According to WHO statistics, cardiovascular diseases are among the top three causes of death. Blood clots in blood vessels are one of the main factors in the development of ischemia of the heart muscle, as well as heart attacks and strokes. That is, increased blood clotting provokes acute diseases that lead to severe, often irreversible complications and death of the patient.
Causes of bleeding disorders
- Genetic. Sometimes the blood clotting mechanism has congenital defects caused by mutations in genes. Some mutations are inherited and lead to diseases such as hemophilia.
- Medicinal. Taking drugs that affect blood clotting (aspirin and other non-steroidal anti-inflammatory drugs, anticoagulants, fibrinolytics).
- Somatic. They occur against the background of other diseases (blood diseases, liver diseases, vitamin K deficiency, massive blood loss, etc.).
Most causes of bleeding disorders require immediate treatment. To detect them, you must first do a general blood test for blood clotting. Coagulation disorders can manifest themselves in two ways: increased and decreased blood clotting. The danger of increased blood clotting is explained by the high risk of blood clots in the vessels and the deterioration or complete cessation of blood supply to a tissue or organ. Reduced blood clotting, which can be congenital or acquired, poses a particular danger during injuries and operations.
Hypocoagulation: symptoms, why the pathology is dangerous
Nosebleeds for no reason, bleeding of mucous membranes when brushing your teeth, spontaneous appearance of bruises and bleeding from your finger that you cannot stop for longer than usual - all these are still harmless signs of reduced coagulability.
The real danger awaits carriers of the pathology during surgical operations, increased blood pressure, after childbirth, and even routine tooth extraction at the dentist.
Diseases associated with blood hypocoagulation
| Name | Pathogenesis – mechanism of occurrence and development | Why is pathology dangerous? | How is it diagnosed? |
| Thrombocytopenia | A decrease in the number of platelets in plasma (less than 150 × 10 * 9 g/l), associated with a violation of their production or rapid decay. The pathology can be congenital, more often acquired due to bone marrow damage, deficiency of vitamins B9 and B12, severe infections, and splenomegaly. | Risk of massive blood loss, internal, uterine bleeding, miscarriage, hemorrhagic stroke. Prohibition on physical activity, restriction of vital activity. | Clinical blood test Hemostasiogram |
| Thrombocytopenic purpura, ITP (Wergolf's disease) | An autoimmune disease that occurs in a chronic form and is more common in young women. With ITP, the amount of IgG on the surface of platelets increases 10 times. The appearance is provoked by viruses, bacteria, and taking certain medications. | Ophthalmic hemorrhages, decreased visual acuity. Skin hemorrhages - petechial rash, purpura. Uterine bleeding, spontaneous abortion, stroke. | Titer for antibodies to platelets General blood test Coagulogram |
| Hemophilia | Inherited with the maternal X chromosome in an autosomal recessive manner. There are 3 forms of the disease, the most common is classical hemophilia A. | Hemorrhages in muscles, internal organs, and joints, and associated disability. | Thromboelastography, APTT Tests for antihemophilic globulin and D-dimer Prothrombin test Coagulogram |
| von Willebrand disease | Associated with a mutation in the hemostasis gene located on chromosome 12. There are 4 forms of pathology - from mild, with asymptomatic carriage, to severe, with gastric, uterine and other types of bleeding. | Genetic risk of bleeding from any organs, premature birth, hemorrhagic stroke - bleeding in the brain with increased blood pressure. | Study of the activity and properties of von Willebrand factor Activity of ADAMTS 13, 8th coagulation factor |
To treat hypocoagulable conditions, corticosteroids and immunosuppressants are used, and the missing antihemophilic globulin (coagulation factor VIII) or platelet concentrate is administered.
Consequences of increased blood clotting
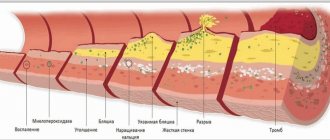
Under these conditions, the risk of blood clots is significantly increased. Inflammation of thrombosed veins leads to thrombophlebitis, accompanied by:
- pain;
- swelling;
- redness of the skin over the vein.
Blood clots in blood vessels lead to narrowing of their lumen and damage to tissue areas due to a lack of blood supply. When blood flow through a vessel is completely stopped due to a blood clot, an area deprived of blood supply appears in the tissue, which is called an ischemic focus. In this area, cells quickly die and the normal functioning of the organ is disrupted. Irreversible damage to the brain and heart are the most dangerous consequences of thrombosis. Another insidious complication is the detachment of a blood clot. Often the diameter of the blood clot is smaller than the diameter of the vessel, so the patient is unaware of its presence for a long time. However, with injuries and concussions of the body, at the beginning of taking medications that thin the blood, as well as when getting up on your feet after a long stay in bed (for example, after surgery), the clot can break off and continue to move through the bloodstream until it clogs the lumen of the vessel somewhere. It is because of such blood clots that a formidable and very dangerous complication develops - pulmonary embolism, which can result in the death of a person if medical assistance is not provided in time. They can only be detected by carrying out certain studies, including a general blood test for blood clotting.
Disorders of vascular-platelet hemostasis
Disturbances in this part of hemostasis most often manifest themselves as increased bleeding, a tendency to form hematomas (bruises) with the slightest contact, or even spontaneously, for no apparent reason. In some situations, on the contrary, there is a tendency to excessively easy thrombosis.
There are factors that stimulate the formation of a primary thrombus and those that disrupt it. Stimulants include the inflammatory process, because inflammation increases the content of biologically active substances in the blood. We can say that there is a readiness for the formation of a blood clot; it is only a matter of local damage to the vessel. Therefore, in severe infectious diseases, blockage of blood vessels may occur. There is an increased readiness for thrombosis during pregnancy, as well as in some hereditary diseases (thrombophilia). Among food products, table vinegar (marinades) and coffee increase platelet activity.
The process of formation of a primary thrombus is disrupted when the number of platelets decreases (thrombocytopenia) and when there is a qualitative deficiency of platelets (thrombocytopathy). Thrombocytopathy can occur when taking certain medications. First of all, these are anti-inflammatory drugs: aspirin, analgin, brufen, some antibiotics. Thrombocytopathy also develops in kidney diseases. Spices and strong alcohol can also reduce the usefulness of platelets.
The blood coagulation system is actually several interconnected reactions occurring in the form of a cascade, or chain reaction. At each stage of this process, the proenzyme (the inactive form of the enzyme) is activated. Thirteen of these proteins (clotting factors) make up the coagulation system. They are usually designated by Roman numerals from I to XIII.
Consequences of decreased blood clotting
With this condition, a person has an increased risk of bleeding. One of the common consequences is gastrointestinal bleeding against the background of an existing ulcer. Blood loss in such conditions due to the duration of bleeding can be very serious. Low blood clotting increases the risk of internal bleeding, which is often noticed too late. Therefore, it is necessary to conduct a general blood test for blood clotting before any operation, as well as during treatment with drugs that have a blood thinning effect (anticoagulants, antiplatelet agents, fibrinolytics, etc.).
Disturbances in the coagulation system
A decrease in the content or activity of coagulation factors may be accompanied by increased bleeding (for example, hemophilia A, hemophilia B, von Willebrand disease). Excessive activation of coagulation hemostasis (for example, Leiden mutation of factor V) leads to the development of thrombosis (thrombophilia).
Hemostasis and pregnancy
Among all the causes of miscarriage, problems in the hemostatic system are in second place in frequency. Second after obstetric and gynecological reasons. What's the matter?
During pregnancy, the expectant mother's body prepares for childbirth. The hemostasis system is also being prepared to minimize blood loss during childbirth. Hemostasis is activated progressively along with increasing gestational age. If a woman’s hemostasis is initially overactive, then during pregnancy microthrombi may form in the vessels of the uterus or placenta, which leads to miscarriage or frozen pregnancy.
Under what conditions can this happen?
- 1. For hereditary thrombophilia,
more often when there is a violation of the metabolism of folic acid and its compounds (folates), when the amount of homocysteine in the blood increases. The reasons for the increase in homocysteine levels may be a lack of folic acid and vitamin B12 in the diet, thyroid disease, and kidney disease. It can also increase in smokers, coffee drinkers and while taking medications such as theophylline (by the way, a relative of caffeine), nicotinic acid. Homocysteine damages the endothelium (inner layer) of blood vessels, and this damage triggers blood clots.
- 2. For antiphospholipid syndrome (APS)
– this is the name of an autoimmune disease in which antibodies are produced to one’s own clotting factors. As a result, blood clots also spontaneously form in the vessels.
Who needs to determine blood clotting?
To reduce the risk of developing vascular accidents and unexpected bleeding, it is necessary to periodically monitor the state of the blood coagulation system using a laboratory method. This is especially important for:
- people over 40 years old;
- women during and after menopause;
- women during pregnancy;
- people who regularly take blood thinners (aspirin);
- patients suffering from varicose veins;
- those preparing for surgery, etc.
The doctor must prescribe blood clotting tests if hemophilia is suspected (usually this disease is detected in early childhood and young adulthood) or when treating an existing thrombosis with fibrinolytic therapy and anticoagulants.
2. Symptoms of the disease
Symptoms of hemophilia may include:
- Bleeding in a joint or muscle area that causes pain and swelling;
- Abnormal bleeding after wounds or surgery;
- Bruising;
- Frequent nosebleeds;
- Blood in the urine;
- Bleeding after dental surgery.
Some people with mild hemophilia may not experience all of these symptoms, especially as the person gets older. However, in infants it is usually possible to diagnose hemophilia based on some signs. So, signs of hemophilia in infancy may be an unusual reaction to the most common vaccination - intramuscular bleeding and serious bruising. Or, for example, bleeding that begins after cutting the umbilical cord and does not stop for a long time (but this happens very rarely).
Visit our Therapy page
How to test your blood clotting
Blood coagulation is a complex process consisting of several different parts and stages. Therefore, a blood clotting test should help evaluate the performance of each component link. Blood clotting occurs through the interaction of many factors along a chain. The results of a general blood test for blood clotting help determine which of the factors is impaired, which facilitates further diagnosis and choice of treatment. For example, an analysis to evaluate APTT (Activated partial thromboplastin time) helps to identify a violation of the “intrinsic” coagulation pathway and determine the tendency to bleeding. And prothrombin time allows you to evaluate the “external” pathway of blood coagulation, detect liver dysfunction and vitamin K deficiency. Another important indicator that greatly helps doctors when planning operations and assessing the risk of thrombosis (including during pregnancy) is a blood test to D-dimer. It allows you to:
- determine the risk level of acute and severe cardiovascular conditions;
- predict the further course of thrombosis;
- monitor the results of treatment over time.
Conducting a general blood clotting test is an important study that helps to significantly reduce the risk of unexpected complications and mortality after illness, surgery, or childbirth. The analysis data gives the doctor the opportunity to expect objective results from the upcoming treatment and control it, and the patient a chance to protect himself from the undesirable consequences of blood clotting disorders.
Reasons for the development of pathology
The mechanism and type of inheritance of hemophilia have been studied in sufficient detail. Genes that provoke insufficient production of blood clotting factors are linked to the X chromosome. The pathology is inherited recessively through the female line. Hereditary pathology occurs exclusively in boys.
The sons of a healthy man and a woman who is a carrier of the pathological gene are equally likely to be born without signs of hemophilia or with them. A man suffering from bleeding disorders will be able to conceive healthy children with a woman who is not a carrier of the altered gene.
Medicine knows of isolated cases of hemophilia in women. Their mothers were carriers of a mutated gene, and their fathers suffered from insufficient production of blood clotting factors. The cause of hemophilia in such cases is a combination of recessive and dominant genes.
What is this condition
Hypercoagulation syndrome is not common among the population. According to official statistics, there are 5-7 cases of the disease per 100,000 people. But knowing what it is and how to avoid the risk of the syndrome is absolutely necessary.
The disease is based on a high level of blood clotting due to changes in its composition.
The usual standard for the liquid to solid ratio is 60 to 40%. Due to a lack of fluid, nutrients or other reasons, the plasma in the blood tissues becomes much smaller, and denser elements predominate.
As a result, the blood becomes very thick, loose and sticky. This qualitatively changes its coagulability.
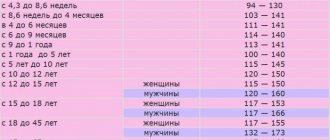
In a normal person, bleeding stops after 2-4 minutes, and a clot remaining on the skin forms after 10-12 minutes. If it occurs earlier, it is suspected that it is prone to hypercoagulability and the necessary tests must be performed to identify the abnormality.
Diagnosis of pathology
Diagnostic procedures are performed by doctors of several specializations: neonatologist, pediatrician, geneticist and hematologist. For concomitant pathologies, consultation with a gastroenterologist, orthopedist, otolaryngologist and neurologist may be required.
At-risk couples should visit a doctor before conceiving a child. Molecular genetic research of biomaterials from future parents will allow us to take into account the risk of having a child with hemophilia. After conception, prenatal screenings may be performed. Their results will confirm or refute the fact that the child inherited hemophilia.
Neonatal tests performed in the first days of a baby’s life are no less effective. A coagulogram provides the neonatologist with comprehensive information about the production of coagulation factors by the newborn’s body.
In case of hemarthrosis, the child is prescribed an X-ray examination of the joints. Ultrasound diagnostics is performed when signs of internal bleeding and retroperitoneal hematomas are detected.
Prevention and treatment
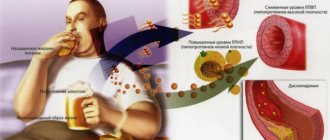
The causes of vascular diseases often lie in late diagnosis and lifestyle provocations. Addiction to smoking, alcohol, junk food and sugar are harmful to your health. Therefore, prevention is important to prevent disease and blood clots.
Prevention
- Diet.
- Quitting smoking and drinking alcohol.
- Avoid intense physical activity.
- Walking through a coniferous forest or just in a green park.
You should exclude sweets, pickles, salty and fried foods, as well as bananas, potatoes and carbonated drinks from your diet. Carbohydrates can be obtained in the form of vegetables, fruits and natural juices.
Tea should be unsweetened, marmalade and sweets are allowed to a minimum.
Protein - in the form of porridges and cereal soups, lean meat and fish. For oils, it is better to use butter and olive oil in small quantities.
Medicines
Don't forget to schedule medical help. There is no need to look for substitutes; you should only take what the doctor prescribed.
During treatment, drugs that dilute platelets are often used: aspirin, heparin, fragmin, clopidogrel, chimes, pentoxifylline, etc. To this are added physiotherapy and injections of vitamins E, C, P (or taking them in tablets).
Folk remedies
Treatment at home is allowed only in combination with a therapeutic regimen. Folk recipes are based on the medicinal effects of plants - grapes, string, licorice, etc.
Also, take 1-2 tablespoons of honey in the morning on an empty stomach, and also use garlic and any raspberry jam.