The heart is the most important human organ that does not stop for a minute. Its contraction is ensured thanks to a complex system of nerve impulses transmitted first from the sinus node in the right atrium, spreading to the atrioventricular node and the entire area of the septum. This process is considered normal and is called sinus rhythm. Sometimes, due to various reasons, patients experience an atrial rhythm on the ECG. In the article we will look at what this means and what the possible reasons for such a violation may be.
Development mechanism
Any cardiac conduction route that does not follow the path described above is called an ectopic rhythm. In this case, an electrical impulse that occurs not in the sinus node, but outside it, excites the heart before the signal is transmitted from the normal pacemaker, that is, the sinus node. In simple words, atrial rhythm is a condition in which the heart muscle contracts faster due to the advance of a healthy impulse by a pathological (minor) one.
Often such a violation occurs due to various blockades due to congenital or acquired causes. In this case, a separate part of the heart cannot be excited due to blocking the propagation of the nerve impulse. When activation occurs, an additional contraction is noted, which disrupts the sequence of heart and atrium impulses. This causes the so-called atrial rhythm.
According to some scientists, the pathological condition can develop as a result of hypoxia or inflammatory myocardial diseases. Cases of ectopic rhythm occurring after influenza, sore throat and other infectious diseases have been reported.
Important! Regardless of the cause of cardiac conduction disturbances, it is necessary to promptly identify the pathological condition and take measures to treat it.
ATRIAL TACHYCARDIA
What types of atrial tachycardia can be distinguished? What are the electrocardiographic signs of atrial tachycardias?
Atrial tachycardias account for approximately 20% of all supraventricular tachycardias. According to the electrophysiological mechanisms of development, three types of atrial tachycardia are distinguished: automatic, triggered (post-depolarization) and reciprocal (re-entry). Reciprocal atrial tachycardias are more often paroxysmal, and automatic ones are chronic (constant or continuously recurrent). In addition, almost all researchers agree that in children, a violation of automaticity can be considered the predominant cause of the development of atrial tachycardia, and the arrhythmia itself is quite often persistent or chronic, lasting months and sometimes years, and can lead to the development of cardiomegaly.
Electrocardiographic diagnosis and clinical manifestations
Electrocardiographically, atrial tachycardias are characterized by the presence of a P wave, the shape of which usually differs from its morphology in sinus rhythm, located before the QRS complex of a supraventricular type (PR interval less than RP interval). The frequency of tachycardia in adults usually ranges from 140 to 180 beats per minute. With an increase in the frequency of the atrial rhythm, the PR interval may increase, and the P wave merges with the preceding T wave. Deterioration of atrioventricular conduction is sometimes accompanied by the development of second-degree AV block (Samoilov-Wenckebach period) without cessation of tachycardia, which distinguishes atrial tachycardia from most atrioventricular reciprocal tachycardia. Although, based on clinical and ECG data, it is difficult to distinguish automatic atrial tachycardia from arrhythmia developing by the re-entry mechanism, there are also a number of differential diagnostic signs. Automatic atrial tachycardia cannot be caused or stopped by pacing, which is precisely typical for reciprocal arrhythmias. Stimulation of the atria at a rate higher than the rate of automatic atrial tachycardia only temporarily suppresses the arrhythmia; after cessation of stimulation, it resumes.
The first P wave of automatic atrial tachycardia is similar to subsequent P waves. In reciprocal tachycardia, the shape of the atrial extrasystole complex, with which the attack usually begins, differs from subsequent P waves, the morphology of which depends on the location of the impulse circulation. In contrast to arrhythmias caused by the re-entry mechanism, the frequency of automatic atrial tachycardias often gradually increases. This phenomenon in electrophysiology is figuratively called “warms up”. In clinical practice, determining the electrophysiological mechanism of the development of atrial tachycardia is necessary, mainly, only when deciding on the use of cardiac pacing.
Vector analysis of the atrial ECG complex during tachycardia helps to establish its localization. A positive or biphasic P wave in lead aVL indicates the presence of an ectopic focus in the right atrium, while a positive P wave (“dome and dart”) in lead V1 and a negative one in leads V4-V6 indicate the origin of the arrhythmia from the left atrium.
Atrial tachycardia in some cases must be differentiated from sinus tachycardia. Differential diagnosis can be difficult, but it is important for choosing treatment tactics. Physical activity and vagal maneuvers significantly affect the frequency characteristics of sinus tachycardia and have little or no effect on them in atrial tachycardia. Long-term ECG recording in patients with chronic atrial tachycardia can reveal short periods of sinus rhythm (especially at night), which also helps in differential diagnosis.
Atrial tachycardias often develop in patients with organic heart disease. They are diagnosed with diseases such as coronary artery disease, myocardial infarction, arterial hypertension, heart valve lesions, dilated cardiomyopathy, cor pulmonale, etc. The role of digitalis intoxication, alcohol intake and hypokalemia in the appearance of atrial tachyarrhythmias is known. At the same time, a number of patients (primarily with automatic atrial tachycardia) are not diagnosed with cardiovascular diseases, which could be the cause of the arrhythmia.
In patients with atrial tachycardia, the prognosis is usually determined by the underlying disease. Mortality among them in the absence of other pathology other than heart rhythm disturbances is very low. However, if the arrhythmia occurs with high frequency and for a long time, then even in patients without organic heart damage, cardiomegaly develops, the ejection fraction decreases and congestive heart failure appears.
Treatment. Patients with asymptomatic, rare, short-lived paroxysms of atrial tachycardia do not require treatment. They need to be examined in order to identify the cause of the rhythm disturbance and eliminate it. Pharmacotherapy or non-drug treatment is necessary only for patients with severe attacks of arrhythmia, as well as in its chronic course, even in the absence of hemodynamic disturbances and good tolerance of the rhythm disturbance - due to the high risk of developing cardiomegaly and heart failure. Many cardiologists, when treating such patients, currently give preference not to antiarrhythmic drugs, but to interventional interventions, given their high effectiveness with a small number of complications.
Paroxysms of atrial tachycardia with unstable hemodynamics should be stopped by an EIT discharge of medium energies (50-100 J). Pharmacotherapy for atrial tachycardias has not been sufficiently developed, although, in principle, it is carried out as for other atrial tachyarrhythmias. When hemodynamics are stable, to reduce high heart rate, drugs that worsen atrioventricular conduction are used: calcium antagonists (verapamil, diltiazem), beta blockers, cardiac glycosides, or a combination thereof. The effectiveness of these drugs in terms of restoring and maintaining sinus rhythm is low. If the paroxysm remains, then restoration of sinus rhythm is carried out with the intravenous administration of antiarrhythmics of classes 1A, 1C and III (procainamide, propafenone, amiodarone, sotalol, etc.), and in case of reciprocal atrial tachycardia, pacing can be used for this purpose.
In order to prevent repeated attacks of arrhythmia, according to our experience and literature data, first of all, drugs of classes 1C and III (propafenone, flecainide, encainide, amiodarone, sotalol) should be used; class 1A antiarrhythmics such as quinidine, disopyramide, procainamide are less effective, ajmaline [1, 2, 3]. K. Koike et al. (13), having assessed for several years the effectiveness of 5 antiarrhythmic drugs of various classes, as well as digoxin and its combinations with propranolol, metoprolol, quinidine for automatic atrial tachycardia in children, they came to the conclusion that it is advisable to begin therapy for this cardiac arrhythmia with sotalol, since in 75% of cases it restored sinus rhythm or significantly reduced the frequency of ventricular contractions. If it is ineffective or there are contraindications, according to the authors, it is necessary to use class 3 antiarrhythmics (with the exception of ethmosin, which is ineffective with ALART) or amiodarone. Chronic atrial tachycardia in most cases is difficult to respond to mono- and combined antiarrhythmic therapy. EIT in this case is also ineffective. If antiarrhythmics do not work, in patients with chronic atrial tachycardia it is necessary to reduce the ventricular rate to prevent the development of congestive heart failure. For this purpose, verapamil, diltiazem, cardiac glycosides or even amiodarone are used (combinations of these are possible); in addition, the issue of non-drug treatment should be addressed.
Radiofrequency catheter destruction has been successfully used to treat atrial tachycardia, regardless of the electrophysiological mechanism of its development (automatic, triggered or reciprocal) and localization (right or left atrium). The main indication for radiofrequency catheter destruction is the ineffectiveness of pharmacotherapy or the patient's reluctance to take antiarrhythmic drugs for a long time. In the USA, according to some data, the effectiveness of such an intervention is 75%, and the number of complications is 0.8% [4]. Destruction of the atrioventricular connection with implantation of a pacemaker or its “modification” (partial destruction) is carried out if radiofrequency catheter destruction of the arrhythmia focus is ineffective or impossible. In patients with symptomatic recurrent supraventricular tachycardias that are controlled by pacing, in whom drug treatment and radiofrequency catheter destruction have been ineffective, implantation of an antitachycardial pacemaker is possible. Surgical interventions (isolation, resection or destruction of the arrhythmogenic zone) are now rarely performed in case of failure of radiofrequency catheter destruction or if another cardiac surgery is planned.
Sinoatrial reciprocal tachycardia
One of the forms of atrial tachycardia, which is somewhat different in its clinical course, electrophysiological and ECG diagnostics, as well as pharmacotherapy, is sinoatrial reentrant tachycardia (sinus nodal reentrant tachycardia). The development of sinoatrial reciprocal tachycardia is associated with the circulation of an excitation wave in the sinus node with the inclusion in some cases of a nearby section of the right atrium myocardium in the circulation circuit.
This arrhythmia, as a rule, is paroxysmal in nature, and the heart rate varies from 100 to 220 beats per minute, but in general it is less than with other supraventricular tachycardias, and in most cases does not exceed 150 beats per minute. Attacks of tachycardia in this case are most often short (from 5-20 complexes to several minutes), prolonged attacks are observed very rarely. It is difficult to talk about the true prevalence of sinoatrial reentrant tachycardia. The frequency of detection of sinoatrial re-entry, according to most researchers, ranges from 2 to 10% among all supraventricular tachycardias. There is much less data indicating its wider distribution. Thus, SART was diagnosed in 11 of 65 patients (16.9%) with supraventricular tachycardias who underwent intracardiac electrophysiological study [5].
Since the mechanism of development of sinoatrial reciprocal tachycardia is associated with the re-entry of the excitation wave, it is successfully caused and stopped by extrastimulation of the atria (sometimes even the ventricles) and increased stimulation of the atria. Unlike most atrial tachycardias, the P wave located before the QRS complex is identical or very similar to that recorded during sinus rhythm. The PR interval is shorter than the RP interval. The sudden onset and, in most cases, the sudden cessation of an attack, as well as the possibility of stopping it with vagal techniques (sinus tachycardia and PRT do not stop with them) can serve as important differential diagnostic signs of sinoatrial reciprocal tachycardia.
Since the frequency of attacks with sinoatrial reentrant tachycardia is usually small, and the attacks themselves are short-lived, it may be asymptomatic and do not require treatment. Curative and prophylactic antiarrhythmic therapy for symptomatic sinoatrial reciprocal tachycardia is similar to that carried out for atrioventricular junctional reciprocal tachycardia. Relief begins with vagal maneuvers (Valsalva maneuver, carotid sinus massage), and if there is resistance to them, antiarrhythmics are administered intravenously: ATP 10-20 mg (adenosine 6-12 mg, very quickly) or calcium antagonists (verapamil 5-10 mg or diltiazem 0.25-0.35 mg/kg for 2 minutes). Possible IV use of digoxin, beta blockers and amiodarone. If the patient's condition is unstable (severe anginal pain, significant decrease in blood pressure, cardiac asthma or pulmonary edema), emergency electrical cardioversion is performed (first shock with a power of 50-100 J). Paroxysms of tachycardia can be successfully stopped by cardiac pacing. To prevent attacks of sinoatrial reciprocal tachycardia, verapamil, diltiazem, beta-blockers, digoxin, as well as class III antiarrhythmic drugs - amiodarone and sotalol are primarily used. There are reports of the effective use of radiofrequency catheter destruction of the source of arrhythmia.
Multifocal (chaotic) atrial tachycardia
Multifocal atrial tachycardia is diagnosed in 0.13-0.4% of hospitalized adult patients. It most often affects older people (the average age is more than 70 years). This rhythm disturbance is recorded in approximately equal proportions in men and women. More than 60% of patients with multifocal atrial tachycardia are diagnosed with pulmonary disease. Chronic obstructive pulmonary diseases are the most common. Less commonly, arrhythmia acts as a complication of acute pneumonia, pulmonary embolism, and lung tumors. Medicines such as aminophylline and isoproterenol, used in the treatment of chronic obstructive pulmonary diseases, can play a role in the occurrence of arrhythmia, and also cause its more severe course. In addition to pulmonary pathology, such patients often have cardiovascular diseases (coronary artery disease, hypertension, less commonly valvular heart disease, etc.), accompanied by congestive heart failure. It is important to note that in many cases (according to some data, up to 70%), disorders of carbohydrate metabolism accompany multifocal atrial tachycardia. Mortality among adult patients with multifocal atrial tachycardia is high and ranges from 29-62%. The cause of death is usually severe illness, which affects most patients with multifocal atrial tachycardia, and not the rhythm disorder itself.
Electrocardiographic criteria for diagnosing multifocal atrial tachycardia are:
- the presence of three or more P waves of different morphology in one ECG lead;
- the presence of an isoline between the P waves;
- irregular PR, PP and RR intervals.
The shape of the P waves depends on the location of the ectopic focus of the arrhythmia and changes in intraatrial conduction.
Most often, multifocal atrial tachycardia must be differentiated from atrial fibrillation. In contrast to the latter, with multifocal atrial tachycardia, P waves of changing shape and the isoline between them are clearly visible.
In the management of patients with multifocal atrial tachycardia, an important place is occupied by the treatment of the underlying disease and the correction of factors predisposing to its development: combating infection during exacerbation of chronic pulmonary disease, treatment of heart failure, normalization of acid-base balance and electrolyte disturbances, streamlining the use of beta-adrenergic receptor agonists and methylxanthine derivatives. These measures sometimes make it possible to normalize the rhythm even without the use of antiarrhythmic drugs.
Antiarrhythmic therapy of multifocal atrial tachycardia is associated with great difficulties. Some studies have shown the ineffectiveness of quinidine, procainamide, lidocaine and phenytoin. Cardiac glycosides are also ineffective and often cause intoxication due to the presence of hypoxia and a number of severe metabolic disorders in patients. Electropulse therapy does not restore sinus rhythm and is therefore ineffective.
An analysis of works on antiarrhythmic treatment of multifocal atrial tachycardia shows that the most effective in slowing down, converting the rhythm and preventing relapses of arrhythmia are probably verapamil, beta-blockers (however, they are contraindicated in patients with bronchospastic syndrome) and amiodarone [6, 7, 11]. There is a small number of studies examining the effect of class 1C artriarrhythmics on multifocal atrial tachycardia. Thus, in particular, we describe a case of tachycardia relief due to intravenous administration of flecainide to a 57-year-old patient in whom verapamil, metaprolol, sotalol, disopyramide and some other antiarrhythmic drugs were ineffective [8]; the possibility of successful parenteral and oral use of propafenone for this type of arrhythmia in pediatric practice has been shown [9]. Interesting data were obtained regarding the high stopping effectiveness of magnesium sulfate (in some cases in combination with potassium preparations): in 7 out of 8 patients with multifocal atrial tachycardia (87.7%), sinus rhythm was restored when administered intravenously for 5 hours from 7 to 12 g MgSO4. It should be noted that a decrease in the level of magnesium and potassium in the blood plasma was observed only in 3 patients [10].
Thus, it is advisable to start pharmacotherapy of multifocal atrial tachycardia with beta-blockers (if there are no contraindications to them) or verapamil; if they are ineffective, use amiodarone and class 1C antiarrhythmics, and to relieve arrhythmia, intravenous administration of magnesium sulfate is also possible.
Literature
1. Pongiglione G., Strasburger JF, Deal BJ et al. Use of amiodarone for short-term and adjuvant therapy in young patients // Am. J. Cardiol. 1991; 68: 603-608. 2. Zeigler V., Gillette PC, Ross AB et al. Flecainide for supraventricular and ventricular arrhythmias in children and young adults // Am. J. Cardiol. 1988; 62:818-820. 3. Colloridi V., Perri C., Ventriglia F., Critelli G. Oral sotalol in pediatric atrial ectopic tachycardia // Am. Heart J 1992; 123: 254-256. 4. Scheinman MM Patterns of catheter ablation practice in the United States // Pacing Clin. Electrophysiol. 1994; 17: 873-877. 5. Gomes JA, Hariman RJ, Kang PS et al. Sustained symptomatic sinus node reentrant tachycardia: incidence, clinical significance, electrophysiologic observations and the effects of antiarhythmic agents // J. Am. Coll. Cardiol. 1985; 5: 45-57. 6. Scher DL, Arsura EL Multifocal atrial tachycardia: mechanisms, clinical correlates and treatment // Am. Heart J 1989; 118: 574-580. 7. Arsura E., Lefkin AS, Scher DL et al. A randomized, double-blind, placebo-controlled study of verapamil and metoprolol in treatment of multifocal atrial tachycardia // Am. J. Medicine. 1988; 85:519-524. 8. Creamer JE, Nathan AW, Camm AJ Successful treatment of atrial tachycardias with flecainide acetate // Br. Heart J 1985; 53: 164-166. 9. Reimer A., Paul T., Kallfelz H.-C. Efficacy and safety of intravenous and oral propafenone in pediatric cardiac dysrhythmia // Am. J. Cardiol. 1991; 68:741-744. 10. Iseri LT, Fairshter RD, Hardemann JL, Brodsky MA Magnesium and potassium theraphy in multifocal atrial tachycardia // Am. Heart J 1985; 110: 789-794. 11. Olgin JE, Zipes DP Specific arrhythmias: diagnosis and treatment. In Braunwald E. (eds). Heart disease. A textbook of cardiovascular medicine. Philadelphia: WB Saunders company. 2001. P. 837.
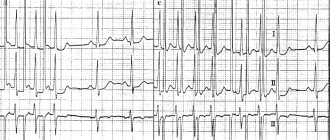
How does it show up on an ECG?
Pathological conduction of the heart can be determined using an electrocardiogram. This instrumental diagnostic technique allows you to identify the localization of rhythm disturbances and the cause of the deviation. Using an ECG, a specialist can determine one of the types of ectopia:
- left atrial rhythm - in this case, deviations such as a P wave of two parts are noted, when the first of them has a dome-shaped appearance, and the second looks like a high and narrow peak. In addition, PI can be smoothed, and PV 1 and 2 are positive, PV 5 and 6 are negative;
- right atrial - in the area of the third lead a negative P wave is observed, while in the first and second leads it is positive. This is characteristic of a mid-lateral right atrial rhythm. The lower type of this disorder is characterized by a negative P wave in the second and third leads, as well as a smoothed one, and aVF in the chest leads - 5 and 6;
- lower atrial rhythm - on the electrocardiogram it looks like a shortening of the PQ interval, a negative P wave in the first, third and aVF leads.
Electrocardiography allows for accurate diagnosis
Based on this, we can say that a specialist determines the conductivity of the heart by assessing the P wave, which, with an ectopic rhythm, is characterized by pathological amplitude and polarity. An experienced doctor should diagnose the condition, since it can be quite difficult to determine the pathology on an ECG due to the vagueness of the signs. Holter monitoring is often used to make an accurate diagnosis.
Do cardiac arrhythmias manifest themselves in the same way?
All rhythm and conduction disorders clinically manifest themselves differently in different patients. Some patients do not feel any symptoms and learn about the pathology only after a scheduled ECG. This proportion of patients is insignificant, since in most cases patients note obvious symptoms.
Thus, rhythm disturbances accompanied by rapid heartbeat (from 100 to 200 beats per minute), especially paroxysmal forms, are characterized by a sharp sudden onset and interruptions in the heart, lack of air, pain in the sternum.
Some conduction disorders, such as fascicular blocks, do not show any signs and are recognized only on an ECG. Sinoatrial and atrioventricular blockades of the first degree occur with a slight decrease in heart rate (50-55 per minute), which is why clinically they can manifest only slight weakness and increased fatigue.
Blockades of the 2nd and 3rd degrees are manifested by severe bradycardia (less than 30-40 per minute) and are characterized by short-term attacks of loss of consciousness.
In addition, any of the listed conditions may be accompanied by a general severe condition with cold sweat, intense pain in the left half of the chest, decreased blood pressure, general weakness and loss of consciousness. These symptoms are caused by impaired cardiac hemodynamics and require close attention from a doctor.
How to make a diagnosis?
What diseases can cause rhythm disturbances?
Atrial rhythm on the ECG can appear in patients regardless of age, gender and region of residence. Often the pathology is temporary and due to certain physiological reasons. In such cases, the duration of conduction disturbance lasts no more than several hours or days.
The situation is different with the development of certain diseases that can provoke an ectopic rhythm. These include myocardial inflammatory processes, ischemic disorders, and sclerotic changes. Let's look at the most common of them.
Myocarditis
Myocarditis is an inflammatory process of the myocardium. The causes of the pathology are damage to the heart muscle by viruses, bacteria or toxins. Often the disease develops due to an allergic reaction or an autoimmune disorder. Doctors note that myocarditis can act as an independent pathology or be provoked by other diseases. The course of inflammation can be chronic or acute. The latter form often develops into cardiomyopathy.
Myocarditis is a common cause of disruption of normal rhythm
Common symptoms of myocarditis are atrial rhythm, chronic fatigue, dizziness, rapid heartbeat, chest pain, and more. If the pathology is diagnosed in a timely manner and the necessary treatment is carried out, the prognosis for the patient is quite favorable.
Cardiomyopathy
A group of diseases that combine pathological changes in myocardial tissue are called cardiomyopathies. As a result of these disorders, disruptions in the functioning of the heart occur. The disease develops both under the influence of cardiac and non-cardiac factors. That is, there are a lot of reasons that can provoke cardiomyopathy. The disorder is primary or secondary in nature and is almost always accompanied by an extracardiac rhythm.
Rheumatism
Rheumatism is a disease accompanied by an inflammatory process of connective tissues and heart muscle. It mainly affects children under 15 years of age. The main cause of inflammation is an attack of the body by streptococcal infection, which provokes diseases such as tonsillitis, tonsillitis, pharyngitis, etc. Rheumatism occurs as a complication, leading to impaired contractility of the heart, increased temperature, joint and heart pain and the development of other symptoms in the patient.
Heart defects
Heart defects are congenital or acquired. The concept of “defect” implies a deviation in the structure or structure of an organ, as a result of which electrical conductivity or blood flow in it is disrupted. In addition to the congenital or acquired type, doctors classify the disease into combined or isolated, as well as the presence of a symptom such as cyanosis (bluish tint of the skin) or its absence.
Sick sinus syndrome
A dangerous condition that carries the risk of sudden cardiac arrest. The causes of this disorder are congenital or acquired. These include coronary heart disease, cardiomyopathy, trauma to the heart muscle, cancer in this area, defects, toxic damage to the organ and much more.
Sick sinus syndrome provokes a disturbance in the electrical conductivity of the heart
A person suffers from arrhythmia, decreased heart rate, weakness, headaches, paresis, decreased vision, hearing, and memory. Without the necessary treatment, the pathology is often accompanied by death.
Cardiac ischemia
IHD is a very common disease, which is accompanied by many disturbances in the functioning of a vital organ. Pathology is provoked by many factors, the most common of which are smoking, anatomical aging of the body, genetic predisposition, diabetes mellitus, hypertension, etc. The atrial rhythm is shown on the cardiogram of many people with this deviation. In addition, signs such as shortness of breath, headache, chest discomfort, and chronic fatigue are noted.
Vegetovascular dystonia
VSD is a set of functional disorders that are caused by a violation of the regulation of vascular tone of the autonomic nervous system. In this case, an ectopic rhythm is formed, the patient experiences periodic or constant disturbances in heart rate, excessive sweating, frequent headaches, coldness in the extremities, lightheadedness or fainting.
Important! Vegetative-vascular dystonia often provokes a persistent increase in blood pressure and nervousness, significantly reducing the patient’s quality of life.
Types of arrhythmias
Most people by arrhythmia mean erratic contractions of the heart muscle (“the heart beats as it wants”). However, this is not quite true. The doctor uses this term for any disturbance of cardiac activity (decreased or increased heart rate), so the types of arrhythmias can be presented as follows:
- Sinus arrhythmia, which may be associated with cycles of respiratory activity (increased rhythm during inhalation and slower rate during exhalation) or occur independently of breathing, but indicate some kind of cardiovascular pathology (coronary artery disease in old age) or be a consequence of autonomic dysfunction, for example, in teenagers. This type of arrhythmia is harmless and does not require special treatment measures. The ECG shows a difference between cardiac cycles (> 0.05 s).
- Sinus tachycardia is diagnosed if the heart rate exceeds 90 beats/min, of course, for no apparent reason (running, exercise, excitement). Typically, with such tachycardia, the heart rate does not exceed 160 beats per minute under calm conditions, and only during intense exercise can it reach up to 200 beats. It is caused by many factors associated with pathological processes in the body, therefore the treatment of such tachycardia is aimed at the underlying disease.
- Sinus bradycardia is characterized by a regular but slow sinus rhythm (less than 60 beats/min), associated with a decrease in the automaticity of the sinus node and resulting from excessive physical exertion (in professional athletes), pathological changes (not necessarily cardiovascular, for example, peptic ulcer). ), taking certain medications (digitalis, antiarrhythmic and antihypertensive drugs). Therapy is also aimed at eliminating the cause that caused bradycardia, that is, the underlying disease.
- Extrasystoles that occur with premature excitation and contraction of one part of the heart or all of them at once, therefore, depending on where and in what place the impulse was formed that disrupted the normal sequence of heart contractions, extrasystoles are divided into atrial, ventricular and those coming from the atrioventricular node. Extrasystolic arrhythmia is dangerous if it is group, early and frequent, since it poses a threat to hemodynamics, and as a result can “develop” into ventricular tachycardia or ventricular fibrillation, which will have serious consequences. During myocardial infarction, extrasystolic arrhythmia is recorded in 100% of cases.
- Paroxysmal supraventricular (supraventricular) tachycardia, which develops suddenly and also suddenly stops, is characterized by a regular, strict rhythm, although the contraction frequency can reach 250 beats/min. Such tachycardias include: atrial tachycardia, AV nodal tachycardia and tachycardia with WPW syndrome.
- Arrhythmias associated with conduction disturbances (blockades) are usually well recorded on the ECG, are a companion and symptom of various pathologies and are treated by influencing the underlying disease. Blockades that quite often produce (sinoauricular and atrioventricular) bradycardia (40 beats per minute and below) are considered life-threatening and require the installation of a pacemaker that compensates for cardiac activity.
- Atrial fibrillation, in terms of frequency of occurrence, follows immediately after extrasystole and holds 2nd place in prevalence. It is characterized by the formation of excitation and contraction only in certain areas (fibers) of the atrium, when these processes are absent as a whole. Such chaotic and disorderly excitation of individual fibers prevents the passage of impulses into the atrioventricular node, as well as into the ventricles, to which single impulses nevertheless reach, causing excitation there that responds with random contractions.
Based on heart rate, there are 3 forms of atrial fibrillation:
- Heart rate less than 60 beats/min – bradysystolic;
- 60-100 beats/min – normosystolic;
- Heart rate exceeds 100 beats/min – tachysystolic.
On an ECG with AF, the P wave is not recorded because there is no excitation of the atria, and only atrial f waves are detected (frequency 350-700 per minute), which are characterized by irregularity, differences in shape and amplitude, which gives the electrocardiogram a unique appearance.
The cause of MA may be:
- Organic damage to the heart muscle;
- Age-related changes (coronary heart disease, often in combination with arterial hypertension);
- In young people: rheumatism, valve defects (mitral valve stenosis, aortic valve disease);
- Thyroid dysfunction;
- Congenital pathology (heart defects);
- Acute and chronic heart failure;
- Myocardial infarction;
- Acute cor pulmonale;
- Myocarditis, pericarditis;
- Cardiomyopathy.
The incidence of atrial flutter (AF) is 20-30 times lower than AF. It is also characterized by contractions of individual fibers, but a lower frequency of atrial waves (280-300 per minute). On the ECG, atrial waves have a greater amplitude than in AF.
It is interesting that on one ECG you can see the transition of flicker to flutter and vice versa.
The causes of atrial flutter are similar to the causes of fibrillation.
Symptoms of flickering and fluttering are often absent altogether, but sometimes there are some clinical manifestations caused by erratic activity of the heart or symptoms of the underlying disease. In general, such a pathology does not give a clear clinical picture.
Other reasons
In addition to various diseases that lead to the development of ectopic heart rhythm, other causes can be identified. These include:
- persistent increase in blood pressure;
- smoking and drinking alcoholic beverages;
- carbon monoxide intoxication;
- taking certain medications;
- frequent stress;
- hormonal disorders;
- regular physical activity;
- professional sports.
Arrhythmia often occurs during heavy physical exertion.
These and other changes in the body can lead to intra-atrial conduction, which causes the development of many unpleasant symptoms.
Possible symptoms
Ectopic left and right atrial rhythms manifest themselves in the same way. A person often does not notice changes, and the symptoms of the underlying disease that caused the deviation come first. The only way to detect a violation is to take an electrocardiogram.
In other cases, the patient makes the following complaints:
- feeling of pulse unevenness and interruptions;
- heart sinking;
- dyspnea;
- weakness, decreased ability to work;
- pain or discomfort in the heart area.
In the presence of temporary jumping atrial complexes, symptoms usually either do not appear or are transient. According to my observations, they do not pose any particular danger and do not affect hemodynamics.
With prolonged attacks, the patient’s condition worsens, in addition to the main complaints, signs of circulatory disorders and cardialgia of ischemic origin appear.
Sometimes ectopic rhythm occurs due to dysfunction of the autonomic system:
- If the influence of the sympathetic department predominates, a person’s pulse quickens, the skin becomes cool and pale, and hypertension is observed. This condition is characterized by chills, headache, and often a panic attack.
- When vagotonia (parasympathetic) comes first, the frequency of contractions decreases, sweat is released, blood pressure decreases, and digestion is disrupted.
Features of the patient's symptoms
Often, cardiac conduction disturbances occur without visible symptoms, but more often the following clinical picture is observed:
- attacks of heartbeat sensations. The patient seems to feel tremors in the chest;
- the average number of heartbeats increases;
- depending on the pathology that provoked the extracardiac rhythm, a slowdown in organ contractions may be diagnosed;
- sometimes the heart freezes for a few seconds. In this case, the patient may feel panic, fear, and a feeling of excitement;
- sweat production often increases;
- headaches and dizziness occur;
- due to shortness of breath, breathing is impaired;
- discomfort and pain, burning or tingling sensation are observed in the chest area;
- the skin of the face acquires a bluish tint, cyanosis may spread to the fingertips.
In addition, patients complain of the appearance of a veil before the eyes, difficulty breathing, and bouts of fever. In severe situations, nausea occurs, often accompanied by vomiting and abdominal pain. There is a malfunction in the functioning of the digestive system, which entails belching, heartburn, hiccups, flatulence, and bowel dysfunction. A common sign of the disease is pre-syncope or fainting.
Tachycardia is a common symptom of atrial rhythm
People with this pathology are characterized by an increase in heart rate. Signs of atrial tachycardia include palpitations, shortness of breath, panic, increased sweating, and flushing of the face. Attacks occur mainly at night. Their duration is usually short, lasting from several minutes to several hours. At the same time, the patient experiences panic and fear for his life.
Causes and types
The main causes of atrial, as well as any ectopic (displaced) rhythm, are:
- Changes in the structure of the myocardium - as a result of inflammation, ischemia, cardiosclerosis, hypertrophy or dystrophy.
- Valve defects and other congenital anomalies.
- Violation of electrolyte and water levels. This happens with a sudden loss of fluid (vomiting, diarrhea, taking diuretics).
- Metabolic changes in diseases of the endocrine organs.
- Internal or external intoxication (impaired kidney and liver function, smoking, alcoholism, drug addiction, ingestion of heavy metal salts, etc.).
- Overdose of cardiac glycosides.
- Traumatic chest injury.
All these reasons are characteristic of ectopic atrial impulses in an adult. In children and adolescents, they most often occur against the background of impaired autonomic innervation.
Depending on the frequency of contractions, slow and accelerated atrial rhythms are distinguished. The lower the pacemaker is located in the conduction system, the rarer the pulse - up to 45–60 beats per minute. An increase of up to 130 or more occurs when, under the influence of inflammation or other pathology, hyperexcitation and excessive activity of the ectopic focus develop.
The displaced rhythm may be permanent or temporary. According to localization, it can be left or right atrial, but this division has no particular clinical significance and does not affect the prescribed treatment regimen.
Ectopic impulses can vary in frequency, regularity and strength. But in the absence of normal sinus rhythm, they allow the heart to continue pumping.
Atrial rhythm in children
The regulation of the autonomic nervous system and the cardiac conduction system in newborns differs from that in adults. They do not function fully due to insufficient formation. This provokes the development of atrial rhythm in infants and preschool children. Normally, such a rhythm is independently transformed into a sinus rhythm; the condition does not require additional treatment methods.
Cardiac conduction disorders in children often develop with minor abnormalities of the organ. For example, with mitral valve prolapse or accessory chord. But this does not mean that you should not pay attention to this symptom, because often a deviation can indicate serious heart defects, infectious myocardial lesions, hypoxia, intoxication and other conditions.
The risk group includes children who have suffered an intrauterine infection or prolonged intoxication with alcohol or nicotine, as well as during severe pregnancy and childbirth. Such patients should undergo a thorough examination after birth to ensure timely detection of various diseases and prevent the development of severe complications.
Organic arrhythmias
Organic arrhythmias include:
- Arrhythmias arising from coronary heart disease (myocardial infarction, angina). Arrhythmia is caused by damage to the heart muscle. It makes it difficult for electrical impulses to propagate correctly through the conduction system of the heart. Sometimes damage can even affect the cells of the main pacemaker - the sinus node. In place of the dead cells, a scar of connective tissue (cardiosclerosis) is formed, which is not able to perform the functions of a healthy myocardium. This, in turn, leads to the formation of arrhythmogenic foci and the appearance of rhythm and conduction disturbances.
- Rhythm disturbances that occur after an inflammatory process in the heart muscle - myocarditis. As a consequence, after suffering from inflammation, the myocardium is also replaced by connective tissue (cardiosclerosis).
- Arrhythmias observed in cardiomyopathies. For an unknown reason, myocardial cells are damaged, the pumping function of the heart is disrupted, and heart failure develops. In addition, various rhythm disturbances are very often associated.
- Arrhythmias that appear with various heart defects (congenital and acquired during life). It should be noted that there are congenital primary diseases of the conduction system of the heart itself.
Types of ectopic disorders
Ectopic arrhythmias include various disorders that develop in the area of the ventricles and atria. According to research, it turned out that often the right atrial rhythm, which does not manifest itself on the electrocardiogram, does not come from the sinus node. That is, an electrical impulse is provoked in neighboring areas of the organ.
The most dangerous type of disorder is considered to be atrial fibrillation.
Types of atrial rhythm:
- extrasystole - occurs quite often (about 60% of people), this condition consists of untimely contraction of the heart muscle or its individual parts;
- paroxysmal tachycardia is a separate type of atrial rhythm, accompanied by periodic attacks of accelerated heartbeat. In this case, the number of strokes can reach 220 per minute. Paroxysms replace the normal heart rhythm and have a sudden onset and end. Electrical impulses are generated in the atria, atrioventricular node or ventricles. The duration of the attack varies;
- ectopic accelerated rhythms - attacks of accelerated heartbeat, in which the heart rate increases to 130 beats. In this case, electrical impulses are generated in the atria, ventricles or atrioventricular junction. During an ECG, a non-sinus pacemaker is recorded in the P–QRS–T complex;
- atrial fibrillation or atrial fibrillation - frequent excitation of the atria or individual muscle fibers of a chaotic nature. In some cases, heart rate reaches 600 beats per minute. The prolonged course of such an attack significantly increases the risk of blood clots and the development of ischemic stroke. If left untreated, acute heart failure occurs.
Important! Therapy for any type of ectopic rhythm should be carried out immediately, regardless of the severity and symptoms of the patient.
Classification
All rhythm and conduction disorders are classified as follows:
- Heart rhythm disturbances.
- Conduction disorders in the heart.
In the first case, as a rule, there is an acceleration of the heart rate and/or irregular contraction of the heart muscle. In the second, the presence of blockades of varying degrees with or without slowing of the rhythm is noted.
In general, the first group includes disorders of the formation and conduction of impulses:
- In the sinus node, manifested by sinus tachycardia, sinus bradycardia and sinus arrhythmia - tachyarrhythmia or bradyarrhythmia.
- According to the tissue of the atria, manifested by atrial extrasystole and paroxysmal atrial tachycardia.
- At the atrioventricular junction (AV node), manifested by atrioventricular extrasystole and paroxysmal tachycardia.
- Along the fibers of the ventricles of the heart, manifested by ventricular extrasystole and paroxysmal ventricular tachycardia.
- In the sinus node and along the tissue of the atria or ventricles, manifested by flutter and fibrillation (fibrillation) of the atria and ventricles.
The second group of conduction disorders includes blockades in the path of impulses, manifested by sinoatrial block, intraatrial block, atrioventricular block of 1, 2 and 3 degrees and bundle branch block.
Treatment methods
The atrial rhythm may be hidden and not manifest itself in any way. If the patient does not feel any unpleasant symptoms and the abnormal pacemakers were identified by chance, most often no special treatment is required. For such people, it is enough to undergo a thorough medical examination to exclude serious anomalies in the structure of the heart and other organs. If no deviations are detected, the ectopic rhythm is considered safe for health.
Treatment methods are determined depending on the diagnosis and symptoms of the patient
When a patient has complaints from the cardiovascular system and any pathologies are detected, drug therapy is carried out. The group of drugs includes the following:
- beta blockers and other drugs intended to lower blood pressure (Nadolol, Metoprolol, Carvedilol);
- medications that accelerate the rhythm during bradycardia. These include Atropine, Isoprenaline, Eufillin. Plant-based extracts are often recommended - ginseng, eleutherococcus;
- sedatives are prescribed to patients with the development of vegetative-vascular dystonia. Popular remedies include tincture of motherwort, valerian, as well as Novopassit, Fitosed, Dormiplant;
- Preventive medications are used to prevent strokes, heart attacks and other dangerous complications. For this, Panangin and Cardiomagnyl are prescribed.
Treatment tactics always depend on the disease that acts as a factor provoking arrhythmia. Based on the data obtained during instrumental diagnostics and the patient’s medical history, the doctor selects the necessary medications.
In particularly severe situations, when conservative therapy has proven useless, the patient is given an artificial pacemaker (cardioversion). Often this method is effective for atrial fibrillation and other dangerous conditions.
Causes of cardiac arrhythmia
The causes of arrhythmia (the occurrence of heart rhythm disturbances) are so diverse that listing absolutely everything is a very difficult task. However, in many cases, the safety of the arrhythmia for the patient’s life and further treatment tactics depend on the cause of the arrhythmia.
Many different classifications of the causes of arrhythmia have been proposed, but none of them is currently generally accepted. We consider the following classification to be the most acceptable for the patient. It is based on the presence or absence of primary heart disease in the patient. If there is heart disease, the arrhythmia is called organic, and if there is no heart disease, it is called inorganic. Inorganic arrhythmias are also commonly called functional.
Folk recipes
A healthy lifestyle and proper nutrition help patients prevent many dangerous complications. They are especially indicated for patients with developed atrial rhythm. Giving up bad habits and saturating your diet with plenty of vitamins and minerals is an important step towards health. Some folk recipes have proven themselves well in the fight against heart disorders. Here are some of them:
- mix 200 ml of grapefruit juice with three teaspoons of olive oil. Take half a glass of the drink in the morning and evening for one month;
- Combine chopped figs and walnuts in equal parts, season the resulting mass with honey and refrigerate for a day. Take a teaspoon of the mixture twice a day. The course of treatment is at least 60 days;
- To restore rhythm, a decoction of calendula flowers is often used. To do this, brew a spoonful of herbs with a glass of boiling water and let the medicine brew for at least 2 hours. Take a quarter glass twice a day for a month;
- A decoction of hawthorn and lemon balm has a beneficial effect on heart health. To prepare it, combine a tablespoon of raw materials, pour a liter of boiling water over the mixture, and simmer over low heat for 10 minutes. After this, the medicine should infuse for 40 minutes. Take the drink instead of tea several times a day.
Traditional recipes are a great way to maintain your heart
Important! Any folk remedies should be used only after consultation with a specialist. Self-medication can be extremely dangerous to health.
What does an ECG look like normally and with pathology?
Electrocardiogram parameters in adult men and women are presented in the table and look like this:
| ECG parameters | Norm | Deviation | Probable cause of deviation |
| RRR distance | Even spacing between teeth | Uneven distance |
|
| Heart rate | 60-90 beats/min at rest | Below 60 or above 90 beats/min at rest |
|
| Atrial contraction - R wave | Directed upward, outwardly resembles an arc. The height is about 2 mm. May not be present in ΙΙΙ, AVL, V1. |
|
|
| PQ interval | A straight line between the PQ teeth with an interval of 0.1-0.2 seconds. |
|
|
| QRS complex | Length 0.1 second - 5 mm, then T wave and straight line. |
|
|
| Q wave | Absent or directed downward with a depth equal to 1/4 of the R wave | Depth and/or width exceeding normal |
|
| R wave | Height 10-15 mm, pointing upward. Present in all leads. |
|
|
| S wave | Depth 2-5 mm, sharp end pointing down. |
| Left ventricular hypertrophy. |
| ST segment | Coincides with the distance between the ST teeth. | Any deviation of the horizontal line greater than 2 mm. |
|
| T wave | The height of the arc is up to 1/2 of the R wave or coincides (in the V1 segment). Direction - up. |
|
|
What kind of cardiogram should a healthy person have?
Indications of a good cardiogram for an adult:
- ECG changes in coronary artery disease (introductory review)
| Prong | Lead | Description |
| R |
| Positive. |
| R | AVR | Negative. |
| T | AVR | Negative. |
| R | V1-V4 | Increase in amplitude. |
| R | V5-V6 | Reducing the swing of oscillations. |
| S | V1-V6 | Reduction until complete disappearance. |
| RST segment | On the isoline. | Error no more than 0.5 mm |
The video compares the cardiogram of a healthy and sick person and provides the correct interpretation of the data obtained. Taken from the channel “Life of a Hypertensive”.
Indicators in adults
An example of a normal ECG in adults:
| ECG indicators | Norm |
| QRS | 0.06-0.1 sec |
| P | 0.07-0.11 sec |
| Q | 0.03 sec |
| T | 0.12-0.28 sec |
| PQ | 0.12-0.20 sec |
| Heart rate | 60-80 beats/min |
Indicators in children
Electrocardiogram parameters in children:
| ECG indicators | Norm |
| QRS | 0.06-0.1 sec |
| P | No more than 0.1 sec |
| Q | 0.2 sec |
| QT | No more than 0.4 sec |
| Heart rate |
|
Diagnostics
To identify the problem, ultrasound diagnostics and an electrocardiogram are performed. Since the problem can only make itself felt at a certain time of the day, a Holter ECG study is performed to obtain a more accurate clinical picture. Sensors are attached to the patient’s body; any changes are recorded around the clock.
One of the research methods
Symptoms on the electrocardiogram
ECG is the most accessible and safe research method. On a cardiogram, the doctor evaluates the following indicators:
- Q wave . The indicator is responsible for the initial stage of excitation in the ventricles.
- Condition of the P wave . In this case, electrical impulses are reflected in the atria.
- QRS complex . In medicine it is called ventricular, it reflects the stages of excitation in all departments.
After receiving the necessary information, the doctor will be able to explain the characteristics of the heart rhythm.
The presence of ectopic atrial rhythm may be indicated by the following changes in the ECG:
- intervals and waves with long duration;
- the P wave is negative, with no changes in the ventricular complexes.
Indicators may vary depending on the individual case.