There is a standard set of indicators that allows a gastroenterologist or hepatologist to judge the condition of the liver. It includes: enzymes alanine aminotransferase (ALT), aspartate aminotransferase (AST), bilirubin (indirect, direct, total), gamma GT, total protein, alkaline phosphatase (ALP), prothrombin time, prothrombin index and total cholesterol. This set of tests - also called liver tests - is recommended not only for people with pronounced symptoms, but also for those who want to examine the liver prophylactically.
We have already talked about increasing the level of ALT and AST enzymes here. Now let's talk about alkaline phosphatase. What kind of enzyme is this and what can deviations in the amount of ALP indicate? Let's figure it out.
What does alkaline phosphatase show?
The content of the article
Many biochemical processes occur in the human body, including the dephosphorylation reaction. In this case, phosphoric acid is separated from organic ester compounds, participating in calcium-phosphorus metabolism. This process occurs in the presence of the enzyme alkaline phosphatase.
Alkaline phosphatase is an enzyme found in many tissues of the body. But it is mainly concentrated in liver cells, bones, and placenta. The main volume is in the intestinal mucosa.
Alkaline phosphatase is represented in the body by 11 isoenzymes. To determine the cause of elevated alkaline phosphatase, it is also necessary to determine its tissue-specific isoenzymes:
- α2 – liver fraction;
- β1 – bone fraction;
- β2 – intestinal fraction.
Alkaline phosphatase is produced by the upper layer of the intestinal mucosa, but only participates secondarily in the digestive processes. The main function of alkaline phosphatase is dephosphorylation, that is, the separation of phosphoric acid from phosphorus-containing compounds. This enzyme also helps transport phosphorus throughout the body.
The enzyme is called "alkaline" because it is most active in an alkaline environment with a pH ranging from 8.6 to 10.1.
Alkaline phosphatase levels reflect the metabolic efficiency of phosphorus and calcium in the body.
Alkaline phosphatase in children - the norm, reasons for deviation from the norm
Reference values for the alkaline phosphatase test vary with age due to growth.
Normal plasma alkaline phosphatase levels vary by age and gender. Norm for children and adolescents:
| Age | Phosphatase norm |
| Newborns | up to 250 units/d |
| 19 years | up to 350 units/d |
| 10 – 15 years | up to 280 units/l |
| 16 – 19 years old | up to 150 units/l |
Serum levels of this enzyme may vary slightly depending on the testing methods and reagents used.
In pediatric practice, the study of alkaline phosphatase activity plays an important role in the diagnosis of liver diseases, which is complemented by a decrease in the outflow of bile in the duodenum. In addition, the level of alkaline phosphatase in the child's blood is often elevated. High phosphatase levels impair the flow of bile due to bile duct stones or bile duct tumors.
A doctor may make the following diagnoses for a child with elevated alkaline phosphatase:
- bone diseases, including tumors, sarcomas, bone cancer metastases;
- hyperparathyroidism;
- bone damage due to lymphogranulomatosis;
- rickets;
- pediatric diseases - skeletal diseases;
- Infectious mononucleosis;
- myeloma;
- childhood cytomegaly;
- intestinal infections.
The alkaline phosphatase level in children is of great importance in the early diagnosis of rickets. In this case, enzyme activity increases long before the onset of clinical symptoms of the disease.
Sometimes a physiological, that is, natural, increase in the level of alkaline phosphatase in the blood serum occurs: in premature children or adolescents during puberty and intensive bone growth.
Medicines with hepatotoxic side effects may also increase a child's alkaline phosphatase enzyme levels. Such drugs include paracetamol, penicillins, sulfonamides, erythromycin and many others. Increased bone metabolism during bone fracture healing often increases levels of this enzyme.
Decreased alkaline phosphatase enzyme levels are not clinically significant. A decrease in enzyme levels can occur with various bone growth disorders, deficiency of zinc, magnesium, vitamins C and B12 in food, anemia and hypothyroidism, as well as in rare cases of congenital hypophosphatasia.
Alkaline phosphatase in adults - the norm, reasons for deviation from the norm
A test to determine the level of enzyme in the blood is carried out in the following cases:
- routine inspection;
- preparation for surgery;
- performing a set of biochemical tests - liver tests to detect liver diseases;
- diagnosis of bone tissue and bone damage;
- if patients complain of heaviness and pain in the right side under the ribs, nausea, loss of appetite and chronic fatigue.
Norm for women
After the age of sixteen, the amount of alkaline phosphatase begins to decline. But the range of its normal concentration is still quite wide.
With the onset of mature and advanced age, the level of enzymes increases again and should be (units/l):
| Woman's age | Phosphatase norm |
| 20-30 years | 85-105 units/l |
| 30-45 years | 95 – 115 units/l |
| 45-55 years | 100 – 125 units/l |
| 55-70 years | 130 – 145 units/l |
| over 70 years old | 165 – 190 units/l |
Norm for men
In adults, the amount of alkaline phosphatase varies slightly depending on gender; for men the norm is 20-25 units/l higher than for women of the same age:
| Man's age | Phosphatase norm |
| 20 – 30 years | 100-115 units/l |
| 30 – 45 years | 135 – 145 units/l |
| 45 – 55 years | 135 – 150 units/l |
| 55 – 70 years | 135 – 160 units/l |
| over 70 years old | 145 – 190 units/l |
How to prepare for research
No special preparation is required for donating blood for alkaline phosphatase. But it will not be superfluous to remember the precautions that must be observed when taking any blood test.
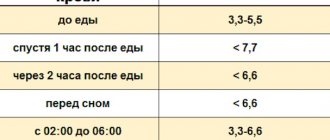
The most important thing is that blood is donated only on an empty stomach. This means that the last meal should be no later than 4 hours before the test. The result will be most reliable if you maintain an 8-hour interval. Dinner on the eve of the study should be light and not plentiful.
Quitting alcohol at least a day before the planned blood donation will prevent falsely inflated test results. The same goes for smoking. Nicotine causes an unjustified and inexplicable increase in the concentration of the enzyme in the blood.
Before taking the exam, it is better not to be nervous and avoid stress. If you have performed physical activity before, it is recommended to rest for at least 5 minutes. Neglecting this advice can also cause distorted results and their interpretation.
Abnormal alkaline phosphatase - causes
The causes of increased alkaline phosphatase levels can be grouped as follows:
- Damage or destruction (destruction) of the liver, problems with the movement of bile:
- viral and autoimmune hepatitis;
- liver pathology caused by toxins and drugs;
- formation of bile in the ducts of stones;
- primary sclerosing cholangitis - manifested by inflammation and narrowing of the intrahepatic ducts;
- Infectious mononucleosis;
- stagnation of bile – cholestasis.
- Pathology of bone tissue:
- osteomalacia or softening of the bones - this systemic damage is characterized by a violation of mineral metabolism and loss of calcium salts, vitamins and phosphoric acid, as a result of which the bones soften and become deformed;
- increased metabolism in bone tissue that occurs during fracture healing;
- Paget's disease - characterized by significant destruction of bone tissue, deformation and weakening of bones, most often affecting men over 50 years of age;
- osteosarcoma and metastases penetrating into bone tissue.
III. Other pathologies:
- primary and secondary hyperparathyroidism are diseases of the endocrine system with severe disturbances in the metabolism of phosphorus and calcium;
- myocardial infarction;
- gastrointestinal pathology.
- Non-pathological reasons:
- alcohol poisoning;
- third trimester of pregnancy;
- lactation;
- the use of drugs with hepatotoxic effects - they can negatively affect the liver and cause structural and functional disorders;
- excessive physical activity;
- poor nutrition and vitamin deficiency;
- possible deviations during childbirth and after menopause vary from person to person.
Exceeding the enzyme norm does not always indicate the type of disease. Perhaps the person is healthy and the increase in alkaline phosphatase is due to physiological properties. Therefore, further tests need to be carried out to determine the exact causes.
Vasilenko V.V. Interpretation of liver tests / GastroScan.ru, 2021
| Authors: Vasilenko V.V. |
Interpretation of liver tests
V.V.
Vasilenko, Candidate of Medical Sciences Reading this text requires some medical training
.
The development of normal boundaries for any biochemical indicator by definition implies that 2.5% of healthy people will not fit into the conventionally normal range. The more tests are used simultaneously, the more deviations we get. In all cases, it is necessary to evaluate the fact, that is, to conclude whether this deviation is clinically significant or insignificant. Naturally, this can only be done taking into account the entire individual clinical context. Recently, this assessment is supposed to be stated in the medical document; This has long been accepted as a rule in clinical drug trials.
With regard to liver tests specifically, it is known that elevated values are more common, namely in 5% of people who do not have symptoms of liver pathology. Factors such as age, gender, blood type, etc. play a role; physiological conditions, such as pregnancy. We also note that Gilbert's syndrome (benign hyperbilirubinemia) occurs in 5% of the population.
The greatest difficulties arise in asymptomatic, or rather low-symptomatic, patients. The tests are classified in Table 1.
Table 1.
Diagnostic minimum biochemical liver tests
| Liver test | Clinical significance of deviations |
| Alanine aminotransferase, ALT (≤45) | ↑ — Damage to hepatocytes |
| Aspartate aminotransferase, AST (≤35) | ↑ — Damage to hepatocytes |
| Bilirubin (2-17) | ↑ - Cholestasis, biliary obstruction or conjugation disorder |
| Alkaline phosphatase, alkaline phosphatase (the rate depends on the method) | ↑ — Cholestasis, biliary obstruction or infiltrative process |
| 5'-Nucleotidase, 5-HT (rate depends on the method) | ↑ — Cholestasis or biliary obstruction |
| γ - Glutamyltransferase, GGTP (≤ 30) | ↑ — Cholestasis or biliary obstruction |
| Lactate dehydrogenase, LDH (≤ 450) | ↑ — Damage to hepatocytes, nonspecific to liver diseases |
| Albumin (40-60) | ↓ — Decreased synthetic function |
| Prothrombin time (PT): 10.9-12.5 sec (and INR) | ↑ — Decreased synthetic function |
If a laboratory error is suspected, the modified test is usually repeated. However, obtaining a normal result does not exclude that the previous deviation was true; it may reflect natural fluctuations in the disease. For example, with hepatitis C, ALT may become normal, but this does not correlate with tissue changes. A normal result, unfortunately, does not exclude liver disease. It is also necessary to take into account the fact that the sensitivity and specificity of determining enzyme activity is limited.
LDH is found in the heart and skeletal muscles, liver, lungs, and blood cells. In the liver - LDH5 isoenzyme.
The liver synthesizes 10-12 g of albumin per day. An albumin content of less than 30 g/l indicates chronic liver disease.
PT reflects the rate of conversion of prothrombin to thrombin. It is associated with factors I, II, V, VII, X of blood coagulation, with the levels of fibrinogen and prothrombin. All factors except VIII are synthesized in the liver.
The half-life of serum albumin is 20 days, and that of coagulation factors is less than 24 hours. If hypoalbuminemia reflects chronicity, then an increase in prothrombin time may serve as a marker of the severity of acute liver dysfunction. For example, in acute viral hepatitis, an increase in PT by 5-6 seconds indicates the possibility of fulminant necrosis. Its detection is possible due to the short half-life of (key) coagulation factor VII.
BILIRUBIN
Bilirubin is formed from heme in the reticuloendothelial system.
Fractions of direct and indirect bilirubin have been determined since the 20s of the last century. But only in the 60s it was stated that indirect B corresponds to its unconjugated form, and direct B is a combination of mono- and diglucuronides B, i.e. bound B). The terms “direct/indirect” are being used less and less. The content of unconjugated B in serum reflects the balance between its production and hepatobiliary excretion. Unconjugated HD is not dangerous in itself, but increases the risk of pigmented gallstones.
Conjugated HD reflects liver parenchymal disease or biliary obstruction. With conjugated HD, significant amounts of B enter the urine. Cholestasis can be extra- and intrahepatic, while headache can occur without simultaneous deviations in enzyme activity.
Fluctuations in bilirubin from day to day are 15-30%; the figure increases by 1.5-2 times after prolonged fasting, decreases by 15% when taking birth control pills, decreases by 33% in the second trimester of pregnancy, increases by 50% after physical activity in men; laboratory errors - blood hemolysis - changes the indicators; keeping a blood sample in the light for an hour reduces the indicator by 50%.
Table 2.
Main causes of hyperbilirubinemia (HB)
| Unconjugated (indirect) GB: |
| Gilbert's syndrome Ineffective erythropoiesis (B12 deficiency, etc.) Hemolysis (including during blood transfusion) Resorption of extensive hematoma |
| Conjugated (direct) GB: |
| Biliary obstruction Hepatitis Cirrhosis Drugs/toxins Primary biliary cirrhosis Primary sclerosing cholangitis Intrahepatic cholestasis of pregnancy Benign recurrent cholestasis |
AMINOTRANSFERASES
Aminotransferases are enzymes of gluconeogenesis.
AST (AST) has cytosolic and mitochondrial isoenzymes. ALT (AlAT) is a cytosolic enzyme. The enzymes AST and ALT have been used in the diagnosis of liver diseases since 1955. They are found in the cells of various tissues, with the highest activity of AST in the liver, heart and skeletal muscles, and kidneys. ALT is found primarily in the cytoplasm of liver cells and, to a lesser extent, in muscle cells. Consequently, an increase in m.b. for endocarditis, heart attack, musculoskeletal injuries. The greatest increase is observed with any hepatitis, including ischemic. The degree is proportional to the severity of acute liver damage. Individuals with an increase in ALT and AST higher than 1.5 and no more than 5 times are considered as a separate category. This is the most current group. Chronic elevation of ALT or AST is conventionally considered to be the persistence of deviations for six months. Liver damage does not necessarily mean necrosis; it may be a reversible condition in the form of increased permeability of cell membranes. A simultaneous increase in ALT and AST usually excludes a laboratory error and indicates a hepatic origin.
Alcoholic liver damage is characterized by an AST/ALT ratio of 2:1 or more + a double increase in GGTP levels. A sharp increase in enzymes rarely occurs in chronic ALD. This occurs when viral hepatitis is attached or paracetamol is taken. Higher transferases are observed in ischemic hepatitis and other conditions listed in Table 3, including sometimes choledocholithiasis.
Table 3.
Main causes of moderate hypertransaminasemia (<5 times)
| HEPATIC: | EXTRAHEPATIC: |
| with a predominance of ALT elevation: | Hemolysis |
| Chronic hepatitis B, C | Myopathies (including from statins) |
| Acute viral hepatitis (A-E, EBV, CMV) | CHF and ischemic hepatitis |
| Steatosis/steatohepatitis | Hypothyroidism |
| Hemochromatosis | Excessive physical load |
| Medicines/toxins | Macro-AST syndrome (rare) |
| Autoimmune hepatitis | |
| α1-antitrypsin deficiency | |
| Wilson's disease | |
| with a predominance of AST rise: | |
| Alcohol liver damage | |
| Steatosis/steatohepatitis | |
| Cirrhosis |
A common serious cause is hepatitis C, hepatitis B will now be less common (vaccination results). In the United States, approximately 4 million people are infected with the hepatitis C virus, and we probably have about the same number. Antibodies to the hepatitis C virus are not protective; they clearly indicate the presence of infection, but appear much later than infection. It must be taken into account that HbsAg becomes positive only 2-8 weeks after the change in liver tests.
A relatively new cause is fatty infiltration of the liver with or without inflammation (steatohepatitis and hepatosis). This diagnosis-cause for chronic enzyme shifts usually has to be made by exclusion. In nonalcoholic steatosis, the AST/ALT ratio is usually less than 1:1, and bilirubin and albumin are normal.
Hereditary hemochromatosis (HC) is one of the most common genetic diseases with varying clinical severity. May initially manifest itself as a rise in transaminases. There is a family history of abdominal pain, arthralgia, impotence, general weakness and fatigue. There are also non-hereditary forms of HC.
Autoimmune hepatitis, Wilson's disease, and α-1-antitrypsin deficiency each occur with a population incidence of approximately 1:6000. In CAH, more than 80% of patients have hypergammaglobulinemia on electrophoresis. There are three types of CAH.
ALT: fluctuations from day to day are 10-30%, during the day - up to 45% (the highest result during the day), physical activity reduces the indicator by 20%. AST: fluctuations from day to day are 5-10%, good physical activity increases the rate almost three times. The activity of both enzymes - ALT, AST - is not affected by food intake; both indicators increase by 4-50% with obesity.
NEW MEDICINES - OLD DANGERS
Most people with isolated mild elevations of ALT do not have liver disease.
If a drug is suspected as the cause, it can be replaced with another drug. It is important to understand which drugs damage the liver and which drugs cause an increase in transaminases to have extrahepatic causes, because you have to decide whether it is advisable to discontinue the drug or continue therapy. The most relevant situations right now are those related to taking statins. Also, ¾ of those receiving anticonvulsant therapy have abnormal liver tests. Conditionally unfavorable liver reactions to drugs are divided into: abnormal tests - when the indicator of one of the enzymes does not exceed two norms, and liver damage - when one of the indicators (not only transaminases) is two times or more higher than the upper limit of normal. The risk of drug-induced liver injury is higher with polypharmacy, especially in old age. Functional liver disorders usually disappear 4-6 weeks after drug withdrawal. The concept of hepatotoxicity includes true drug-related toxicity, dose-dependent toxicity (paracetamol), and idiosyncrasy. The second is a consequence of individual predisposition. Much more often we deal with milder conditions caused by idiosyncrasy. More than 50 microsomal isoenzymes are known in the hepatic cytochrome P450 detoxification system, the structure of which is encoded by individual genes. Genetic differences in the catalytic activity of enzymes explain the reason for the development of idiosyncratic reactions to individual drugs. But an excessive increase in the activity of enzymes of the cytochrome P-450 system as a result of their induction (for example, against the background of alcohol intoxication) can be accompanied by a sharp increase in the production of toxic metabolites.
Dopegit, Nicotinic acid, Ketoconazole and Fluconazole provoke acute drug-induced hepatitis.
Paracetamol - necrosis of hepatocytes in the pericentral zone of the hepatic lobule.
Diclofenac, Finlepsin, Propylthiouracil - liver damage as a hypersensitivity reaction. The reaction usually develops after 2-4 weeks of treatment, especially when the “culprit” drug is re-prescribed. Clinically, there is a wide variability of manifestations: from isolated acute hepatitis of moderate activity to active hepatitis with systemic lesions. Of the NSAIDs known to us, diclofenac is significantly more likely to cause serious liver disorders compared to placebo. When a reaction develops according to the hypersensitivity mechanism, when the drug acts as a hapten, symptoms may persist even many months after drug withdrawal.
Amiodarone - development of drug-induced steatohepatitis. It inhibits the oxidation of fatty acids in mitochondria and disrupts the process of electron transfer in the respiratory chain, which promotes the activation of lipid peroxidation. The catabolism of phospholipids in lysosomes is also suppressed, which leads to the development of phospholipidosis.
Depakine - liver damage of the mitochondrial cytopathy type. The mechanism of this type of lesion is due to the blockade of enzymes of the mitochondrial respiratory chain, direct inhibition of enzymes by the metabolite of valproate (2-propylpentanoic acid).
Amoxicillin, Maninil, Sulfonamides - parenchymal-tubular cholestasis. Immune mechanisms appear to predominate in the pathogenesis of the disorder.
The first step in treatment should be discontinuation of the drug. In most cases, drug information relatively quickly leads to a significant improvement in clinical and laboratory data. But it should be borne in mind that it is necessary to continue long-term observation of patients, especially those who received drugs with a long half-life (for example, amiodarone).
Table 4.
Medicines, maybe cause of hypertransaminasemia
| Methyldopa (Aldomet, Dopegyt) |
| Nicotinic acid in high doses |
| Ketoconazole (Nizoral) |
| Fluconazole (Diflucan) |
| Paracetamol in high doses |
| Diclofenac |
| Carbamazepine (Finlepsin) |
| Propylthiouracil |
| Amiodarone (Cordarone) |
| Valproic acid (Konvulex, Depakin) |
| Amoxicillin + clavulanic acid (Amoxiclav) |
| Glibenclamide (Maninil) |
| Sulfonamides |
| Heparin |
| Zafirlukast (Akolat) |
| Proteinase inhibitors (Gordox, Contrical) |
| Statins |
| Phenylbutazone (Butadione) |
ALKALINE PHOSPHATASE
ALP belongs to the family of zinc-containing metalloenzymes.
Contained mainly in the liver and bones, 20% is in the intestinal wall. ALP increases when there is metabolic stimulation in the corresponding tissues. Thus, in adolescents it increases 2 times compared to the adult norm due to the bone isoenzyme. During pregnancy, in the first trimester it can increase twofold due to placental isoenzymes and more significantly in the prenatal period. The half-life of ALP is a week, so it begins to rise 1-2 days after the onset of biliary obstruction and remains elevated for several days after its resolution.
Isolated increase in alkaline phosphatase may. the only anomaly in primary biliary cirrhosis and other cholestatic diseases. An increase in alkaline phosphatase with normal or slightly elevated levels of other indicators may also indicate an infiltrative (tumor) process.
Every time you have to deal with alkaline phosphatase - whether it is of hepatic or bone origin. It is also known that ALP can increase in cancers without damage to the liver or bones due to one isoenzyme, which is now called the (President) Reagan isoenzyme. Fractional determination of alkaline phosphatase isoenzymes allows us to determine the source of the increase in its activity. A more specific test than ALP is the determination of 5′-nucleotidase, also from the phosphatase family; it is significantly increased only in liver diseases with cholestasis. It is also found in other organs, but not in bones. Another way to evaluate a source is to determine the GGTP.
Fluctuations in ALP levels from day to day are 5-10%; the figure increases 2-3 times in the third trimester of pregnancy, decreases by 20% when taking birth control pills, 10% higher in smokers, 25% higher in obesity; physical activity has no noticeable effect; food intake changes the indicator in individuals with a certain blood type.
Table 5.
Causes of elevation of alkaline phosphatase
| Hepatic |
| Biliary obstruction |
| Primary biliary cirrhosis |
| Medicines |
| Infiltrative liver diseases |
| Liver metastases |
| Hepatitis |
| Cirrhosis |
| Dysfunction of the biliary sphincters |
| Benign recurrent cholestasis |
| Extrahepatic |
| Infection/inflammation |
| Bone diseases |
| Congestive heart failure |
| CRF (chronic renal failure) |
| Lymphoma and other malignancies. processes |
| Growth spurt in teenagers |
| Pregnancy (III trimester) |
GAMMAGLUTAMYLTRANSPEPTIDASE
This enzyme is localized on the canalicular membrane of the hepatocyte, facing the bile capillary.
GGTP is also found in the kidneys, pancreas, intestines and, to a lesser extent, heart muscle. This enzyme is absent in bones. Thus, the rise in GGTP confirms the hepatic genesis of the rise in alkaline phosphatase. In general, GGTP increases in many situations, for example in alcoholics. An isolated increase in GGTP can also be observed after episodic alcohol intake during anticonvulsant therapy or taking warfarin. By the way, adding diclofenac to warfarin increases the risk of gastric bleeding by 3-6 times.
Table 6.
Reasons for increasing GGTP
| Hepatobiliary diseases (usually simultaneous with abnormalities of other enzymes) |
| Pancreatic diseases |
| Alcohol intoxication |
| COPD (chronic obstructive pulmonary disease, chronic obstructive bronchitis) |
| Diabetes |
| Acute myocardial infarction |
| Medicines (eg anticonvulsants) |
Amoxiclav, Chlorpropamide, Peritol can provoke parenchymal-tubular cholestasis.
Diltiazem, Biseptol - drug-induced steatohepatitis.
Estrogens - steatohepatitis and tubular cholestasis. The development of cholestasis is caused by suppression of bile transport, independent of bile acids.
Antiviral drugs - liver damage due to mitochondrial cytopathy.
Finlepsin, Quinidine - liver damage as a hypersensitivity reaction.
Captopril is an acute drug-induced hepatitis.
Table 7.
Medicines that can cause a rise in bilirubin or alkaline phosphatase
| Amoxiclav |
| Chlorpropamide |
| Cyproheptadine (Peritol) |
| Diltiazem |
| Co-sulfamethoxazole (Biseptol) |
| Estrogens |
| Antiviral (Viramun, Krixivan) |
| Carbamazepine (Finlepsin) |
| Quinidine |
| Captopril (Capoten) |
| Allopurinol |
| Imipramine (Melipramine) |
| Erythromycin |
* * *
In a country where they count money, they give the following assessment of current situations. Repeating the transaminase analysis costs $30, a regular clinical diagnostic examination (serology of viral hepatitis, serum iron, etc.) costs $350, and an extended one, including additional serology and liver biopsy, costs $3000. That is, a timely conclusion from a certified specialist information about the patient’s health can save you a couple of thousand dollars.
V.V. Vasilenko. Sixty essays on digestion (recommendations from a gastroenterologist to patients) Back to section
Alkaline phosphatase levels are below normal
A decrease in enzyme content can signal the appearance or presence of dangerous diseases in the body.
Reasons for decreased enzyme levels:
- severe anemia;
- hypothyroidism – decreased levels of thyroid hormones;
- significant blood transfusions;
- fetal malformations, for example, placental insufficiency - a common complication of pregnancy;
- frequent use of oral contraceptives;
- hypophosphatasia is a rare but life-threatening disease;
- radioactive contamination - in this case, measuring blood parameters will show the accumulation of radioactive isotopes;
- malnutrition, lack of magnesium, zinc and vitamin C;
- Excess vitamin D can cause a change in the reagent when diagnosing certain diseases, for example, rickets.
When is a blood test for alkaline phosphatase performed?
In clinical practice, alkaline phosphatase levels acquire important diagnostic value only in combination with other laboratory and instrumental studies. Therefore, patients are usually given a biochemical blood test, which includes alkaline phosphatase.
This study is indicated for all outpatient and inpatient patients with impaired liver, kidney, digestive and endocrine system function. Currently, in most cases they are limited to determining the total level of alkaline phosphatase, since fractional analysis, although more informative, is very expensive and is carried out only in specialized laboratories.
Complications without treatment
Changes in the biochemical blood test themselves do not pose a threat to human life. Diseases that cause an increase or decrease in alkaline phosphatase are dangerous.
Bone tumors can be aggressive. Early detection and initiation of specific treatment minimizes early disability and mortality in these cases and provides a chance for a high five-year survival rate. Identification of the primary site within metastasis also allows timely initiation of therapy and achievement of a favorable prognosis.
Hepatitis is dangerous and can lead to cirrhosis. This applies to viral hepatitis C, which goes unnoticed for a long time.
Cirrhosis is complicated by loss of liver function, development of bleeding, decreased protein levels, and failure of heart function.
Bone tumors are dangerous due to skeletal deformation. If metastases occur, complications depend on their location. Foci in the brain and liver are especially dangerous.
Alkaline phosphatase is not a specific marker for any disease. But this indicator indicates to specialists in which direction to look for pathology. It is important to understand that the norms differ for men and women of different ages. An additional examination is ordered to find the cause. As a result, the causative factor is identified and its specific treatment begins.
Article design: Vladimir the Great
How is the alkaline phosphatase test performed?
To get the correct test result, you must follow these rules:
- the test may be performed in a laboratory, from which a healthcare professional takes a blood sample from the bloodstream and places it in a closed container for testing;
- Blood sampling is carried out in the morning from the ulnar vein in the amount of 5-10 ml;
- the test should be performed on an empty stomach and it is best not to eat for at least 12 hours before taking blood;
- the day before donating blood, you should not engage in heavy physical work or sports associated with severe stress;
- Avoid drinking alcohol and drugs that increase alkaline phosphatase levels.
Typically, test results are ready in 1–2 days.
Features of determining alkaline phosphatase
Blood serum is used for analysis. In most cases, the top layer formed in the separator tube is taken. The activity of this enzyme may vary slightly when blood samples are stored at room temperature. Hemolysis in vitro does not affect the test results.
How the biomaterial is collected
In inpatient conditions, a laboratory assistant comes to the department and draws blood in a treatment room. Patients arrive at the clinic at the appointed time in the early morning, where they are collected material for research on a first-come, first-served basis.
The laboratory assistant places up to 15 ml of the patient’s venous blood into a dry, clean test tube. The vein puncture site is treated with an antiseptic swab, which is then disposed of.
What to do if your alkaline phosphatase level is abnormal?
When treating, the etiological direction should be indicated. If you have liver or biliary tract diseases, you should consult a gastroenterologist. The presence of cholestasis, pancreatitis, alcoholic hepatitis or cirrhosis of the liver requires appropriate medical correction, the extent of which is determined only by a doctor. Self-medication in this case can aggravate the underlying disease.
Changes in enzyme levels, including alkaline phosphatase, may occur in heart failure, cancer and serious kidney problems, as well as diabetes, so consult a cardiologist, nephrologist or endocrinologist. The doctor determines treatment tactics depending on the clinical picture.
By eliminating etiological factors, alkaline phosphatase activity is normalized. When prescribing therapy, it should be taken into account that, for example, a physiological increase in this indicator is possible with fractures, active skeletal growth and pregnancy. This does not require medical intervention. Interpretation of laboratory test results should be carried out comprehensively, taking into account other biochemical indicators and patient complaints.