Lactate dehydrogenase (LDH) is an intracellular enzyme involved in glucose metabolism. Contains zinc and is produced by all cells of the body.
The greatest activity of the enzyme is observed in muscles, heart, liver, kidneys and blood cells - red blood cells.
There are 5 types of LDH; the predominance of one or another type of enzyme determines the method of glucose metabolism in tissues - aerobic (to carbon dioxide and water) or anaerobic (to lactic acid). For example, LDH-1 predominates in the myocardium, LDH-2 predominates in the kidneys and blood cells, LDH-3 and 4 predominate in most internal organs, and LDH-5 predominates in muscles, placenta, and liver. All forms of the enzyme are present in the blood, where they are determined as part of the total indicator - total lactate dehydrogenase.
The concentration of LDH in the blood increases in diseases characterized by damage to body tissues. A blood test for LDH is not specific, but in combination with other tests it helps to diagnose various pathological conditions: pulmonary infarction, hemolytic anemia, etc. When diagnosing myocardial infarction, the analysis is used as an auxiliary test in the case of pain in the chest. In the presence of a heart attack, LDH activity increases, while during angina attacks the indicator does not change. The level of LDH in the blood can increase even in the presence of malignant tumors and decreases with their effective treatment, which allows the test to be used for dynamic monitoring of cancer patients.
Distribution of fractions in plasma. Age and norm
content of LDH fractions in organs
The first fraction (LDH-1 or HHNN tetramer) originates primarily in the cardiac muscle and is significantly increased in the blood serum with myocardial damage.
The second, third, fourth fractions (LDG-2, LDH-3, LDH-4) begin to actively enter the plasma under pathological conditions accompanied by massive death of blood platelets - platelets, which occurs, for example, in the case of such a life-threatening condition as pulmonary embolism (PE).
The fifth isoenzyme (LDG-5 or MMMM tetramer) comes from the cells of the liver parenchyma and is released into the blood plasma in large quantities at the acute stage of viral hepatitis.
Due to the fact that different types of tissue accumulate and release different concentrations of LDH, fractions of lactate dehydrogenase isoenzymes are distributed unevenly in the blood plasma:
| Isoenzyme | Serum concentration |
| LDH-1 | 17 – 27% (0.17 – 0.27 relative units) |
| LDG-2 | 27 – 37% (0,27 – 0,37) |
| LDG-3 | 18 – 25% (0,18 – 0,25) |
| LDG-4 | 3 – 8% (0,03 – 0,08) |
| LDG-5 | 0 – 5% (0,00 – 0,05) |
The activity of lactate dehydrogenase in red blood cells (erythrocytes) is 100 times higher than the levels of the enzyme contained in the blood plasma, and increased values are observed not only in pathological conditions, but also in a number of physiological conditions, for example, pregnancy, the first months of life or excessive physical effort on their part also contribute to an increase in LDH activity. Significant differences in the normal levels of this indicator are also due to age and gender, as evidenced by the table below:
| Age | Normal indicators (U/l, 37°C) |
| Newborns | 150 — 785 |
| From 1 month to six months | 160 — 437 |
| From 7 months to a year of life | 145 — 365 |
| From 1 year to 2 years | 86 -305 |
| From 3 to 16 years | 100 — 290 |
| Adult Women Men | 120 – 214 135 — 240 |
Meanwhile, the normal values for blood LDH are always approximate; they should not be memorized once and for all for the reason that the analysis can be performed at a temperature of 30°C or 37°C, the level is calculated in different units (μkat/l, mmol/( h·l), U/l or U/l). But if there is an urgent need to independently compare your own results with the normal variants, then it will be useful to first inquire about the institution that performed the analysis, the methods of its implementation and the units of measurement used by this laboratory.
Excretion of lactate dehydrogenase isoenzymes (LDH-4, LDH-5) by the kidneys does not exceed the level of 35 mg/day (excretion rate).
Reasons for increased LDH
The level of LDH activity is increased in almost any pathological process that is accompanied by inflammation and death of cellular structures, therefore the reasons for the increase in this indicator are primarily considered to be:
- Acute phase of myocardial infarction (a more detailed description of changes in the LDH spectrum during necrotic myocardial damage will be presented below);
- Functional failure of the cardiac and vascular system, as well as the respiratory system (lungs). Involvement of lung tissue in the process and the development of circulatory failure in the pulmonary circulation (LDH levels are increased due to the activity of LDH-3 and, to some extent, due to LDH-4 and LDH-5). Weakening of cardiac activity leads to circulatory disorders, symptoms of congestion and an increase in the activity of LDH-4 and LDH-5 fractions;
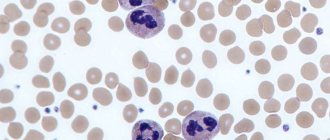
- Damage to red blood cells (pernicious and hemolytic anemia), causing a state of tissue hypoxia;
- Inflammatory processes affecting the lungs, as well as the renal or hepatic parenchyma;
- Pulmonary embolism, pulmonary infarction;
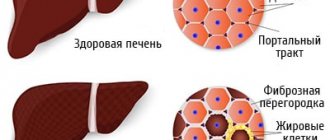
- Acute period of viral hepatitis (in the chronic stage, LDH activity, as a rule, does not leave the normal range);
- Malignant tumors (especially those with metastasis), localized mainly in the liver tissue. Meanwhile, a strict correlation, in contrast to myocardial infarction (the larger the size of the lesion, the higher the activity of LDH) between the progression of the oncological process and changes in the spectrum of lactate dehydrogenase is not traced;
- Various hematological pathologies (polycythemia, acute leukemia, granulocytosis, chronic myeloblastic leukemia, anemia caused by vitamin B12 deficiency or lack of folic acid);
- Massive destruction of platelets, which is often caused by blood transfusions that are not provided with sufficient selection for individual blood systems (for example, HLA);
- Diseases of the musculoskeletal system, primarily damage to skeletal muscles (injuries, atrophic lesions, mainly at the initial stage of disease development).
Alkaline phosphatase (ALP)
This is an enzyme that is usually localized in the membrane, in contrast to the enzymes described in the first part of the article, which are located in the cytoplasm of cells.
It is mainly contained in the brush border of the mucous membrane of the bile canaliculi (the surface layer of cells forms brush-like outgrowths, hence the name). This is a key enzyme involved in the metabolism of phosphoric acid. Most often, alkaline phosphatase is determined when gallstone disease is suspected and the mechanical origin of jaundice occurs when stones block the lumen of the ducts, bile stagnates, and the pigment bilirubin begins to leak into the blood. The diagnostic value is based on the fact that during obturation the activity of alkaline phosphatase increases 10 times. ALP is often determined by monitoring the healing of bone tissue and the healing of fractures, as well as when tumor processes in the bone are suspected, since the enzyme functions as a marker of osteosynthesis. Norm:
30-90 units/l.
Increase:
with obstructive jaundice, bone tumors and metastases, rickets, to a lesser extent with destructive liver diseases (cirrhosis, cancer), amyloidosis, blood diseases (myeloma, lymphogranulomatosis, mononucleosis), hyperthyroidism.
Decrease:
observed with a lack of certain microelements (zinc, magnesium, vitamins B12 or C), as well as with anemia, placental insufficiency during pregnancy, hyperthyroidism and disorders of growth and bone formation.
LDH and cardiac muscle necrosis
The study of the glycolytic enzyme has a very important diagnostic value in case of damage to the heart muscle, therefore it is one of the main enzymatic tests that determine myocardial infarction on the first day
development of a dangerous necrotic process localized in the heart muscle (8–12 hours from the onset of pain). The increase in enzyme activity occurs, first of all, due to the LDH-1 fraction and partly due to the second fraction (LDH-2).
After a day or two from a painful attack, the level of LDH in the blood reaches its maximum values and in most cases remains highly active for up to 10 days. It should be noted that activity is directly dependent on the area of myocardial damage
(the larger the size of the lesion, the higher the indicator values). Thus, myocardial infarction, initially diagnosed using laboratory tests such as determination of creatine kinase and the MB fraction of creatine kinase, can be confirmed within a day by this enzymatic test (LDG is elevated and increased significantly - 3 - 4 ... up to 10 times).
In addition to increasing the total activity of lactate dehydrogenase and increasing the activity of the LDH-1 fraction, the LDH/LDH-1 or HBDG (hydroxybutyrate dehydrogenase) ratio and the LDH-1/LDH-2 ratio are of particular value for detecting acute myocardial infarction. Considering that the GBDG values in the acute period of the disease change significantly upward, and the total activity of lactate dehydrogenase will be reduced relative to the rather high LDH-1 values, the LDH/GBDG ratio will noticeably drop and will be below 1.30. At the same time, the LDH-1/LDG-2 ratio, on the contrary, will tend to increase, tending to reach 1.00 (and sometimes even cross this line).
LDH, Lactate dehydrogenase
Lactate dehydrogenase is an intracellular glycolytic zinc-containing enzyme that accelerates the final conversion of glucose.
LDH is localized in the cytoplasm of cells and is contained in almost all tissues and organs of the human body. The highest concentration of LDH is in the liver, kidneys, heart, pancreas, skeletal muscles, and blood cells (erythrocytes contain 100 times more LDH than blood serum). The level of the enzyme in a child’s body is higher than in an adult’s (the enzyme exhibits especially high activity in the body of newborn children). As children grow and mature, LDH levels gradually decrease. The concentration of lactate dehydrogenase in the female body is slightly lower than in the male body.
LDH is not a homogeneous enzyme. It is divided into five isoenzymes that have different molecular structures and are localized in different tissues and organs. A representative of any of them consists of a combination of four peptide chains - M and H. Under the influence of an electric field, the isoenzymes move at different speeds. The gradation from fast to slower movement looks like this: LDH-1, LDH-2, LDH-3, LDH-4, LDH-5.
The predominant isoform of the enzyme “dictates” the main way in which glucose will be oxidized. There are two options:
- aerobic (with the presence of oxygen), with oxidation to carbon dioxide and water;
- anaerobic (without oxygen), with oxidation to lactic acid.
This difference is due to the fact that each of the LDH isoforms has a characteristic degree of affinity with pyruvic acid.
The largest amounts of LDH-1 are found in the heart muscle, red blood cells, platelets and the renal cortex (the molecule consists of 4 identical H units).
Red blood cells, platelets, and kidneys also contain a significant amount of LDH-2.
Of the 5 isoenzymes, the predominant concentrations of LDH-3 and LDH-4 are characterized by the lungs, pancreas and thyroid gland, spleen, lymphocytes, and adrenal glands.
In addition, LDH-4 is contained in granulocytes, the placenta, male germ cells and, to a lesser extent, the liver.
The LDH-5 isoform (MMMM chain) is contained in skeletal muscles (it also contains LDH-4 and LDH-3, but their activity is lower than LDH-5) and the liver.
Normally, blood serum contains a small amount of LDH isoenzymes, which come there from renewing cells. The concentration of total LDH studied in this test is determined as the sum of the concentrations of all five isoenzymes. As the activity of LDH isoforms decreases, it is determined as follows: LDH-2 > LDH-1 > LDH-3 > LDH-4 > LDH-5.
Tissue damage results in the release of excess LDH into the serum, and therefore this test is used to determine the presence of tissue damage. The indicator is not specific - it cannot accurately determine the disease, however, in combination with other indicators, the test result allows you to diagnose:
- pulmonary infarction;
- muscular dystrophy;
- hemolytic anemia.
Testing LDH concentration is an auxiliary test in the diagnosis of myocardial infarction. Previously, studies of creatine kinase and aspartate aminotransferase (AST) levels were widely used to confirm pathology. However, the level of these enzymes during the process of treatment and restoration of the myocardium returns to normal values twice as quickly as the level of LDH. Therefore, studying the concentration of lactate dehydrogenase makes it possible to track the dynamics of the process at later stages of the disease.
Currently, to confirm the diagnosis of myocardial infarction, troponin testing, which is a more specific indicator of damage to the heart muscle, is more often performed. However, monitoring changes in LDH concentrations also allows one to monitor the progression of the disease. Its level begins to increase 12-24 hours after the onset of a painful attack and reaches peak levels after 24-48 hours. LDH activity remains high up to 10 days. It is directly dependent on the size of the myocardial lesion, and the speed of normalization depends on how quickly the heart muscle recovers. In addition, LDH activity is an identifier of true myocardial infarction and allows it to be distinguished from angina attacks with similar pain symptoms. During angina pectoris, LDH activity does not change, but during infarction, total LDH activity increases significantly.
An increase in the level of lactate dehydrogenase 1-2 days after a painful attack in the chest against the background of normal AST levels is an indicator of pulmonary infarction.
Studying the level of LDH in muscle pathologies allows us to identify the nature of the disease:
- enzyme activity remains normal if the cause of muscle dysfunction is neurogenic (caused by disruptions in the nervous system) diseases;
- the concentration of lactate dehydrogenase increases if muscle damage is caused by dysfunction of the endocrine glands or diseases characterized by metabolic disorders.
The development of malignant tumors can serve as an impetus for increasing the activity of lactate dehydrogenase. If the treatment used is effective, then the level of the enzyme decreases, so this testing can be used to monitor the condition of a cancer patient over time.
The reasons for increased LDH levels can be not only pathological, but also physiological. The latter, in particular, include pregnancy, the neonatal period, excessive physical activity, and the presence of a prosthetic heart valve.
Using different research methods may show different levels of the enzyme. Therefore, when determining an indicator over time, it is advisable to undergo examination in one laboratory.
Other reasons for changing odds
The above parameters, in addition to necrotic damage to the heart muscle, are also subject to changes in the case of other serious diseases:
- Hemolytic anemia of various origins (LDG/GBDG decreases and becomes below 1.3);
- Megaloblastic anemia (the content of the first fraction significantly exceeds the concentration of the second);
- Conditions accompanied by increased cell destruction (acute necrotic process);
- Neoplasms localized in the glands of the female and male reproductive system: ovarian dysgerminoma, testicular seminoma, teratoma (here only an increase in the concentration of LDH-1 is noted);
- Renal parenchyma lesions.
Thus, the main culprits, and therefore the main reasons for changes in the concentration of the described indicators in the blood serum, can be considered conditions associated with the destruction of liver and kidney parenchyma cells, as well as blood cells (platelets, erythrocytes).
Some nuances
To study LDH in the blood, 1 ml of serum is sufficient, which is obtained from blood donated, as for any other biochemical test, in the morning on an empty stomach (however, if there is a question about diagnosing acute MI, then these rules, of course, are neglected).
In a laboratory study of LDH, hemolysis leads to distortion of the analysis results (overestimates them). And when exposed to heparin and oxalate, the enzyme activity in the serum, on the contrary, will be reduced compared to the real blood LDH values. To prevent this from happening, you should start working with the material as early as possible, first of all separating the clot with formed elements from the serum.
Lactate dehydrogenase (LDH)
Lactate dehydrogenase (LDH) is an intracellular glycolytic enzyme that is involved in the reversible conversion of lactate to pyruvate and is found in most tissues of the body.
Research method
UV kinetic test.
Units
U/L (unit per liter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Do not eat for 12 hours before the test.
- Avoid physical and emotional stress 30 minutes before the test.
- Do not smoke for 30 minutes before donating blood.
General information about the study
Lactate dehydrogenase (LDH) is a zinc-containing intracellular enzyme that catalyzes the oxidation of lactic acid to pyruvate. LDH is most active in skeletal muscle, cardiac muscle, kidneys, liver and red blood cells.
There are five different forms (isoenzymes) of LDH, which differ in molecular structure and location in the body.
In diseases accompanied by tissue damage and cell destruction, LDH activity in the blood increases. In this regard, it is an important marker of tissue destruction. Despite the fact that an increase in enzyme activity does not indicate a specific disease, its determination in combination with other laboratory tests helps in the diagnosis of pulmonary infarction, muscular dystrophy and hemolytic anemia. Increased LDH activity can be detected in newborns, pregnant women and after intense physical exercise. for dynamic monitoring of cancer patients.
What is the research used for?
- To diagnose acute or chronic tissue damage during a comprehensive examination of the patient.
- For differential diagnosis of diseases with severe pain in the chest (myocardial infarction, angina, pulmonary infarction).
- To identify diseases accompanied by hemolysis of red blood cells.
- To monitor the course of cancer during therapy.
- For the study of liver and kidney pathologies.
- For diagnosing muscle tissue lesions.
What do the results mean?
| Age, gender | Reference values |
| 6 – 12 years | |
| 12 - 17 years old | |
| > 17 years old, female | 135 - 214 U/l |
| > 17 years old, male | 135 - 225 U/l |
Reasons for increased activity of general lactate dehydrogenase:
- myocardial infarction,
- pulmonary embolism and pulmonary infarction,
- blood diseases accompanied by hemolysis,
- malignant neoplasms of various localizations,
- leukemia,
- liver pathology,
- kidney disease (kidney infarction, glomerulonephritis, pyelonephritis),
- muscle pathology (muscular dystrophy, injury, atrophy),
- bone fractures,
- congestive heart failure, acute coronary failure,
- Infectious mononucleosis,
- intestinal infarction,
- acute pancreatitis,
- stroke,
- convulsive seizure,
- traumatic shock,
- severe conditions accompanied by hypoxia, hyper- and hypothermia,
- burn disease,
- hypothyroidism
Important Notes
Due to the non-specificity of this analysis, its result should be interpreted taking into account the indicators of other laboratory tests and the clinical picture of the disease.