Complexes with this research
Expanded hospital complex Expanded infectious screening for prevention and hospitalization 4,390 ₽ Composition
Examination during pregnancy. 3rd trimester 5,820 ₽ Composition
Miscarriage Identification of the main causes of miscarriage RUR 28,220 Composition
IN OTHER COMPLEXES
- Joining IVF RUB 15,090
- Female infertility RUB 9,760
- Examination during pregnancy. 1st trimester 10,260 RUR
- Extended coagulogram RUB 2,790
- Coagulogram RUB 1,190
Prevention of bleeding disorders during pregnancy
In order to avoid pregnancy complications, all pregnant women must undergo laboratory tests - a clinical blood test, a coagulogram (blood clotting parameters), and determination of homocysteine levels.
Women who have previously had miscarriages or frozen pregnancies, as well as those pregnant as a result of IVF, are at risk for developing disorders in the hemostatic system. For patients at risk, it is recommended to conduct a complete study of the hemostatic system, blood testing for antiphospholipid antibodies. In the case of IVF (in vitro fertilization), monitoring of blood clotting parameters must be carried out throughout pregnancy. In accordance with the recommendations of the WHO (World Health Organization) expert committee, monitoring of coagulogram and D-dimer must be performed at least once every 2 weeks. Correction of such disorders is carried out jointly by a gynecologist and a hematologist.
Ideally, it is advisable to carry out a full examination not after pregnancy, but at the stage of family planning.
At the Clinic of High Medical Technologies named after. N.I. Pirogov has established and operates a system for diagnosing and treating patients with problems in the hemostatic system. Laboratory diagnostics, including genetic studies, can identify the causes of disorders. Treatment of such patients at the stage of family planning and their management during pregnancy (both physiological and as a result of IVF) is carried out by qualified gynecologists together with a hematologist.
Detailed description of the study
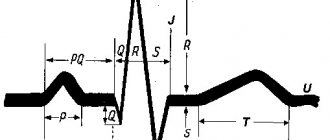
Fibrinogen, or factor I, is a plasma protein that is produced in the liver and plays an important role in the blood clotting process (hemostasis). Through various interactions, it plays an important role in stopping bleeding.
Fibrinogen is able to dissolve in plasma and serves as a precursor to the insoluble protein fibrin. The process of converting fibrinogen into fibrin, as well as the adhesion (aggregation) of platelets, is carried out with the help of three main enzymes that regulate hemostasis - thrombin, plasmin and factor XIIIa.
As a result, a blood clot is formed, consisting of fibrin strands and an accumulation of platelets. This helps stop bleeding effectively. The fibrin clot also activates the fibrinolytic system. This maintains a balance between blood clotting and protection against blood clots.
The amount of fibrinogen in the body may vary among individuals depending on age and gender. A physiological increase in the concentration of this protein is observed in pregnant women. Its level may also increase with age.
Pathological conditions that change the fibrinogen content in the body are divided into congenital and acquired. The first group of diseases is associated with mutations in genes. Some of them lead to fibrinogen deficiency in the blood, others increase its level. The presence of single mutations in the genes encoding the formation of this protein may not have any symptoms, but increases the risk of thrombosis with unfavorable concomitant factors.
Acquired diseases in which fibrinogen concentration increases primarily include infectious or other diseases accompanied by inflammation. Among them one can also note diabetes mellitus and obesity. Injuries and burns increase fibrinogen production, which is necessary to stop bleeding. An increased content of this protein is observed during pregnancy, as well as when taking estrogen hormones.
A decrease in fibrinogen levels is caused by a violation of its formation in the liver or accelerated destruction in the blood (fibrinolysis). However, in most pathological conditions (acute and chronic inflammation, trauma, burns, surgical interventions), this indicator becomes higher than normal.
Determining the amount of fibrinogen in plasma is necessary in order to assess blood clotting ability and, if necessary, carry out treatment to normalize hemostasis.
Causes of deviations in coagulogram
During gestation, there is a risk of developing disseminated intravascular coagulation syndrome, the first stage of which is characterized by hypercoagulation, and the second by hypocoagulation (increased and decreased blood clotting, respectively) and is dangerous with massive bleeding.
The development of DIC syndrome is caused by blood clotting disorders that occur in the following situations:
- gestosis;
- premature placental abruption;
- placenta previa;
- amniotic fluid embolism;
- arterial hypertension;
- liver diseases;
- antiphospholipid syndrome;
- threat of miscarriage (infections, hormonal imbalance);
- Rhesus conflict pregnancy;
- antenatal fetal death;
- hemorrhagic shock;
- chronic extragenital diseases of the mother (kidney disease, diabetes mellitus, systemic diseases).
Folate cycle gene defects and pregnancy
Genes involved in the metabolism of folic acid and vitamin B12 may play a certain role in miscarriage.
Folic acid (vitamin B9) is responsible for the transfer of methyl groups (CH3-) during chemical reactions in the body - these are reactions during which DNA, RNA and a number of amino acids (glycine, methionine) are synthesized. Therefore, it is so important for pregnant women and the fetus not to have a deficiency of both folic acid itself and the enzymes involved in its metabolism.
High concentrations of the active form of folate are required to convert homocysteine to methionine. The main genes whose products control the conversion of folic acid into metabolically active forms and regulate homocysteine metabolism are MTHFR (methylenetetrahydrofolate reductase), MTR (methionine reductase), and MTRR (methionine synthetase reductase). A decrease in the activity of these enzymes is one of the important reasons for the accumulation of homocysteine in the body.
Violation of embryo implantation (genes TP53, LIF and others)
It has now been proven that the expression of the LIF protein is a crucial factor for the formation of the so-called “implantation window”.
In the endometrium of women with infertility, the expression of LIF is reduced, and it has also been shown that in case of infertility of unknown origin, the expression of LIF is significantly reduced in the middle secretory phase of the endometrium.
The level of LIF is regulated by the p53 protein; accordingly, mutations in the genes of the TH53 gene signaling pathway indirectly affect the expression of LIF in the endometrium. These are mutations of the genes TP53, MDM2, MDM4, USP7 and some others (D. d'Avila Paskulin et al., 2012)
Embryo implantation disorders (LIF and TP53 gene network)
| Gene | Name | Polymorphism | Clinical significance |
| ESR1 | Estrogen receptor 1 | XbaI Polymorphism; A-351G; IVS1-351A>G | Co-regulation by both p53 and estrogens is required to ensure LIF expression at levels sufficient for blastocyst implantation. Considering that the function of the estrogen receptor with the rs9340799-G gene variant in the homozygous state (genotype G/G) is significantly reduced, we should expect a decrease in the amount of LIF and, as a consequence, impaired blastocyst implantation. |
| ESR1 | Estrogen receptor 1 | PvuII Polymorphism; T-397C; -397T>C | Co-regulation by both p53 and estrogens is required to ensure LIF expression at levels sufficient for blastocyst implantation. Considering that the function of the estrogen receptor with the rs2234693-C gene variant in the homozygous state (genotype C/C) is significantly reduced, one should expect a decrease in the amount of LIF and, as a consequence, impaired blastocyst implantation. |
| HTR1A | 5-hydroxytryptamine (serotonin) receptor 1A | C-1019G; -1019C/G | Homozygous carriers of the rs6295-C variant of the 5-HT1A gene (genotype C/C) exhibit significantly lower implantation rates. They are also characterized by significantly higher biochemical rates of pregnancy loss. PMID: 23499153 |
| LIF | Leukemia inhibitory factor | Val64Met; Val86Met; 3400 G/A; G3400A; Arg26His | The likelihood of idiopathic infertility and the likelihood of unsuccessful IVF in patients who are carriers of a mutant variant of the LIF gene are significantly increased compared to control groups. |
| LIF | Leukemia inhibitory factor | 1414A>C | An association of variant C of the rs929271 polymorphism in the 3 'UTR of the LIF gene with impaired blastocyst implantation was revealed. The occurrence of the C allele is much higher in women with idiopathic infertility under the age of 35 years, but not older. |
| MDM2 | MDM2 proto-oncogene, E3 ubiquitin protein ligase | T-410G; -410T>G | The rs2279744-G variant dramatically increases the expression of the MDM2-encoded protein. Increased amounts of MDM2 in turn inhibit p53, which reduces LIF levels and the likelihood of implantation. |
| MDM4 | MDM4, p53 regulator | rs1563828 | The presence of the T allele in the rs1563828 polymorphism of the MDM4 gene increases the expression of the p53 suppressor protein encoded by this gene. Inhibition of p53, in turn, leads to a decrease in the amount of LIF and the likelihood of implantation. |
| PTGS2 | Prostaglandin endoperoxide synthase (prostaglandin G/H synthase and cyclooxygenase) | G-765C; -765G>C | The -765C allele of the PTGS2 gene is associated with recurrent implantation disorders and is a molecular marker of reproductive dysfunction. |
| SLC6A4 | Neurotransmitter serotonin transporter | L/S; Long/Short; 44-bp Ins/Del | Homozygous carriers (L/L genotype) exhibit significantly lower implantation rates, lower clinical pregnancy rates (PR), and higher biochemical pregnancy loss rates (BPL). |
| TP53 | Tumor protein p53 | Arg72Pro; Ex4+119C>G; 12139G>C; R72P | The percentage of women carrying the Pro72 allele was significantly higher in the sample who underwent IVF due to an increased number of cases of implantation disorders. The Pro72 allele is a risk factor for the development of implantation failure. |
| USP7 | Herpes virus-associated ubiquitin-specific peptidase 7 | rs1529916; Hausp-A | In patients carrying the Hausp A allele (genotype A/A), there is a significant impairment of the function of the USP7 gene, which ultimately reduces the activity of p53. Loss of p53 activity entails a decrease in the expression of the LIF gene, which reduces the amount of the corresponding protein, which plays a key role in the process of blastocyst implantation |
Choosing a method of contraception.
When taking estrogen-containing contraceptives, blood clotting increases, which in the case of thrombophilia becomes simply dangerous to health and life.
Indications for prescribing a study for hereditary thrombophilia:
- the presence in the past of two or more fetal growth arrests in early pregnancy;
- the presence of severe pregnancy complications in the past (severe forms of late toxicosis, intrauterine fetal death, fetal growth retardation);
- the presence of relatives with thrombotic complications under the age of 50 years (deep vein thrombosis, pulmonary embolism, stroke, myocardial infarction, sudden death);
- several failed IVF attempts;
- increased levels of antiphospholipid antibodies and/or increased homocysteine levels;
- planning gynecological operations;
- planning hormonal contraception
Risk factors for thrombophilias:
- genetic predisposition (cases of thrombosis in relatives);
- diseases such as atherosclerosis, arterial hypertension, varicose veins, autoimmune diseases, thrombocytosis, erythremia, malignant neoplasms;
- history of stroke or heart attack;
- pregnancy;
- injuries and surgical interventions;
- sedentary lifestyle;
- obesity;
- taking hormonal contraceptives.
The main blocks of genes involved in the development of thrombophilia:
- Genes of the blood coagulation system (F2, F5, F7, FGB, SERPINE 1)
- Platelet factor genes (ITGA2, ITGB3)
- Folate cycle enzyme genes (MTHFR, MTRR, MTR)
- Genes responsible for endothelial dysfunction (ACE, AGT, NOS3)
- Genes responsible for monogenic hereditary thrombophilias (PROC, PROS)
Primary (genetically determined) thrombophilias include (10):
- G1691A mutation of the factor V gene (Leiden);
- G20210A mutation of the prothrombin gene (blood coagulation factor II);
- homozygous mutation C677T of the methyltetrahydrofolate reductase (MTHFR) gene;
- deficiency of natural anticoagulants (ATIII; protein C, S);
- sticky platelet syndrome;
- increased levels of homocysteine in the blood;
- increased activity or amount of factor VIII;
- rare causes (dysfibrinogenemia, deficiency of factors XII, XI, heparin cofactor II, plasminogen)
Frequency of various thrombophilias (10):
- Antiphospholipid syndrome – 28%
- Resistance to activated protein C – 25:
- Increased factor VIII levels – 25%
- Protein C deficiency – 10%
- Protein S deficiency – 10%
- Homocysteinemia – 10%
- Prothrombin G20210A – 5-10%
- Plasminogen deficiency – 2-3%
- Dysfibrinogenemia – 1.5%
- High PAI level – 1-3%
- Tissue plasminogen activator deficiency – 1%
The main mutations leading to hereditary thrombophilia:
| F5 | Coagulation factor 5 | Leiden mutation; G1691A; Arg506Gln | Inhibition of factor 5 degradation by activated protein |
| F2 | Coagulation factor 2 (prothrombin) | G20210A | Increased synthesis of prothrombin allele A, shift of equilibrium in the hemostatic system towards increased blood coagulation |
| F2 | Coagulation factor 2 (prothrombin) | Thr165Met | Increased thrombus formation |
| FGB | Fibrinogen, beta chain | C-148T | Increased fibrinogen gene expression, increased fibrin production, increased thrombus formation |
| FGB | Fibrinogen, beta chain | G-455A; G-467A | Decreased intensity of fibrinogen synthesis |
| MTHFR | Methylenetetrahydrofolate reductase | C677T; Ala222Val | The formation of a thermolabile form of the enzyme with reduced activity leads to impaired homocysteine methylation and an increase in its level in the blood. Hyperhomocysteinemia leads to damage to the vascular endothelium. |
| MTHFR | Methylenetetrahydrofolate reductase | A1298C; Glu429Ala | The mutation leads to thermolability of MTHFR ONLY when co-carried with the 677T mutation |
| ITGA2 | Glycoprotein Ia | С807T | Increased density of collagen receptors on the platelet surface, increased platelet adhesion to the endothelium |
| ITGB3 | Glycoprotein 3a | PIA1/PIA2; Leu33Pro | The mutation affects the aggregation properties of platelets |
| SERPINE1 | Plasminogen activator inhibitor type 1 | 4G/5G;Ins/Del G | Genotype 4G/4G - hypercoagulability |
| PROC | Protein C | 1201G>A; Asp401Asn | Autosomal dominant thrombophilia due to protein C deficiency |
| PROC | Protein C | 1042C>T Arg348Ter | Autosomal dominant thrombophilia due to protein C deficiency |
| PROS | Protein S | 773A>G; Asn258Ser | Autosomal dominant thrombophilia due to protein S deficiency |
| PROS | Protein S | 586A>G; Lys196Glu | Autosomal dominant thrombophilia due to protein S deficiency |
Diagram of folic acid metabolism
The reasons for the toxic effect of excess homocysteine on the body of a woman and fetus are as follows (6):
- homocysteine damages the vascular endothelium, which leads to stimulation of thrombus formation. This can lead to placentation disorders and fetoplacental circulation disorders, resulting in infertility and miscarriage;
- elevated levels of homocysteine in late pregnancy can cause placental insufficiency and, as a result, intrauterine growth retardation and chronic fetal hypoxia;
- There was a positive correlation between the level of homocysteine in the blood and the severity of gestosis.
| Gene | Name | Polymorphism: names and [synonyms] | Clinical significance |
| MTHFR | Methylenetetrahydrofolate reductase | C677T; Ala222Val; A222V | The 677T mutant variant of this polymorphism leads to the formation of a heat-labile enzyme and an increase in homocysteine levels in the blood |
| MTHFR | Methylenetetrahydrofolate reductase | A1298C; Glu429Ala; E429A | An increased frequency of the A/C and C/C genotypes for this polymorphism has been reported in women with recurrent early miscarriages. |
| MTR | Methionine reductase | Asp919Gly; A2756G | An increase in the frequency of occurrence of the 66A allele of the MTRR gene and the 2756G allele of the MTR gene was shown in women with a history of premature birth (after the 22nd week of pregnancy). |
| MTRR | Methionine synthetase reductase | Ile22Met; A66G | The MTRR A66C gene polymorphism is associated with Down syndrome and spinal cord defects. |