For everyone child's hematopoietic system characterized by extreme functional instability (lability), easy vulnerability to the most insignificant exogenous factors.
A decrease in the amount of hemoglobin, red blood cells, the appearance of immature elements of red blood, leukocytosis with the formation of young cells are observed in children much more often and develop faster than in adults. The formation of foci of extramedullary hematopoiesis, and sometimes a complete return to the embryonic type, can be caused in children not only by severe anemia and leukemia, as in an adult, but often occur under the influence of various infections, intoxications and other harmful factors (bronchopneumonia, pyelonephritis, otitis media and etc.). Blood for infections, analysis - children's clinic "Markushka"
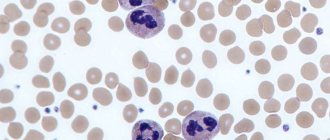
Peripheral blood of a healthy child
Erythrocyte system : erythropoiesis begins with a bone marrow stem cell that is sensitive to erythropoietin (a glycoprotein produced in response to tissue hypoxia in the fetal liver and the child’s kidney), and proceeds through its differentiation into an erythroblast, then into a pronormocyte, basophilic normocyte, polychromatophilic normocyte, oxyphilic normocyte, reticulocyte.
Of the estimated 18 divisions that occur during the transformation of a stem cell into a mature red blood cell, erythropoietin significantly stimulates the final 8-10 divisions. The preceding cell divisions that give rise to erythropoietin-sensitive erythroid progenitor cells are largely erythropoietin-independent.
The lifespan of red blood cells is 100-120 days. With the help of phagocytic macrophages of the spleen, liver, lungs, and lymph nodes, an average of 1.4% of red blood cells are destroyed per day.
Diagnosis of leukocytosis
Why does a child under one year bleed from the nose?
With leukocytosis, the number of “white” blood cells increases compared to their normal value. The increase may be slight or severe.
Thus, the level of leukocytes increases after eating or during exercise. These are physiological processes and do not pose any danger. After a short period of time, the indicators return to normal. If such growth is considered as a pathological reaction of the body, we are talking about an inflammatory process.
The famous pediatrician Komarovsky recognizes the need for a general blood test. It, first of all, allows you to determine the nature of the disease, bacterial or viral. This is the basis for subsequent treatment. If the body is attacked by bacteria, then it will be difficult to cope without antibiotics, but they have no effect on viruses. Therefore, their use does not make sense, just like the use of antiviral drugs. Immunity to them is usually developed on days 6-7, and the body copes on its own. If this does not happen and the disease develops, most likely a bacteria has joined.
Possible symptoms in a child
When a child's white blood cell count is elevated, it not only indicates that he or she is sick, but also that the immune system is active. The body's defenses began to fight pathogenic microorganisms.
- Leukocytosis (increased white blood cells in the blood): normal or pathological?
The following symptoms may indicate leukocytosis in a child:
- Increased body temperature without identifying the cause;
- Weakness and dizziness;
- Indigestion, lack of appetite, weight loss;
- Nausea, vomiting;
- Headache and migraine;
- Aches in joints and muscles;
- Sleep disorder, most often insomnia. The child becomes anxious and shudders;
- Increased sweating;
- Moodiness and irritability.
An infant will not be able to talk about his health; parents only have to guess about existing problems. What should alert you is that the baby’s behavior has changed, he is not the same as before. When this happens once, and then the baby becomes himself again, then there is no need to worry. If the condition drags on, behavior and well-being worsen, then you need to consult a pediatrician.
Upset child
We must remember! In a baby, a temperature of up to 37.5° is considered normal. At the same time, he is calm and active, no unpleasant symptoms are observed. This is often due to uncomfortable indoor conditions and too warm clothing. If the temperature is higher and the baby begins to act up, you should consult a doctor.
Composition of peripheral blood in a child
The composition of a child's peripheral blood undergoes significant changes in the first days of life after birth. Immediately after birth, red blood is characterized by an increased hemoglobin content and a large number of red blood cells. From the end of the 1st to the beginning of the 2nd day of life, a decrease in the content of hemoglobin and red blood cells occurs.
The blood of a newborn by a distinct anisocytosis, observed within 5-7 days, and macrocytosis (the diameter of erythrocytes is somewhat larger in the first days of life - up to 8.5-9 µm, the norm is 7.5 µm). The blood of a newborn contains many young red blood cells, which indicates the active processes of erythropoiesis. During the first few days of life, it is possible to detect nucleated forms of erythrocytes in the blood, most often normocytes and erythroblasts. The number of reticulocytes in the first hours of life ranges from 8 to 42%. The high content of erythrocytes and hemoglobin, as well as immature forms of erythrocytes in the peripheral blood in the first days of life indicates intensive erythropoiesis as a reaction to the lack of oxygen supply to the fetus during intrauterine development and during childbirth.
After birth, due to the establishment of external respiration, hypoxia is replaced by hyperoxia
After birth, due to the establishment of external respiration, hypoxia is replaced by hyperoxia . This causes a decrease in erythropoiesis and a drop in the number of red blood cells and hemoglobin levels. Red blood cells produced in utero have a shortened lifespan compared to that of older children and are more prone to hemolysis. The lifespan of red blood cells in children in the first days of life is 12 days, which is 10 times less than in adults and older children.
The erythrocyte sedimentation rate (ESR) depends on many chemical and physical properties of the blood. In a newborn, ESR is 2 mm/h, in young and older children - 4-8 mm/h, in adults - 5-8 mm/h. Slower erythrocyte sedimentation in newborns is explained by low levels of fibrinogen and cholesterol in the blood, as well as blood thickening, which is especially pronounced in the first hours after birth.
Why are leukocytes elevated: possible diseases
In some cases, indicators exceed acceptable values due to a pathological process. The reasons for this may be:
- Worm infestation. Any intestinal parasites (worms are more often detected in children, especially if they have cats/dogs and live in their own home) provoke elevated leukocytes in the blood and a high level of eosinophils.
- Allergy. The entry of an allergen into the body immediately responds with leukocytosis. If inflammation occurs at the site of an allergic reaction (itching, swelling, redness), this immediately provokes additional production of leukocytes.
- Diseases of the spleen. The spleen is an organ for recycling outdated leukocytes. When it is damaged or splenectomy (operation to remove the spleen), significant, long-term leukocytosis is observed.
- Autoimmune disorders. The most serious causes of leukocytosis lie in the autoimmune aggression of leukocytes against the body's own cells. The failure that led to this pathological condition is observed in lupus erythematosus and rheumatoid arthritis.
- Endocrine pathology. For example, with hypothyroidism (insufficient thyroid function), basophilia is observed - an increase in the level of basophils.
- Blood loss, hemolytic anemia. A decrease in the number of red blood cells in the blood due to blood loss or anemia causes the bone marrow to work harder. At the same time, new (immature) leukocyte cells are also synthesized, so these conditions are almost always accompanied by neutrophilic leukocytosis.
- Oncology. A very important sign: very often with oncology, a large number of monocytes are found in the blood. Fluctuations in leukocytes from 0.1 to 300 x 109/l (from leukopenia to large-scale leukocytosis) are observed in leukemia, a cancerous degeneration of leukocytes.
Leukocyte system
Leukocyte system : leukopoiesis begins with a bone marrow stem cell and proceeds through its differentiation into a myeloblast, then into basophilic, neutrophilic and eosinophilic segmented cells through the phases: promyelocyte - myelocyte - band cells.
Neutrophils are continuously supplied to the skin, mucous membranes and other peripheral tissues. Their daily turnover is about 100 billion cells. The lifespan of granulocytes is from 14 to 23 days. Neutrophils spend most of their lives in the bone marrow. On their way to peripheral tissues, neutrophils spend about 10 hours in the intravascular space, and at any moment only half of the intravascular cells are in motion, while the other reversibly adheres to the endothelial surface of the vessels (mural cells). The latter are a reserve pool of mature cells that can be called upon in case of infection or inflammation.
Features of the number of leukocytes
There are features and numbers of leukocytes . In the peripheral blood in the first days after birth, the number of leukocytes is 18-20 -109/l, with neutrophils predominating (60-70%). The leukocyte formula is shifted to the left due to a large number of band forms and, to a lesser extent, metamyelocytes (young).
With age, the leukocyte formula undergoes significant changes
This is reflected in a decrease in the number of neutrophils and an increase in the number of lymphocytes . On the 5th day of life, their number is comparable (the so-called first crossover), amounting to about 40-44% in the white blood formula with a ratio of neutrophils and lymphocytes of 1:1. Then there is a further increase in the number of lymphocytes (by the 10th day to 55-60%) against the background of a decrease in the number of neutrophils (approximately 30%). The ratio between neutrophils and lymphocytes will be 1:2.
Gradually, by the end of the 1st month of life, the shift of the formula to the left disappears, myelocytes completely disappear from the blood, the content of band forms decreases to 4-5%.
By the beginning of the 2nd year of life, the number of lymphocytes begins to decrease, and the number of neutrophils increases, respectively, by 3-4% of cells per year, and at 5 years a “second crossover” is observed, in which the number of neutrophils and lymphocytes is again compared (1:1 ratio) . After 5 years, the percentage of neutrophils gradually increases by 2-3% per year and by 10-12 years reaches values like those of an adult - about 60%. The neutrophil to lymphocyte ratio is again 2:1.
This parallelism of changes in neutrophils and lymphocytes can be explained by the commonality of their functional properties, which play a role in immunity. The lifespan of lymphocytes is 100-300 days.
Absolute and relative neutrophilia in the first days after birth is explained by the entry of maternal hormones into the child’s body through the placenta, thickening of the blood in the first hours of extrauterine life, resorption of interstitial hemorrhages, and adaptation of the body to external conditions.
The content of eosinophils, basophils, and monocytes practically does not undergo significant changes during the growth of the child. The number of leukocytes further decreases to (7.6-7.9)x10(9)/l.
Diagnostics
A general blood test will help detect leukocytosis.
For this study, you will need biological material taken from a finger, or less often from a vein. In order for the hematologist, whose competence is to decipher the results, to receive the most reliable information, patients need to donate the main biological fluid on an empty stomach - at least 8 hours must pass after the last meal. No other preparation is required from children. Since all blood components are interconnected, in addition to a shift in the leukocyte mass, other disorders may develop, for example, lymphocytes, basophils, neutrophils, monocytes and eosinophils will be decreased or increased. Often the ESR accelerates and leukocytes are higher than normal.
However, the data from this diagnostic laboratory test will not be enough to identify the reasons behind the increase in white blood cells. To identify the etiological factor, a comprehensive examination of the body will be required.
First of all, it is necessary to implement measures carried out directly by the clinician, for example:
- familiarization with medical histories to search for the root cause, which has a pathological basis;
- collection and analysis of life history - this includes information regarding the child’s consumption of any medications, food preferences and general lifestyle;
- a thorough physical examination of the patient;
- a detailed survey of the patient or his parents regarding the first time of occurrence of characteristic signs, as well as for the clinician to compile a general symptomatic picture.
Additional diagnostic measures may include specific laboratory tests (general urine analysis or stool microscopy, as well as bacterial blood culture), instrumental procedures (ultrasonography, radiography, CT, MRI) and consultations with specialists from other fields of medicine. The accompanying diagnostic program will be purely individual.
Ultrasonography
Platelets
Platelets , like all other blood cells, originate from a bone marrow stem cell with subsequent differentiation: thrombopoietin-sensitive cell - megakaryoblast - promegakaryoblast - megakaryocyte - platelet. About 35-40% of circulating platelets are destroyed daily due to aging and the body's ongoing clotting process.
Platelets are directly involved in the process of hemostasis. The activity of platelet coagulation factors in newborns and infants is reduced. The duration of bleeding is not changed, the clotting time may be prolonged, especially in children with severe jaundice (over 6-10 minutes).
Hematocrit number , which gives an idea of the percentage ratio between formed elements and blood plasma, varies depending on age. The hematocrit value increases in cyanotic congenital heart defects, in a state of dehydration, etc. A decrease in hematocrit is observed in anemia and diseases accompanied by hydremia.
Red blood: what is it?
Yeah. The blood test is divided into two parts. The first part is the so-called “red blood”, that is, hemoglobin, red blood cells, platelets and color index. All this fraternity is responsible for the transfer of oxygen into cells and does not suffer much during infection. You and I just need to quickly go through the standards and, making sure that everything is fine, move on to the second part.
Norms
Hemoglobin (aka Hb) is measured in grams per liter (!) of blood and is responsible for the transport of oxygen.
A one-month-old child has a hemoglobin norm of 115-175 (this is not an adult, everything is more complicated here), at six months - 110-140 - the same as you and I, and so, in fact, right up to 10-12 years. 110-140 (145 according to other sources) grams per liter of blood.
Red blood cells , also known as RBCs, are cells in which hemoglobin floats in the blood. They carry oxygen with the help of hemoglobin. The norm for a child per month will be 3.8-5.6 - attention! - trillions of red blood cells per liter of blood. A one-year-old child (like an adult) already has fewer of these same trillions - 3.5-4.9 per liter of blood. What to do - if you pump out blood for analysis in liters, everything has to be counted in trillions. No problem, it will be easier next time.
Reticulocytes , also known as RTC, their number is measured, thank God, as a percentage. These are, so to speak, young red blood cells; they should not be more than 15% in children under one year old and no more than 12% in children over one year old or in adults. The lower limit of normal for reticulocytes is 3%. If there are fewer of them, the child is on the verge of anemia, and measures must be taken as soon as possible.
Platelets . English abbreviation PLT. There are significantly fewer of them than red blood cells - their number is measured “only” in billions per liter of blood, the norm is from 180 to 400 for children under one year old and from 160 to 360 for children over one year old or in adults. Platelets are actually not cells at all, but rather fragments of a giant precursor cell, from these fragments, in which case blood clots are formed - for example, to stop bleeding if the baby, God forbid, gets injured.
ESR (ESR). These are not even cells at all, but an indicator of the erythrocyte sedimentation rate - the higher this rate (and this is not a car, here the speed is measured in millimeters per hour), the more active the inflammatory process, for which you may have been recommended to take a blood test. ESR norms at 1 month are 4-10, at 6 months 4-8, but from one year to 12 years - from 4 to 12 mm per hour. Then the norms of that same ESR will also differ depending on gender, but that’s a completely different story.
In addition to these indicators, there are many others - hematocrit (HCT), red blood cell distribution width (RDWc), mean erythrocyte volume (MCV), mean erythrocyte hemoglobin content (MCH) and even mean erythrocyte hemoglobin concentration (MCHC). All these indicators serve to diagnose anemia, so it would be better for you and me (we are talking about infections, remember?) to postpone their discussion until later.
What is much more important for us is not the oxygen transport system, but the body’s defense system against infections. This is the so-called white blood, leukocytes. Here we will dwell on it in very, very detail.
Peripheral blood in premature infants
The red blood of a healthy premature baby at birth is characterized by erythroblastosis, reticulocytosis, increased red blood cell and hemoglobin counts, as well as anisocytosis and poikilocytosis. Soon after birth, there is a gradual drop in the content of red blood cells and hemoglobin, and by the 2-3rd month of life, most preterm infants develop anemia, known as “early anemia of prematurity.” Its pathogenesis is based on increased hemolysis and functional immaturity of bone marrow hematopoiesis. The cause of intense hemolysis is the predominance of unstable red blood cells containing fetal hemoglobin in the blood of premature babies.
Thus, in healthy premature infants, anemia in the 2-3rd month of life can be considered as a manifestation of adaptation when replacing extramedullary hematopoiesis with bone marrow. In sick children, early anemia is often accompanied by more pronounced changes in the content of red blood cells and hemoglobin and has a long course.
By the beginning of the 4th month, there is a spontaneous increase in the level of red blood cells and hemoglobin, but a month later there is a repeated decrease in levels and late anemia of prematurity develops, caused by a lack of iron in the body. Unlike early, late iron deficiency anemia can be prevented and effectively treated with iron supplements.
Symptoms
Elevated leukocytes in a child’s blood have their own clinical picture.
It is worth noting that the symptoms expressed in this disorder are nonspecific and cannot accurately indicate the course of this particular disorder. In addition, external manifestations characteristic of this condition may go unnoticed, since the symptoms of the underlying disease often come to the fore.
It is very difficult to determine the increase in the number of white blood cells in the blood of an infant. This is due to the fact that infants cannot describe their condition and sensations in words.
Symptoms that develop due to the fact that the child’s white blood cells have increased include:
- constant fatigue;
- loss of appetite;
- increase in temperature indicators;
- dizziness;
- profuse sweating;
- sleep disorder;
- slight decrease in visual acuity;
- muscle and joint pain;
- weight loss;
- frequent mood changes;
- increased moodiness and tearfulness in infants;
- problems with concentration in older children;
- decreased physical activity.
Such external manifestations are common to all age categories. The only difference may be the intensity of symptoms.
Blood in children after one year of age
Blood in children over the age of one year also has its own characteristics. The amount of hemoglobin in children over 1 year of age clearly increases, gradually approaching the figures of an adult, although at this age there are significant individual fluctuations. The number of red blood cells also increases in parallel; their absolute quantities and growth rates in children of different ages are subject to fairly wide individual fluctuations. The number of erythrocytes with supravital granularity gradually decreases, reaching by school age the figures characteristic of adults, that is, about 2%. The color index ranges from 0.85 to 0.95.
It should be noted that recently, in both children and adults, some changes : a trend towards a decrease in the number of leukocytes is definitely emerging (in children aged 2 to 15 years).
Types of leukocytes
White blood cells - leukocytes
Leukocytes are white bodies of different sizes that are part of the blood. This is a general name for groups of cells, each of which performs its own function, and all together are active defenders of the body.
Types of leukocytes:
- Neutrophils (NEU). They absorb and digest bacteria, fungi and some viruses. When dying, neutrophils release a large amount of biologically active substances that destroy the remaining harmful substances.
- Eosinophils (EOS). Their function is to combat the allergen, as well as helminths and their larvae. They absorb foreign proteins and dissolve them with their enzymes. In the fight against larvae, eosinophils destroy their granules, which leads to the destruction of worm embryos.
- Basophils (BAS). Helps expel and destroy ticks and helminths. But the main task is to maintain natural blood flow, protect blood vessels from the formation of blood clots, and help other leukocytes reach the source of inflammation.
- Lymphocytes (LYM). They destroy viruses, bacteria, dead and cancer cells, regulate the activity of other leukocytes, and produce antibodies. The production of antibodies, that is, protein molecules, allows the body to create protection against each individual virus and bacteria, neutralizing their effect and preventing reproduction.
- Monocytes (MON). The largest leukocytes not only absorb large particles of viruses, microbes, bacteria, but also clean the site of the pathogenic factor. They free the body from dead cells and promote the restoration of damaged tissues.
How is the analysis performed?
When testing blood for a general or, as it is also called, clinical analysis, the child should, if possible, be hungry, i.e., the procedure is done on an empty stomach. Typically, blood collection rooms in clinics are open from 8.00. until 9.30. At this time, blood levels in the body are the most optimal.
Blood must be donated on an empty stomach, because after eating, the stomach begins to work actively and the number of leukocytes may increase, and this, in turn, may give the doctor incorrect information about the child’s health status. Also, before taking the test, you should not undergo any procedures, such as x-rays, FGDS and various physiotherapeutic procedures, this can also lead to an increase in leukocytes in the blood. [adsen]