The importance of blood can hardly be overestimated: it carries oxygen and nutrients to tissues, helps regulate the functioning of the body by transporting hormones and other active substances, helps regulate temperature and performs a host of other tasks.
Obviously, a decrease in blood volume has a negative impact on the overall functioning of the body.
However, nature provides a mechanism for protecting against excessive blood loss - the ability of blood to thicken and coagulate, covering the damaged area. The level of blood clotting is a kind of indicator of the body’s survival.
Coagulation indicators and their norm in children
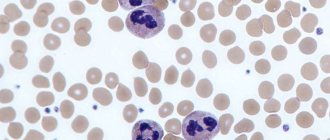
Blood is not a homogeneous liquid, but a suspension of many cells in a water-protein solution - plasma.
There are many types of blood cells, which (to simplify somewhat) can be divided into three groups.
- The first is erythrocytes, also known as red blood cells, which transport oxygen to tissues.
- The second is leukocytes, white blood cells that absorb and neutralize foreign objects (viruses, bacteria, etc.).
- The third is platelets, the cells responsible for the ability of blood to clot.
When the integrity of the vessel wall is damaged, special substances are released from the damaged tissues, the so-called coagulation factors (mainly proteins).
They activate platelets and cause them to stick to the edges of the wound and connect with each other, forming a dense clot that covers the damaged area.
In turn, platelets also secrete a special substance that activates the fibrinogen protein dissolved in the plasma.
It begins to transform into the protein fibrin, which is capable of forming long elastic cords in which red and white blood cells “get stuck.” Thanks to this, the clot covering the wound becomes denser, and its edges begin to tighten.
The blood clotting process is characterized by many indicators.
- Platelet level is the number of cells responsible for the blood clotting process.
- The duration of bleeding is the time that passes from the moment the integrity of the vessel is damaged until a blood clot forms.
- Clotting time is the duration of formation of a blood clot.
- Prothrombin time is the rate of activation of a certain factor (namely factor VII, proconvertin) involved in the “launch” of the coagulation process in the early stages. This factor activates the formation of thrombin, a substance that promotes the conversion of fibrinogen into fibrin. In other words, this is the rate of formation of a blood clot after exposure to substances from the tissues of a damaged vessel.
- Thrombin time is the rate at which fibrinogen is converted into fibrin.
- Activated partial thromboplastin time (aPTT) is the duration of the formation of a blood clot without the participation of external factors, i.e., without damage to the vascular walls and the release of corresponding substances, solely due to factors initially present in the blood in an inactive state.
- Fibrinogen level is the amount of fibrinogen protein that can be converted into fibrin.
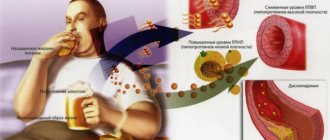
- Antithrombin III level is the level of antithrombin III protein in the blood, which prevents blood clotting. This protein is needed in the blood so that coagulation processes, relatively speaking, do not start without a serious reason. Increased blood clotting is no less dangerous than decreased blood clotting - it often causes the formation of blood clots and blockage of blood vessels.
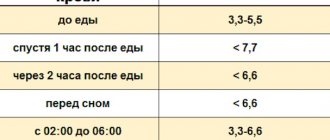
The values of these indicators for children aged 3 to 14 years are almost the same:
- number of platelets in thousands per 1 cubic milliliter of blood – 180-320; in girls in adolescence, at the onset of menstrual bleeding, the platelet count may decrease to 75-220;
- duration of bleeding - can be determined in accordance with different methods: according to Duke, the norm is 2-4 minutes, according to Ivey and Lee-White - less than 8 minutes, according to Sukharev less than 5 minutes;
- clotting time – from 2 to 5 minutes;
- prothrombin time – 11-15 s;
- thrombin time – 15-18 s;
- APTT – within 24-35 s; specific indicators may vary significantly depending on the determination method and the reagents used;
- fibrinogen level – 2-4 g/l;
- antithrombin level - 101-131% - in children from one to 6 years old, 95-134% - in children from 6 to 11 years old, 96-126% - in adolescents under 16 years old.
The importance of these indicators and their role in the blood clotting process should be considered separately.
Laboratory diagnosis of hemostatic system disorders is one of the most expensive in laboratory practice. Performing all possible tests to clarify the nature of the disorders for all patients is an almost impossible task. Therefore, it is extremely important to follow the stages of testing, based on the clinical data and patient’s medical history. At the first stage, to clarify the direction of the disorders, it is necessary to conduct tests that reflect the state of entire parts of the hemostatic system. There is a set of recommended screening tests for diagnosing the state of the hemostatic system:
- APTT (activated partial thromboplastin time)
- Prothrombin time (according to Quick)
- Thrombin time
- Fibrinogen
Blood clotting time (BCT) BCT is an approximate indicator of the state of the multi-stage coagulation cascade, as a result of which soluble fibrinogen passes into insoluble fibrin. This indicator evaluates the coagulation process as a whole and does not make it possible to identify the mechanisms leading to its disruption. A shortened CVV indicates the need to prevent hypercoagulation, which often threatens thrombosis or thromboembolism.
Activated partial thromboplastin time aPTT is used as a screening test to evaluate the intrinsic plasma coagulation cascade, diagnose lupus anticoagulant, and monitor the anticoagulant effect of heparins. APTT is a more significant test for the primary detection of pathology than prothrombin time, as it detects the relatively common hemophilia A and B (deficiency of factors VIII and IX, respectively) and the presence of lupus anticoagulant. The APTT-L+ test has particularly high sensitivity to lupus anticoagulant. In the presence of VA in the blood, the clotting time is extended by 3-3.5 times. The APTT-L test is characterized by high specificity for intrinsic coagulation factors and heparin and low sensitivity to lupus anticoagulant, which makes it possible to differentiate disorders in the intrinsic coagulation cascade even at the stage of their screening.
Prothrombin time (PT) is a widely used screening test to assess the state of the extrinsic and common pathways of the coagulation cascade of plasma coagulation. Normal PT values for adults are 11-15 seconds, for newborns - 13-18 seconds. An increase in PT indicates a tendency to hypocoagulation and may depend on individual reasons:
- Insufficiency of one or more factors of the prothrombin complex, which is observed in such rare hereditary coagulopathies as hypoproconvertinemia (factor VII deficiency) and hypoprothrombinemia (factor II deficiency);
- Deficiency of factor X in amyloidosis (which is absorbed by amyloid) and deficiency of factors V and VII in nephrotic syndrome (which are excreted in the urine);
- Reduced synthesis of prothrombin complex factors in liver diseases;
- Enteropathy and intestinal dysbiosis leading to vitamin K deficiency;
- When treated with vitamin K antagonists;
- For DIC syndrome (consumption of prothrombin complex factors);
- For chronic pancreatitis, pancreatic and bladder cancer;
- Decrease in the level of fibrinogen in the blood (up to 1 g/l and below);
- For acute and chronic leukemia (due to the development of DIC syndrome);
- When the level of antithrombin or antithromboplastin increases;
- Medicines (anabolic steroids, antibiotics, high-dose aspirin, laxatives, methotrexate, niacin, quinidine, quinine, thiazide diuretics, tolbutamide).
A shortened PV indicates a tendency toward hypercoagulation and can be noted in the initial stages of deep vein thrombosis of the lower extremities, with polycythemia, and in the last months of pregnancy.
Monitoring anticoagulant therapy Determination of PT plays a leading role in monitoring therapy with indirect anticoagulants. Research results are traditionally expressed in seconds. When determining PT, a blood clotting activator, thromboplastin, is used. If a laboratory(s) uses one thromboplastin today and another tomorrow, the patient’s PT will differ from day to day. In order to exclude the influence of thromboplastin on the results of determining PT, an indicator is used - the international normalized ratio of INR, which provides the ability to compare the results obtained in different laboratories and guarantees more accurate control of treatment with indirect anticoagulants. INR is calculated using the formula:
Patient INR = [patient PT (sec)/control PT (sec)]international sensitivity index
The main objective of monitoring with indirect anticoagulants is to prevent bleeding. The dose of the anticoagulant should be adjusted to maintain the INR at the required level, depending on the reason for treatment. In most patients, the INR should be maintained at 2-3.0. INR monitoring should be carried out every 2-3 weeks.
To monitor the level of anticoagulants, WHO has developed the following recommendations:
| Clinical condition | Recommended INR |
| Prevention of primary and recurrent deep vein thrombosis and pulmonary thromboembolism | 2,5 (2,0-3,0) |
| Preoperative preparation: surgical interventions in the hip area | 2,0 (2,0-3,0) |
| All other surgical procedures | 2,5 (1,5-2,5) |
| Treatment of deep vein thrombosis, pulmonary thromboembolism and prevention of recurrent venous thrombosis. | 3,0 (2,0-4,0) |
| Prevention of arterial thromboembolism, including in patients with prosthetic valves | 3,5 (3,0-4,5) |
| Recommended levels of hypocoagulation when taking warfarin: high average low | 2,5 — 3,0 2,0 — 3,0 1,6 — 2,0 |
Thrombin time (TT) is the third most important basic screening test. The test characterizes the final stage of the coagulation process - the conversion of fibrinogen into fibrin under the influence of thrombin; it is influenced by the concentration of fibrinogen in plasma and the presence of fibrin degradation products (FDP).
Quantitative determination of fibrinogen using the Clauss method is the basic test for studying hemostasis. Fibrin formation and stabilization is the final step in thrombus formation, in which soluble fibrinogen is converted to insoluble fibrin by the action of thrombin and factor XIII. With atherosclerosis, there is a steady increase in fibrinogen levels, which is difficult to correct with medications. As a result, the risk of cardiovascular diseases increases with increasing initial fibrinogen content in the range of 3.0-4.5 g/l. It was found that an increase in the level of fibrinogen in the blood plasma of patients with cardiovascular diseases precedes the development of myocardial infarction and stroke. The correlation between fibrinogen levels and the development of these complications is especially clear in young and middle-aged patients. Fibrinogen levels are the most sensitive test for detecting asymptomatic stages of peripheral arterial vascular disease.
Special tests for assessing plasma hemostasis
Factor VIII is synthesized in the liver, spleen, endothelial cells, leukocytes, and kidneys and takes part in the first phase (prothrombinase formation) of plasma hemostasis. Determination of factor VIII plays a critical role in the diagnosis of hemophilia A. The development of hemophilia A is caused by a congenital deficiency of factor VIII. At the same time, there is no factor VIII in the blood of patients (hemophilia A) or it is in a functionally inferior form, which cannot take part in blood coagulation (hemophilia A+). Hemophilia A occurs in 90-92% of patients, and hemophilia A+ occurs in 8-10%. In patients with hemophilia, the content of F VIII:C in the blood plasma is sharply reduced, and the concentration of VIII-vWF in it is within normal limits. Therefore, the duration of bleeding in hemophilia A is within the normative limits, and in von Willebrand disease it is extended. Hemophilia A is a hereditary disease, but in 20-30% of patients with hemophilia, family history on the part of the mother's relatives does not provide any information. Therefore, determining factor VIII activity has great diagnostic value. Depending on the level of factor VIII activity, the following clinical forms of hemophilia A are divided: extremely severe form (factor VIII activity from 0 to 1%); severe form (factor VIII activity from 1 to 2%); moderate severity (factor VIII activity from 2 to 5%); mild form, or subhemophilia (factor VIII activity from 6 to 24%). About a third of hemophilia A carriers have factor VIII activity levels between 25 and 49%. In patients with mild forms and carriers of hemophilia A, clinical manifestations of the disease are observed only after injuries and surgical interventions. The minimum hemostatic level of factor VIII activity in the blood for operations is 25%; with a lower level, the risk of developing postoperative bleeding is extremely high. The minimum hemostatic level of factor VIII activity in the blood to stop bleeding is 15-20%; with a lower content, stopping bleeding without administering factor VIII to the patient is impossible. In von Willebrand disease, the minimum hemostatic level of factor VIII activity to stop bleeding and to perform surgery is 25%. In DIC syndrome, starting from stage II, there is a clear decrease in the activity of factor VIII due to consumption coagulopathy. Severe liver disease can lead to a decrease in the level of factor VIII in the blood. The content of factor VIII is reduced in von Willebrand disease, as well as in the presence of specific antibodies to factor VIII. Factor VIII activity increases significantly after splenectomy. In clinical practice, it is very important to differentiate hemophilia from von Willebrand disease.
Coagulogram indicators in hemophilia and von Willebrand disease
| Index | Hemophilia | von Willebrand disease |
| Clotting time | Lengthened | Norm |
| Duration of bleeding | Norm | Lengthened |
| Platelet aggregation with ristocetin | Norm | Reduced |
| Prothrombin time | Norm | Norm |
| APTT | Lengthened | Norm |
| Thrombin time | Norm | Norm |
| Fibrinogen | Norm | Norm |
Factor VII (proconvertin, or convertin) refers to α2-globulins. Congenital deficiency of factor VII causes the development of hemorrhagic diathesis (Alexander disease). Acquired forms of hypoproconvertinemia occur in infants in the first days of life, in patients with liver damage, and also as a result of the action of indirect anticoagulants. There is a decrease in the activity of proconvertin in the blood plasma in patients with viral hepatitis, liver cirrhosis, acute alcoholic hepatitis, and chronic persistent hepatitis. In patients with liver cirrhosis, there is a clear connection between a decrease in proconvertin levels and the severity of the process. Due to its short half-life, decreased activity of proconvertin is the best marker for the development of liver failure. The minimum hemostatic level of factor VII activity in the blood for operations is 10-20%; with a lower level, the risk of developing postoperative bleeding is extremely high. The minimum hemostatic level of factor VII activity in the blood to stop bleeding is 5-10%; with a lower content, stopping bleeding without administering factor VII to the patient is impossible. In DIC syndrome, starting from stage II, the activity of factor VII clearly decreases due to consumption coagulopathy.
Factor XIII (fibrin-stabilizing factor, fibrinase, Lucky-Lorand factor) is a β2-glycoprotein. Congenital factor XIII deficiency is inherited in an autosomal recessive manner, predominantly by males. The first clinical sign of fibrinase deficiency in 80% of patients is prolonged (for days, sometimes weeks) bleeding from the umbilical wound. Bleeding manifests itself in the petechial type. Brain hemorrhages occur. Slow healing of wounds is noted, postoperative hernias often form, and fractures heal poorly. All parameters in the coagulogram, except for the decrease in the level of factor XIII in plasma, remain within normal limits. Acquired deficiency of factor XIII is detected in patients with vitamin C deficiency, radiation sickness, leukemia, cirrhosis, hepatitis, cancer with liver metastases, lymphoma, DIC syndrome, and those who have undergone adrenalectomy; after taking indirect anticoagulants, its activity decreases. The decrease in factor XIII in the blood in these diseases is due to a violation of its synthesis or consumption in the process of DIC syndrome. The activity of factor XIII is recommended to be studied in long-term and poorly healing wounds and fractures, since in some cases such phenomena may be associated with a deficiency of this factor, since factor XIII stimulates the development of fibroblasts. The minimum hemostatic level of factor XIII activity in the blood to stop bleeding is 1-2%; with a lower content, stopping bleeding without administering factor XIII to the patient is impossible. In patients with thromboembolic complications, atherosclerosis, after surgical interventions, in women in labor, after the administration of adrenaline, glucocorticoids, pituitrin, fibrinase activity is often increased.
Factor V resistance to activated protein C. A number of new, recently unknown, but widespread thrombophilias include a condition caused by factor V resistance to activated protein C. Hereditary resistance to activated protein C (RAPS) is the most common cause of primary thrombophilias. Among patients with thrombosis, this pathology occurs in 30-60%, and among a clinically healthy population - in 10-15%. RAPS in 90% of cases is caused by a point mutation in the factor V gene. It causes the replacement of arginine in the factor V molecule with glycine at position 506, the main site of action of activated protein C (APC). The result of this anomaly is low sensitivity, that is, resistance of factor Va (factor V Leiden) to inactivation of its APS. When the procoagulant activity of factor Va is preserved, this leads to the generation of thrombin and a thrombophilic state. Clinically, RAPS is more benign than congenital deficiencies of antithrombin III, protein C, and protein S. The most important clinical risk factors for thrombosis in RAPS include surgery, pregnancy, and the use of oral contraceptives. It has been established that about 30% of postoperative thrombosis is caused by RAPS. During pregnancy, RAPS can manifest itself as thrombosis of placental vessels and intrauterine fetal death. Women who have the Leiden mutation and use oral contraception have a 30-fold increased risk of developing thrombosis. The results of epidemiological studies indicate a frequent combination of RAPS with hereditary or acquired deficiency of protein S or protein C. It is clear that with such combined defects the risk of developing thrombosis increases. It is fundamentally important that the high prevalence of RAPS in the general population dictates the need for laboratory testing of this pathology not only in patients with thrombosis, but also in asymptomatic individuals at high risk of thrombosis. If factor V is resistant to activated protein C, the APS index will be below the lower limit of normal. To confirm the results of functional tests, several polymerase chain reaction-based methods have been developed to diagnose factor Va resistance to activated protein C.
Bleeding time
There are many methods for studying the duration of bleeding, differing in the method of blood sampling and the method of implementation.
Currently, three methods are especially widely used:
- Ivy:
- Duke;
- Sukhareva.
The duration of bleeding according to Ivey is determined as follows: a tonometer is fixed on the patient’s shoulder, with its help a pressure of 40 mm Hg is injected. st, then a small incision is made with a blade on the inside of the forearm. After this, the time is recorded on a stopwatch, and a special filter is applied to the incision every half a minute to absorb blood. When there are no traces of blood left on the filter, the bleeding is considered to have stopped.
This method can only be used with older children and adolescents - it is considered quite aggressive.
The Duke method is more popular and is considered more gentle. To test using this method, you do not need to use a tonometer or make an incision - a small puncture of your finger or earlobe with a special Frank needle is enough. A paper filter is also applied to the puncture site, but not every half a minute, but every 15 seconds. The blood clotting rate in the Duke study does not exceed 4 minutes.
This method is used more widely and is more often used in children.
Sukharev's method is as follows: a blood sample is taken from a finger, then placed in a test tube; The tube is tilted from side to side until the blood sample begins to thicken. The norm from start to finish of coagulation is no more than 5 minutes.
Prothrombin
Prothrombin is a protein that is converted into thrombin during blood clotting; thrombin, in turn, starts the process of converting fibrinogen into fibrin.
When analyzing blood, attention is paid to such an indicator as prothrombin time.
This is the time during which the blood, under the influence of tissue factors, forms a clot.
For children under 14 years of age, this time normally ranges from 11 to 15 s; in infants this figure may be slightly higher - from 14 to 16 s.
An increase in prothrombin time indicates disturbances in the synthesis of prothrombin or fibrinogen.
The reason for this may be:
- liver disease or increased load on the liver as a result of intoxication;
- deficiency of vitamin K, which promotes the production of prothrombin;
- calcium deficiency;
- a decrease in the number of platelets due to allergies, radiation sickness or other disorders;
- anemia;
- hemophilia;
- increased levels of heparin (a protein that prevents blood clotting).
A decrease in prothrombin time can be caused by:
- excess vitamin K;
- increased platelet levels;
- genetic failures that disrupt the production of certain coagulation factors.
Blood clotting according to Sukharev
Blood clotting time (according to Sukharev) is a fairly simple blood test that is taken from a finger prick. The coagulation indicator itself is needed to assess the state of enzymes, but it does not provide information about the mechanisms of its disruption.
In general, the clotting process shows how much the body can protect itself, including from blood loss. Coagulability directly depends on the functioning of the endocrine as well as the nervous system. To determine the state and assess hemostasis (the general coagulation system), a coagulogram is prescribed, as well as blood clotting time (according to Sukharev).
In essence, Sukharev’s method allows you to estimate the interval between blood sampling and the beginning of its thickening, or more precisely, the appearance of fibrin (clot) in it.
Previously, more than thirty methods for determining coagulability were used in medicine; today laboratories use only two, the most reliable and informative ones - according to Sukharev and the Lee-White method. The Sukharev method determines the clotting time of capillary blood only, and the Lee-White method determines only venous blood. This is their difference, but in general both of these methods are quite informative; without them it is impossible to obtain a complete homeostatic picture.
No preparation is required for this analysis, except that the material is collected in the morning and on an empty stomach. Of the liquids, you can only drink water, since all kinds of juices, as well as tea or coffee, can distort the picture of the coagulogram. The procedure itself takes very little time.
How is the research conducted?
The material for the study is a small amount of blood from the patient’s finger. The blood is placed in a special stand, the so-called Panchenkov apparatus. Since the very first drop may contain tissue fluid, only subsequent portions are examined, and the first drop is blotted and wiped off the finger.
The material is collected into a special vessel - a capillary, which tilts in a given rhythm, either left or right at a certain angle. The stopwatch measures the time when the blood stops moving freely inside the vessel, that is, it begins to clot. The normal blood clotting time (according to Sukharev) is: the beginning of fibrin formation is from 30 to 120 seconds, the end of the process is from 3 to 5 minutes.
It should be noted that the results, that is, blood clotting time (according to Sukharev), may vary depending on what medications the person being examined takes. For example, the period from fibrin formation to the end of the coagulation process may be increased due to the use of anticoagulants (warfarin, fraxiparin and others). Liver pathologies or more severe diseases such as hemophilia also increase clotting time.
The blood clotting time (according to Sukharev) can be much lower than normal, as a rule, this happens in women taking oral contraceptives, and this is also possible with large blood loss.
It should be taken into account that clotting may be increased due to the fact that prothrombinase has begun to form in large quantities in the body. All information about the time and speed of blood flow clotting is needed, first of all, by the doctor to clarify the diagnosis and monitor the effectiveness of therapy. In any case, the interpretation of such a complex indicator is the task of a specialist, and not the patient himself.
Thrombin time
Thrombin time is the time it takes fibrinogen to convert to fibrin during the final stages of the coagulation process.
Normally, in children under 14 years of age and adults, the thrombin time is 15-18 s; in infants, this figure may be slightly higher.
An increase in thrombin time may indicate serious disorders, such as:
- liver diseases;
- DIC syndrome (disseminated intravascular coagulation);
- acute leukemia;
- severe intoxication.
However, a relatively harmless lack of vitamin C can also cause an increase in thrombin time.
A decrease in thrombin time can be caused by reasons such as:
- the presence of malignant tumors;
- acute form of an infectious disease (influenza, tuberculosis, pneumonia);
- DIC syndrome in the initial stage.
Thrombin time may also decrease after serious injuries or burns.
Fibrinogen
From all of the above, it can be understood that fibrinogen - the protein from which fibrin is formed - is extremely important for the normal process of blood clotting. The fibrinogen level for children under 14 years of age is from 2 to 4 grams per liter of blood, in infants - from 1.5 to 3 grams per liter.
A decrease in fibrinogen levels can be caused by:
- DIC syndrome;
- serious liver dysfunction; severe intoxication;
- lack of vitamins C and B;
- genetic disorders.
An increase can be caused by:
- acute infectious diseases;
- the presence of malignant tumors;
- diabetes.
Main indicators of coagulogram
The main indicator is the clotting time, the period during which a dense clot is formed that stops bleeding. For a sample from capillaries, this time should be from 30 seconds to 3 minutes, for venous blood - up to 10 minutes.
Prothrombin index
The prothrombin index, or PTI coagulogram, is a comparative study that allows one to determine the deviation in the clotting time of a patient’s sample from that of a healthy person. Normally, the error should be no more than 7%. If the readings are higher, there may be problems with the liver. However, in some cases, for example during pregnancy, the indicator may rise for physiological reasons and not be an indicator of a specific disease. But this does not mean that you should refuse the analysis, it’s just that the norms for pregnant women are slightly different. An INR coagulogram is also performed for those patients who have been taking hormonal medications or contraceptives for a long time.
Fibrinogen concentration level
In order to exclude thyroid disease, acute infection or identify malignant neoplasms, a coagulogram is also performed; fibrinogen in the sample should normally have a concentration of 5.9 to 11.7 µmol/l. If the indicators are significantly higher or lower, you will be immediately referred to a specialized specialist to clarify the diagnosis.
Antithrombin
Antithrombin III is an extremely important protein that regulates the level of blood clotting, preventing its excessive thickening and the formation of blood clots. To assess the general condition of the blood, it is necessary to know the level of antithrombin.
The content of antithrombin in the blood varies greatly depending on age: in infants it is the lowest - 60-90%, in children from one to six years old it reaches a maximum value - 101-131%, then gradually decreases, in adults reaching 66-124% .
An increase in antithrombin levels is observed when:
- acute inflammatory processes in the body;
- acute viral hepatitis;
- lack of vitamin K.
A decrease in antithrombin levels may accompany:
- liver diseases;
- DIC syndrome;
- sepsis;
- congenital disorders of antithrombin synthesis.
Reasons for deviation from the norm
The most common causes of changes in blood clotting parameters are disseminated intravascular coagulation syndrome, hemophilia, intoxication and acute inflammatory processes. These conditions are most often diagnosed based on the results of coagulation tests. However, we should not forget that changes in the composition of the blood can also reflect other pathological processes in the body.
The condition of the blood is influenced by many factors; it somehow “reflects” any violation of the normal state of the body. Therefore, it is necessary to pay attention to any non-standard test results, especially when it comes to the health of the child.
Why is it worth doing a blood clotting test at the State Scientific Research Center of PM?
The reason is simple - we take our work seriously. We have modern high-precision equipment for laboratory research. A staff of qualified and experienced specialists has been recruited.
In addition, if you need a coagulogram, the price of this analysis will be extremely low - we value our visitors and always try to meet them halfway!
Come - we don't have queues or rudeness. We do not lose or confuse tests and can, if necessary, immediately after receiving the results, refer you to a highly qualified doctor.
The page is for informational purposes only. Find out the exact list of services provided and the specifics of the procedures by calling.