Sepsis is the most severe, generalized form of the infectious process, which develops either with a high pathogenicity of the pathogen or with an insufficient response of the body's defense systems. International consensus recommends using the following definition: sepsis is a life-threatening dysfunction of internal organs caused by dysregulation of the body's response to infection. With sepsis, general intoxication syndrome, thrombohemorrhagic syndrome (hemorrhages) and damage to internal organs are observed.
- Causes of sepsis
- Types of sepsis
- The first signs and symptoms of sepsis
- Diagnosis of sepsis
- Stages of sepsis development
- Clinical classification of sepsis by stages
- Treatment of sepsis
- Complications of sepsis
- Prognosis for sepsis
Causes of sepsis
Sepsis can be caused by most microorganisms known in epidemiology, including bacteria, viruses (including seasonal influenza viruses), fungi, and parasites. Typically, the infectious agent enters the body from the external environment. Under certain conditions, for example, with immunodeficiencies, the disease can develop from the natural, opportunistic flora of the body, which is normally present in every person. [1]
The presence of infection in itself does not guarantee the development of sepsis. Additional conditions are needed that will lead to generalization of the process and a pathological response of the body. The likelihood of such events increases in the following cases:
- The patient's age is over 75 years.
- Performing surgeries or invasive procedures.
- Presence of injuries and burns.
- Immune system disorders - AIDS, cancer, chemotherapy, the need to use immunosuppressive therapy (for example, after organ transplantation), the need to take high doses of glucocorticosteroids.
- Long-term treatment in a hospital setting.
- Availability of catheters, cannulas, probes and other invasive devices.
- Pregnancy and childbirth.
- Chemical dependence - alcoholism, drug addiction.
- The presence of chronic diseases - chronic renal failure, respiratory failure, diabetes mellitus and much more.
Types of sepsis
Depending on the location of the primary source of infection, primary (cryptogenic) and secondary sepsis are distinguished. In primary cases, the source of infection cannot be determined. In secondary sepsis, such a focus is present. Depending on its location, there are:
- Percutaneous sepsis. The primary focus is on the skin; these can be wounds, burns, purulent skin diseases (purulent abscesses, boils, etc.).
- Odontogenic sepsis. The cause of its development can be caries, pulpitis, periodontitis, maxillary osteomyelitis and other diseases of the dental system.
- Otogenic sepsis. The primary focus is the inflammatory process in the ear. As a rule, these are purulent otitis media of the middle ear.
- Gynecological sepsis - the primary focus is located in the woman’s genital organs.
- Surgical sepsis - develops as a result of infection of a surgical wound or infection during invasive procedures. [2-4]
Book a consultation 24 hours a day
+7+7+78
Specialists
| 4.9 269 reviews | Chekulaeva Natalya Petrovna Infectious disease specialist Experience 37 years Admission from 2900 rub. |
| 4.7 10 reviews | Mazur Elena Vladimirovna Infectious disease specialist 18 years of experience Admission from 3110 rub. |
| 4.4 4 reviews | Minaeva Tatyana Yurievna Infectious disease specialist 35 years of experience Doctor of the highest category Admission from 3110 rub. |
The first signs and symptoms of sepsis
Identifying the first signs of sepsis can be difficult, even for specialists. This is due to the fact that, firstly, this syndrome develops against the background of an existing pathology, which can have a wide variety of symptoms, and secondly, in the presence of immunodeficiency, the clinical picture can be erased. However, there are some symptoms that suggest the onset of sepsis:
- Increase or decrease in body temperature - above 38 and below 36 degrees.
- Pressure drop below operating value.
- Increased heart rate.
- Increased frequency of breathing movements (shortness of breath).
- Decreased amount of urine excreted.
- General weakness, exhaustion.
- Impaired consciousness or behavior.
Particular attention is paid to the occurrence of these signs in chronic patients, in the presence of leukopenia, cancer, and in patients who have undergone trauma or surgery. If at least 2-3 of these symptoms occur, you should immediately contact your doctor.
Symptoms of chronic sepsis
Chronic sepsis occurs over a long period of time and is characterized by a sluggish course, the symptoms are mild. Therefore, diagnosing chronic sepsis is often difficult.
There is an opinion among experts that even acute sepsis should be considered as a two-phase disease with a chronic component. Even if the patient can be cured in the acute period, the disease often does not go away without a trace. Disorders persist that lead to chronic critical illnesses and can cause death.
Diagnosis of sepsis
Timely diagnosis of sepsis is crucial for the patient’s recovery. The earlier treatment is started, the greater the chances of success. The diagnosis is made on the basis of clinical examination and laboratory and instrumental examination.
Clinical criteria:
- Body temperature is more than 38 degrees or less than 36 degrees.
- Heart rate is more than 90 or exceeds the age norm.
- Respiration rate more than 20 times per minute.
- Presence of edema.
- Confusion.
- An increase in blood glucose levels of more than 7.7 µmol/l in the absence of diabetes.
- Disturbance of hemodynamic processes - a decrease in systolic blood pressure of less than 90 mmHg, or its decrease by more than 40 mmHg. from the usual meaning. [5,6]
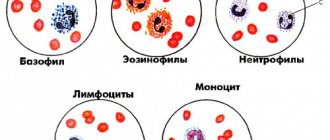
Laboratory criteria
A general blood test is performed with a leukocyte count and platelet count. In case of sepsis, leukocytosis is determined by more than 12*109/l or leukopenia when the number of leukocytes is below 4*109/l. There is also the release of immature forms of granulocytes into the bloodstream and a decrease in the number of platelets.
A biochemical blood test shows an increase in C-reactive protein, creatinine, and bilirubin. But these are nonspecific signs that can be observed in other diseases. Therefore, the search for more informative diagnostic methods continues.
Today, the main such markers are procalcitonin, presepsin, and CRP. Based on this laboratory indicator, a diagnosis is made and the dynamics of the disease are monitored.
Bacteriological culture
Detection of microorganisms in the blood is an important, but not mandatory, manifestation of sepsis. Even with the use of the most modern diagnostic systems and careful adherence to material sampling techniques, it is possible to isolate the pathogen from the blood in less than half of the cases. Therefore, a negative culture result in the presence of clinical symptoms should not be regarded as the absence of sepsis, and, conversely, the isolation of microorganisms from the blood in the absence of symptoms should be regarded as transient bacteremia or viremia, but not as sepsis.
However, biological studies should in any case be present as one of the stages in diagnosing sepsis for the following reasons:
- Possibility of determining the etiology of the pathogen.
- Selection or change of antibiotic treatment regimens.
- Monitoring the effectiveness of treatment.
- In some cases, it allows you to determine the source of infection, for example, catheter-related infection, endocarditis, etc.
Book a consultation 24 hours a day
+7+7+78
Diagnostic measures
If sepsis is suspected, it is necessary to find the cause of the infection, its causative agent. It is important to understand to what extent the functioning of the body’s functions is impaired, and then determine treatment tactics.
Among the diagnostic methods:
- Tests to determine infection;
- Coagulogram;
- Analysis of platelet counts and electrolytes;
- Analysis of kidney and liver activity;
- Determining the sufficiency of oxygen supply to tissues;
- Analysis of the activity of the cardiovascular system;
- X-ray examination;
- Ultrasound;
- CT;
- MRI.
Cirrhosis
Stages of sepsis development
The development and course of the septic process is individual and depends both on the properties of the pathogen and on the characteristics of the patient’s body. However, several phases of the course of this disease can be distinguished:
- Voltage phase. In response to the introduction of the pathogen, the body’s defense systems are activated and mobilized, in particular the pituitary-adrenal system is activated.
- Catabolic phase. The patient's condition deteriorates due to metabolic disturbances. The processes of metabolism of proteins, fats and carbohydrates are enhanced, and they are extracted from the “depot”. Disorders of water-electrolyte metabolism and acid-base status also develop.
- Anabolic phase. At this time, recovery processes begin. This primarily concerns structural proteins.
- Rehabilitation phase. During this period, further restoration of metabolic processes occurs. In some cases, complete recovery is not possible.
As for the duration of the disease, everything is again individual. In some, stronger patients, sepsis is relieved within 3-4 weeks, in others it can last for years, periodically subsiding and flaring up.
In addition, when diagnosing sepsis, the following conditions are distinguished.
Toxic-resorptive fever
Toxic-resorptive fever is a condition that develops when bacterial toxins or tissue decay products are absorbed from the primary pathological focus. As a rule, this is typical for bacterial infections of wounds, catheters, etc. There are common typical syndromes that accompany infectious processes - fever, changes in general blood and urine tests (leukocytosis, proteinuria). Once the primary lesion is eliminated, the patient's condition stabilizes.
Septicemia
Septicemia is a form of sepsis in which there is a pronounced intoxication syndrome, hyperergy (increased reactivity of the body) and a rapid course. Septic foci are either minimally expressed or absent. This form of sepsis is more typical for children in the first years of life. The clinical picture is more characterized by general manifestations:
- Hemolytic jaundice, accompanied by yellowing of the skin and sclera.
- Rash. It first appears as small pink dots, which grow and merge with each other, forming pale pink or purple spots.
- In some patients, elements of the rash may become blistered or ulcerated. With deep lesions, subcutaneous fatty tissue may be affected with the development of phlegmonous inflammation.
- Hemorrhagic syndrome - hemorrhages in internal organs.
Septicopyemia
Septicopyemia is a form of sepsis in which in the body, in addition to general intoxication, metastatic abscesses begin to appear in organs and tissues, which are the result of bacterial embolism. Most often, the first abscesses are found in the lungs, and then the process spreads to other organs: liver, liver, heart, meningeal membranes, synovial membranes. Abscesses can break through and cause the development of pleural empyema, phlegmon, peritonitis, etc.
Causes of blood poisoning
The causative agents of sepsis are a variety of microorganisms: staphylococci, meningococci, pneumococci, Escherichia coli, Mycobacterium tuberculosis, Klebsiella, Candida type fungi, and viruses of the herpetimorph group.
It is worth noting that the development of sepsis is associated not so much with the properties of the pathogens themselves, but with the state of the human body and its immunity. A decrease in the effectiveness of protective barriers leads to the fact that our security systems can no longer localize harmful pathogens in a timely manner, much less prevent their penetration into various organs.
If we talk about the most common methods of infection with sepsis, it is worth noting that they depend on the type of specific pathogen. Each of them has its own characteristics and epidemiological prerequisites. The only exceptions are cases where patients develop nosocomial sepsis, the symptoms of which sometimes make themselves felt even after inhaling poorly purified air in the wards (potentially dangerous microorganisms are detected in 60% of samples).
It is also possible to identify other routes of infection that determine the main symptoms of sepsis:
- obstetrics and gynecology;
- otogenic;
- cryptogenic;
- percutaneous sepsis;
- oral;
- blood poisoning resulting from surgical and diagnostic procedures.
Identifying the “gate” through which sepsis entered is of great importance for the successful treatment of patients. Early diagnosis of sepsis allows you to identify the infection in time, separate it from cases of short-term presence of microbes in the blood and activate the body's defense systems.
As we said above, for the development of sepsis certain conditions must be met, in particular:
- the formation of secondary foci, which subsequently also supply pathogens;
- the presence of a primary focus (it must be associated with the circulatory system or lymphatic vessels);
- repeated penetration of pathogens into the blood;
- the body’s inability to organize the necessary immune defense and provoke reactions against harmful microbes.
Only if all these conditions are met and the patient has appropriate clinical signs of infection, doctors diagnose blood sepsis. The development of sepsis is provoked by serious diseases (diabetes, cancer, rickets, HIV, congenital defects of the immune system), therapeutic measures, injuries, long-term use of immunosuppressive drugs, radiotherapy and some other factors.
Clinical classification of sepsis by stages
Clinical staging of sepsis plays an important role, as it helps doctors choose the optimal tactics and achieve the best possible treatment results in each specific case. The following stages are distinguished:
- Sepsis is diagnosed when the core temperature (measured on the mucous membranes) of the body rises above 38 degrees or falls below 36 degrees, heart rate 90 bpm or more, respiratory rate 20 bpm or more, or partial pressure of carbon dioxide in arterial blood (PaCO2 ) falls below 32 mm. Hg Art. In this case, the level of leukocytes in the blood rises to more than 12,000/μl or falls below ≤4000/μl, or more than 10% of immature forms appear among them.
- Severe sepsis is sepsis that is combined with acute organ dysfunction.
- Septic shock is diagnosed when a patient has persistent hypoperfusion (low blood pressure) or tissue hypoperfusion (insufficient blood supply) despite adequate fluid resuscitation.
- Multiple organ dysfunction syndrome is a condition in which the patient has organ dysfunction (impaired functioning of internal organs), and its homeostasis cannot be maintained without drug intervention.
Signs of septic shock
With septic shock, disruptions in the functioning of the circulatory system begin - oxygen and necessary substances do not reach the body tissues. Septic shock often results in death. In addition to a confirmed infection, septic shock is diagnosed when:
- increased content of lactic acid in the body, which is called serum lactate, in this case oxygen does not fully reach the cells;
- the need to take medications to maintain blood pressure at approximately 65 mmHg.
Treatment of sepsis
Treatment of sepsis is based on three principles:
- Sanitation of the primary lesion. This can be achieved with surgery and/or adequate antibiotic therapy. If a primary lesion is discovered that can be treated surgically, it is necessary to do this as soon as possible. This may include opening and drainage of abscesses, removal of infected invasive devices (catheters, implants, etc.), drainage and lavage of the abdominal cavity, etc.
Antimicrobial therapy is another cornerstone of sepsis treatment, and its timeliness and adequacy are important. For example, if septic shock develops, drugs should be administered within an hour of the onset of symptoms. In this case, the drug must cover the entire spectrum of suspected pathogens and, importantly, penetrate the primary infectious focus. If it is necessary to prescribe combination therapy of several drugs, they are used for no more than 5 days, after which data from biological research methods must be obtained and the treatment regimen must be adjusted. [7]
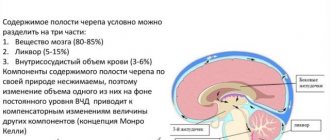
- Ensuring oxygen transport - all clinical manifestations of sepsis are aggravated in conditions of lack of oxygen, so it is very important to control this process. To do this:
- Hemodynamic support - infusion of solutions that ensure replenishment of water and electrolyte balance, medications are prescribed to maintain blood pressure, etc.
Respiratory support - artificial ventilation, oxygen masks, etc.
- Correction of metabolic disorders
- Ensuring the supply of necessary nutrients (proteins, fats, carbohydrates). If the patient is unable to take food or nutritional formulas on his own, replacement therapy is considered.
Monitoring glucose levels.
- Detoxification activities. [8-10]
One of the effective ways to treat sepsis is selective sorption on TORAYMYXIN columns. This technique is successfully used in many countries around the world. Currently, more than 200 thousand patients with septic shock and severe forms of sepsis have undergone such treatment. The effectiveness and safety of the technology has been confirmed in clinical studies. [11,12]
Complications of sepsis
- Complications from the respiratory system. Impaired ventilation of the lungs leads to an increase in the air-hematic barrier and, as a result, sweating of fluid into the alveoli. This further disrupts gas exchange and leads to the development of shock lung and respiratory distress syndrome, which is aggravated by fatigue of the respiratory muscles.
- Kidney complications. There is a decrease in the filtration function of the kidneys due to damage to the tubules, which developed as a result of a decrease in pressure. Accompanied by a sharp decrease in urine output, proteinuria, and azotemia.
- Impaired blood clotting due to a drop in platelet levels and the development of disseminated intravascular coagulation syndrome - a dangerous condition in which first there is massive formation of blood clots in the bloodstream, and then massive bleeding due to insufficiency of blood clotting factors.
- Neurological complications. Long-term sepsis can lead to the development of polyneuropathy, which, in particular, leads to weakening of the respiratory muscles and the inability to breathe independently.
- Septic shock is the most severe manifestation of sepsis, accompanied by a persistent decrease in blood pressure that is difficult to restore even with the use of fluid therapy and vasopressors. It develops due to the release of fluid from the blood vessels and due to general dehydration. At the same time, the violations are so severe that they can lead to the death of the patient from multiple organ failure. [13]