General information about pathology
The electrical activity of the body's "motor" is recorded on an ECG. To imagine what the heart axis is, you need to construct a coordinate scale and designate directions at intervals of 300. The semi-vertical position of the organ in the chest, superimposed on the coordinate system, determines the electrical axis.
The vectors form an angle, so the EOS direction is measured in degrees from -180 to +1800. The normal position should be from +30 to +69.
If, under the influence of any factors, a change in the position of the organ and the vector of signal transmission occurs, we are talking about a change in its position in the coordinate system.
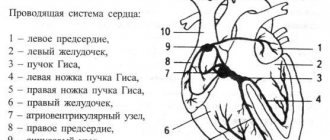
The heart generally follows sinus rhythm, and the electrical impulse begins in the atrium and then spreads to the ventricles. On the electrocardiogram you can see whether there is a P wave for atrial contraction, a QRS complex for ventricular contraction, and a T wave and their repolarization.
The position of the clamps when taking an ECG is the direction of the electrical impulse of the heart. When collecting electrodes, 3 main lines and 3 auxiliary lines are determined, as well as readings from the chest.
The axis value is normal when the R waveform is highest in the 2nd major lead and R1>. R3.
What does it mean to shift the electrical axis to the left? There are factors that cause this organ to tilt to the left. The left axis is observed if the axis position is in the range from 0 to -900.
Reasons for rejection
The EOS deviates to the left not only in cardiac pathologies. The cause of the deviations is left ventricular hypertrophy caused by the following diseases:
- heart failure;
- arterial hypertension with congestive symptoms;
- heart disease;
- left bundle branch block;
- atrial fibrillation.
In the cardiac cycle, during the first contraction, blood is pushed into the atrium, the valve closes, then goes into the ventricle, and with the next contraction, all the blood must go into the vessels.
If the pumping function is impaired, when the organ cannot compress with sufficient force to push out all the fluid, some of the fluid remains permanently in the body cavity. Gradually stretches.
This phenomenon is provoked by cardiomyopathy of coronary artery disease as a result of a heart attack, myocarditis.
The second reason for the accumulation of residual fluid: the valve does not close completely or a narrowing occurs, that is, a narrowing of the lumen of the vessel. Some of the blood then flows back or not into the aorta in one cycle.
Heart defects can be congenital or acquired. In the first case, it is detected during examination of a newborn, in the second - in an adult.
When conduction in the left bundle of His is disrupted, the function of the left ventricle is impaired and it does not contract properly. In this case, the sinus rhythm is maintained, but the axis deviates.
Hypertension causes an increase in blood pressure on the vessels, which affects their condition. The more often an increase in blood pressure occurs, the greater the likelihood of decreased vascular flexibility and ventricular dilatation, which is associated with heavy workload.
With atrial fibrillation, with the exception of changes in the electrical axis of the heart, there is no contraction of the atria, and ventricular syndromes develop at different periods of time.
Diseases accompanied by levogram
Most patients are trying to understand what it means when the electrical axis of the heart is deviated to the left and what diseases this is associated with. The most common cause is hypertension. When blood pressure is constantly elevated, the load on the left chambers of the heart muscle increases. Which leads to an enlargement of the ventricle and atrium. Accordingly, the electrical axis of the heart shifts to the left.
Acquired heart defects associated with the appearance of atherosclerotic plaques also lead to an increase in the hemodynamic load on the left ventricle. This occurs due to damage to the aortic and mitral valve.
Myocarditis leads to inflammation of the walls of the heart muscle. Accordingly, the tissues increase in volume and hypertrophy occurs. The disease can only be determined in special cardiology centers by undergoing a scintigraphic examination.
Author of the article: Yulia Dmitrieva (Sych) - In 2014, she graduated with honors from Saratov State Medical University named after V. I. Razumovsky. Currently working as a cardiologist at the 8th City Clinical Hospital in the 1st clinic.
Symptoms and manifestations
The deviation itself is not symptomatic, but since the disorder is caused by certain causes, symptoms appear when the process spreads significantly.
Hemodynamics are impaired and there are associated symptoms.
If the patient has heart failure or a heart defect, symptoms include shortness of breath when walking or climbing stairs, contusion of the limbs and nasolabial triangle, shortness of breath and dizziness.
Atrial fibrillation is manifested by attacks of shortness of breath, palpitations, chest pain and fluctuations in heart rate.
Arterial hypertension is manifested by a headache, mainly in the back of the head, a feeling of heaviness in the chest, and at high levels - flickering before the eyes.
Diseases that are accompanied by levogram
If a patient has a deviation in EOS, this may be a consequence of diseases such as:
- coronary heart disease (CHD);
- cardiopathy of various origins;
- chronic heart failure (CHF) of the left ventricular type;
- congenital heart defects;
- myocardial infarction;
- infectious damage to the myocardium.
In addition to diseases, blockage of the conduction system of the heart can result from taking certain medications.
Diagnostics
To determine the disorder, it helps to bring together the symptoms of the disorder, functional diagnostics, and other methods:
- ULTRA-HEARING;
- Holter monitoring;
- ECG;
- X-ray;
- ischemic angiography.
Thanks to these tests, it is possible to visually evaluate the organ, its cross sections, determine the size of the enlarged defect and determine the cause of failure.
The point at which myocardial ischemia occurs can be determined using weighted electrocardiography on a bicycle or exercise bike.
Your doctor will order a 24-hour test if he suspects you are suffering from the disorder. During periods of arrhythmia, the person is suspended from a machine that records the heart's contractions for one day.
Angiocoronography is a study of blood vessels, allowing you to see their condition and blood flow disorders. The scan allows you to determine the increase in the shadow of the organ, which indicates its hypertrophy.
Additional diagnostics
To find out the reasons for the EOS deviation, the ECG is analyzed in detail. They may also assign:
- EchoCG (ultrasound of the heart) - to identify possible organ defects.
- Stress echocardiography – ultrasound of the heart under stress – for diagnosing ischemia.
- Angiography of the coronary vessels - their examination to identify blood clots and atherosclerotic plaques.
- Holter monitoring – recording an ECG using a portable device throughout the day.
After a detailed examination, appropriate therapy is prescribed.
When additional examination is required
Standard EOC values are about the same for everyone, but a tall person may have a slightly different heart size and location, although they will not get sick. Therefore, if any abnormalities are detected during the initial examination, additional tests are necessary.
Changes in this parameter are also normal for athletes.
Because they exert a lot of effort during constant training, their heart pumps a large amount of fluid, causing the cavities to stretch. They may have horizontal deviations when the organ position is from -15 to +30.
If during the examination a person takes a deep breath or changes his body position, even if it is correct, a deviation of the healthy heart to the left is detected.
What does a sharp deviation mean?
Since the deflection angle can vary, the process steps also vary. Changing an academic degree is a gradual process. The more the size of the defect increases, the more the indicator deviates from the norm. If the deviation is from -450 to -900 degrees from the norm, the organ is said to be sharply shifted to the left.
In adults
A shift in the position of the heart in the chest may indicate an ECG disorder if the person is in good condition and no other health problems are detected.
Typically seen in people who exercise regularly and athletes.
The obvious deviation is not accidental; it is a sign of pathology in adults. There may be clogs that accumulate over several years.
When does the heart axis “go to the left”?
Sharp deviation of the electrical axis of the heart to the left
The conclusions of a functional diagnostics doctor about the deviation of the cardiac axis to the left are not an independent diagnosis. But they always give reason to wonder why the heart axis “went to the left.” A slight shift of the EOS to -190, as well as its semi-vertical position, in some cases is not considered a pathology. This position of the axis can be observed in healthy, tall, thin people, in athletes with a trained heart, in children with an asthenic physique, and with a high position of the diaphragm dome.
If the cardiac axis is significantly deviated to the left, then this pathological condition indicates problems with the heart; the cause of such a displacement must be established. After all, this symptom can sometimes be the first “bell” in case of pathology of the heart and blood vessels. According to some data, a deviation of the electrical axis of the heart to the left up to -29-300 is sometimes called a slight deviation, and if the angle is from -450 to -900 they speak of a sharp deviation.
In children
A child in the neonatal period has a sharp deviation of the axis to the right, this is the norm. If such a disorder is observed in an adult, he will develop symptoms of right ventricular hypertrophy.
In a child, this is due to the fact that the right side of the heart has more mass than the left side. By the age of one year, this condition is normalized, and the organ should take a vertical position in the chest. During this period, it can rotate around its axis in different directions.
The left ventricle then gains mass and is no longer attached to the chest. At the age of 6-7 years, the organ acquires the correct semi-vertical position.
Is treatment necessary?
The heart axis is a criterion by which a health disorder can be determined, therefore, if there is a deviation, therapy is aimed at combating the cause identified during diagnosis. If it is eliminated, normal heart function can be restored.
These may include the following procedures:
- installation of an artificial valve;
- pacemaker implantation;
- bypass surgery;
- prescription of antihypertensive and antiarrhythmic drugs.
The range of measures depends on the severity of the violation.
If the arrhythmia recurs and can be treated with medication, an appropriate measure is chosen. If the arrhythmia is life-threatening, a pacemaker is chosen.
Coronary bypass surgery is the cleaning of blood vessels from atherosclerotic and lipid plaques, which expands their lumen and eliminates ischemia.
For congenital and acquired heart defects or CHF, valve replacement helps restore the heart rhythm to normal. If the pumping function of the heart is impaired, poor contractility of the heart muscle remains.
Additional diagnostic methods - a set of examinations
Based on the indications of axis deviation to the left, it is impossible to reliably determine what changes are occurring in the heart muscle. Therefore, cardiologists prescribe a number of additional examinations.
- Ultrasound. Allows you to determine how enlarged the ventricles are and how their contractile function is impaired.
- Electrocardiogram with exercise (walking on a treadmill or riding an exercise bike). Allows you to detect coronary heart disease.
- Chest X-ray. If the tissue is significantly enlarged, the shadow of the heart will be larger.
- 24-hour Holter ECG monitoring. Performed in case of significant cardiac dysfunction src=”https://infoserdce.com/wp-content/uploads/2021/08/foto-7.jpg” class=”aligncenter” width=”375″ height=”510″[ /img]
- KAG. Also necessary for diagnosing coronary artery disease.
- Echocardioscopy. Allows you to fully assess the condition of all components of the heart muscle.
Possible consequences and complications
It is not the deviation of the heart position itself that is dangerous, but the reasons why it occurs. Complications of left ventricular hypertrophy:
- heart failure;
- arrhythmia;
- angina pectoris;
- heart failure.
All causes of organ dysfunction are interconnected. If a heart defect has led to an enlargement of the left ventricle, arrhythmias with the development of a pathological process should be expected. If the heart muscle becomes so weak that contraction of the fibers does not produce further blood, circulatory failure and cardiac arrest develop.