menopause in Prague, when this article had already been accepted for publication.
In 1977, the groups of Schally and Guillemin were awarded the Nobel Prize for the discovery of gonadotropin-releasing hormone (GnRH). In 1978, E. Knobil [8] demonstrated the importance of pulsatory GnRH secretion for adequate activation of the hypothalamic-pituitary-ovarian axis (HPO-axis) during puberty and its cyclic function during reproductive age. The release of GnRH is pulsatile in nature, and it clearly correlates with pulses of LH activity in the peripheral blood [9, 10].
Feedback mechanisms continue to operate in postmenopause, so naturally, in response to a decrease in estrogen synthesis by the ovaries, the level of gonadotropins increases. Despite the well-defined role of GnRH during puberty and maintenance of adult reproductive function, little is known about how GnRH release changes during aging and whether it plays a role in the involution of the female reproductive system [11].
It is known that GnRH release in aging primates and women is not directly controlled by gonadotropin levels [12–14]. Thus, in a study by M. Woller et al. [14] showed an increase in LH pulsatile activity with aging in female monkeys. In women, gonadotropin levels were higher in early postmenopause compared to premenopause [15–17]. In addition, the pituitary gland itself can undergo aging processes, for example, changing sensitivity to GnRH, which also affects the synthesis of gonadotropins. Therefore, it is important to directly study the processes of GnRH pulsatile activity with aging. Due to the inaccessibility of GnRH neuron terminals and the inability to detect GnRH peptide in peripheral blood, it was not possible to conduct such a study in women. Experiments on macaques showed that pulsatile secretion of GnRH persisted in different age groups, but postmenopausal individuals were characterized by a significant increase in the concentration of GnRH and the presence of pulses of extremely large amplitude, while the frequency of the pulses remained the same. In one monkey, estrogen administration reduced the amplitude of pulsatile GnRH release [11].
Experiments on female monkeys also showed that the use of estrogen replacement therapy reduced GnRH release [18] and GnRH gene expression [19, 20]. Administration of estrogen to postmenopausal women leads to a decrease in LH and FSH levels, and the response in late postmenopausal women was greater compared to early postmenopausal women. This once again proves that the negative feedback between estrogens and central regulatory mechanisms is not only maintained, but even strengthened with aging [12, 21].
However, the temporal relationship between hot flashes and peaks in GnRH/LH secretion is not causal. When estrogens were prescribed and then withdrawn, hot flashes in women persisted even after surgical removal of the pituitary gland [6] or against the background of GnRH agonists, which suppress LH secretion [22, 23]. GnRH itself is also not the cause of vasomotor complaints, since hot flashes continue to occur in patients with Kallmann syndrome despite the absence of GnRH neurons [24]. Since it has been proven that LH impulses are caused by GnRH impulses, and hot flashes are timed to LH impulses, it becomes clear that the mechanism of hot flashes is closely related to the hypothalamic control of GnRH secretion.
Studies in the early 2000s demonstrated that pulsatile GnRH secretion is modulated by a subpopulation of arcuate nucleus neurons expressing estrogen receptor alpha (ERα), neurokinin-3 receptor, kisspeptin, neurokinin B, and dynorphin—the so-called KNDy neurons [25]. One of the striking discoveries of the 21st century in the field of neuroendocrinology was evidence of the participation of kisspeptin and its receptor in the initiation of puberty and the maintenance of reproductive function [26, 27]. Kisspeptin is the main stimulator of GnRH synthesis; its secretion is also pulsating in nature and clearly correlates with GnRH/LH secretion pulses: after each kisspeptin secretion pulse, a GnRH secretion pulse occurs [26, 28]. Neurokinin, together with kisspeptin, has a stimulating effect on GnRH secretion [26]. Dynorphin is an endogenous opioid peptide that mediates the negative feedback between estrogens and GnRH [29].
Kiss1 neurons of the arcuate nucleus of the infundibular region (group of KNDy neurons) participate in the negative feedback between sex steroids and gonadotropins, providing tonic secretion of GnRH, with the participation of dynorphin (suppressor of GnRH synthesis) and neurokinin B (stimulator of GnRH synthesis). They form an autosynaptic feedback loop and modulate the pulsatile secretion of GnRH and, accordingly, the synthesis of LH and FSH [30]. Kiss1 neurons of the rostral part of the third ventricle field play a key role in transmitting the positive feedback of estradiol to gonadotropins, primarily regulating the pulsatile activity of GnRH, in the presence of activated progesterone receptors, which initiates the preovulatory GnRH peak [3, 25, 31] (Fig. 1 ).
Rice. 1. Feedback mechanism in postmenopause when ovarian function is turned off and possible ways of generating hot flashes [3].
In postmenopause, KNDy neurons undergo unusual somatic hypertrophy and express increased levels of transcripts of the kisspeptin and neurokinin B genes [3, 25, 32], the expression of the Kiss1 gene in the infundibular nucleus increases, which increases the secretion of GnRH and LH [32–34]. Animal data suggests changes in postmenopausal KNDy neurons are secondary to estrogen deficiency rather than aging Per se
[3, 32].
When performing ablation of KNDy neurons in the experiment, LH secretion was naturally disrupted. In rats of the control group, ovariectomy naturally led to an increase in LH levels, and the administration of estrogen normalized it. In the main group (ablation of KNDy neurons) after ovariectomy there was no significant increase in LH levels, and it was lower regardless of estrogen administration. In addition, when KNDy neurons were ablated, rats maintained their core body temperature better [3, 25].
It is known that KNDy neurons are adjacent to structures responsible for the regulation of body temperature [3, 35–37], including the median preoptic nucleus, an important component of the thermosensory pathway for protection against overheating. Thus, connections of KNDy neurons with both preoptic structures responding to thermoregulation and with GnRH neurons explain the temporal relationship between hot flashes and pulses of LH secretion in postmenopausal women. Based on the above experiments, it can be argued that it is KNDy neurons that play an important role in the occurrence of hot flashes [3, 25].
It is known that the “gold standard” for relieving vasomotor symptoms is menopausal hormone therapy (MHT), the effectiveness of which reaches 90–95% [38, 39]. During the first 2-3 weeks of taking MHT, hot flashes stop almost completely. According to feedback mechanisms, an increase in the level of estradiol in the blood helps to reduce the hyperactivation of KNDy neurons, reduce the amplitude of pulse secretion of GnRH and the level of gonadotropins. The transmission of hyperexcitation to neighboring hypothalamic structures responsible for temperature and vasomotor manifestations stops.
It should be remembered that MHT, like any drug therapy, has its own indications and contraindications. Thus, MHT is contraindicated in women with a previous heart attack or stroke, or venous thrombosis. In addition, from the standpoint of balancing positive effects and risk profile, the world community recommends that hormone therapy be prescribed for the first time to women no older than 60 years or with menopause lasting no more than 10 years [38, 39]. However, a meta-analysis [40] of 6 studies assessing the natural history of vasomotor symptoms showed that hot flashes persisted in 50% of women 4 years after menopause, and in 10% even after 10 years. How can we help patients with vasomotor complaints who are contraindicated in MHT or for whom it is too late to start it, given that the effectiveness of herbal remedies is on average about 30%, and the effectiveness of serotonin reuptake inhibitors is 50%? Are there other mechanisms to reverse the hyperactivation of KNDy neurons?
The year 2000 was marked by a landmark event in the field of neuroendocrinology - the discovery of gonadotropin-inhibiting hormone (GnIH) [41]. In mammals, the cell bodies of GnRH-synthesizing neurons are located in the dorsomedial region of the hypothalamus, and their axons approach the median eminence and GnRH1 neurons in the preoptic nucleus. Gonadoinhibin inhibits the synthesis and release of gonadotropins due to a direct effect on pituitary gonadotrophs and causes inhibition of the activity of GnRH neurons through its receptor, and also disrupts the pulsatile secretion of GnRH in the hypothalamus [42, 43] (Fig. 2). In addition, the axons of GnIH neurons approach kiss neurons and reduce their activity. Thus, the level and pulsating rhythm of the secretion of GnRH, FSH, and LH depend on the frequency of exposure to kisspeptin and gonadoinhibin [44].
Rice. 2. Central departments for the regulation of reproductive function. The role of melatonin.
According to experiments on ovariectomized mice [45], intravenous administration of GnIH resulted in a significant decrease in plasma LH levels, and intracerebral administration did not affect either the average LH level or the frequency of pulsatile secretion. In a study [46] on cell culture, the use of GnIH did not affect basal secretion, but reduced GnRH-stimulated LH secretion by an average of 25%. In studies, it was noted, according to some authors, that it is the long-term use of GnIH that matters, since a single injection did not give any effect.
According to modern research [47], the activity of GnIH neurons is modulated by both environmental factors and internal factors. One of these factors is endogenous melatonin. In an experiment in birds, the use of melatonin increases the expression of gonadoinhibin mRNA and the release of GnIH itself in the brain. There is a subtype of melatonin receptor Mel1c on GnIH neurons of quails. Thus, melatonin directly acts on GnIH neurons to increase the secretion and release of gonadoinhibin. The release of GnIH increases during periods of short daylight hours, when nocturnal melatonin production increases [48] (see Fig. 2). The main volume of melatonin is formed in the secreting cells of the pineal gland - pinealocytes.
In 2015, the drug Pineamin was registered in Russia (Geropharm LLC). The active ingredients of Pineamin are pineal gland polypeptides PPG (Polypeptides of Pineal Gland), which restore the normal functional density of pinealocytes and stimulate the synthesis of endogenous melatonin. After intramuscular administration of the drug, PPG polypeptides enter the inferior vena cava, bypassing the portal system, enter the right heart and then into the arterial circle along the branches of the middle and posterior cerebral arteries, bypassing the blood-brain barrier, and immediately enter pinealocytes through axovasal synapses, where they activate the synthesis of melatonin and serotonin. As discussed above, melatonin stimulates the activity of GnIH neurons and the synthesis of GnIH, which in turn helps to eliminate excessive hyperactivation of KNDy neurons, GnRH neurons and adjacent parts of the median preoptic nucleus. Accordingly, the neurovegetative manifestations of menopausal syndrome are stopped.
The effectiveness of Pineamin was studied in a multicenter placebo-controlled study led by V.N. Prilepskoy et al. [49] with the participation of 120 women: Pineamin 2 course group - 60 patients, Pineamin 1 course group - 30, placebo group - 30. The study demonstrated a statistically significant decrease in the manifestations of menopausal complaints on the scale of the modified Kupperman menopausal index in comparison with the placebo group. At the same time, it was shown that the injection form of Pineamin has a high ability to retain the effect, which makes it possible to carry out repeated courses no more than 2-3 times a year.
There were no statistically significant differences in the incidence of adverse events between the groups (Pineamine; placebo): endometrial thickness according to ultrasound, and the condition of the cervix did not change.
Also, there was no statistical difference between the Pineamin and placebo groups when measuring the level of female sex hormones: estradiol, FSH, LH, prolactin.
When assessing the parameters of the blood coagulation system (fibrinogen, prothrombin index, activated partial thromboplastin time and INR), it was found that the study drug Pineamin had no effect on them and their level was within normal limits.
When assessing the biochemical parameters of the blood, it was revealed that there was no effect on lipid spectrum indicators, as well as such metabolic indicators as glucose, creatinine, alanine, aspartate transferase and bilirubin.
Thus, despite the fact that new links in the central departments of regulation of the function of the reproductive system and the main pathogenetic stages of the occurrence of vasomotor complaints have been discovered in the last two decades, today the doctor’s arsenal already has a drug with an innovative mechanism that makes it possible to relieve hot flashes with a favorable safety profile.
The authors declare no conflict
of interest .
Hot flashes outside menopause
In addition to women during menopause or perimenopause, men and women of any age can experience hot flashes. Hot flashes are not considered too negative and in most cases go away soon after we discover and prevent the cause of their formation.
Also, if you're not sure what's causing a hot flash, it's a good idea to keep notes in your cell phone or notebook/diary handy. Write down when the hot flash occurred, how long it lasted, and what you did before it hit.
Hot flashes in people without menopause can be caused by:
- medications such as antidepressants, opioid analgesics, osteoporosis medications, etc.;
- excess weight, as it disrupts metabolism;
- food allergies (write down what foods you ate before the hot flashes, if some foods are repeated, try to exclude them from your diet);
- stress and anxiety (for many people, exposure to stressful situations causes sweating, rapid heart rate and fever);
- problems with the thyroid gland and other glands that produce hormones;
- Being in a very warm room (an overheated bedroom can cause night sweats).
How to relieve menopause symptoms
A healthy lifestyle, balanced nutrition, taking vitamins and physical activity will help smooth out the symptoms of menopause and improve your emotional background. Regular sex life will help maintain prostate health. But if the symptoms of menopause worsen a man's quality of life, he may be advised to take testosterone.
If you want to preserve your men's health for as long as possible, contact Dr. AkNer, here you will be given a high-quality examination and all existing problems will be identified.
Urologist, andrologist Akopyan Nerses Grigorievich.
Back to list of articles
Treatment of hot flashes and their prevention
The ovary is the shortest-lived endocrine gland, and when it stops producing hormones, a replacement must be found.
Typically a combination of natural estrogens (most often estradiol) and progestogens is used.
Depending on the age, diseases and desires of the woman, treatment is agreed upon, which can be:
- cyclically combined (simulates the menstrual cycle);
- continuously combined (no cycle).
Usually it lasts up to 5 years, and if necessary, longer. Hormonal treatment has many benefits: it reduces symptoms such as hot flashes and night sweats, insomnia, headaches, mood swings, helps with dry and thin skin, and hair loss. It also has a protective effect on the nervous system, heart, blood vessels, atrophic changes in the female reproductive system, suppresses atherosclerosis, osteoporosis and reduces the risk of developing senile dementia.
Contraindications:
- estrogen-dependent breast cancer or a high risk of its occurrence;
- active thromboembolism;
- liver disease;
- cardiac ischemia;
- pregnancy;
- undiagnosed uterine bleeding;
- uterine fibroids and endometriosis.
What to take for hot flashes during menopause?
Most often, doctors prescribe menopausal hormone therapy (MHT) to patients. Normalizing hormonal levels by taking such drugs not only reduces sweating, but also improves psycho-emotional state, helps cope with mood swings, increases performance and optimizes concentration.
However, it must be taken into account that drugs that compensate for the lack of estrogen can activate the launch of developing oncological diseases - in particular, breast, endometrial or ovarian cancer and aggravate chronic diseases and the risk of thrombosis. Therefore, treatment with hormonal drugs should occur exclusively according to the regimen drawn up by the doctor.
In recent years, it has become possible to replace the use of traditional tablet medications with the use of hormonal patches, gel forms, and intrauterine complexes.
They are considered less dangerous in terms of the possibility of venous thrombosis.
Stages of menopause
You can talk about the onset of menopause as soon as its first symptoms appear. However, the decline of reproductive function occurs slowly and is divided into three stages:
- premenopause, when periods are still present, but the cycle becomes longer or less regular, and ovarian function decreases. These processes last about 2 years;
- menopause, when 12 months have passed since the date of the last menstruation;
- postmenopause, which is characterized by increasingly serious changes in the body and complete cessation of ovarian function.
The duration of these stages, as well as the clinical manifestations of menopause, depends on the individual characteristics of the woman, her lifestyle, general health, and heredity.